Abstract
Background
Preoperative nutritional status is considered to affect the short-term and long-term outcomes of cancer patients. The clinical value of the controlling nutritional status (CONUT) score in elderly patients undergoing gastrectomy for gastric cancer remains unknown.
Methods
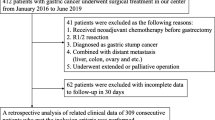
This study reviewed 211 elderly patients aged 75 years or over who underwent curative resection for gastric cancer from 2000 to 2015. Patients were grouped according to the preoperative CONUT score into those with normal nutrition (75 patients), light malnutrition (100 patients) and moderate or severe malnutrition (36 patients). The predictive value of the CONUT score for postoperative morbidity and survival was assessed.
Results
Impaired nutrition was associated with cardiovascular disease (P = 0.012) and chronic kidney disease (P = 0.014), and worsened malnutrition was linked to advanced age (P = 0.004), decreased body mass index (P = 0.008) and advanced disease stage (P = 0.01). Multivariate analysis showed the CONUT score as an independent predictor of procedure-unrelated infectious morbidity (odds ratio, 2.36; 95% confidence interval [CI], 0.99–5.40; P = 0.046). Patients with a higher CONUT score had significantly shorter overall survival in both stage I and stage II/III gastric cancer (P = 0.044 and P = 0.007, respectively) and reduced cancer-specific survival in stage II/III (P = 0.003) The CONUT score was a strong predictors of overall survival (hazard ratio [HR], 2.12; 95% CI, 1.18–3.69; P = 0.012) and cancer-specific survival (HR, 3.75; 95% CI, 1.30–10.43; P = 0.015) independent of disease stage.
Conclusions
The preoperative CONUT score is a simple and promising predictor of postoperative procedure-unrelated infectious morbidity and prognosis in elderly gastric cancer patients.


Similar content being viewed by others
References
Cutsem EV, Sagaert X, Topal B et al (2016) Gastric cancer. Lancet 388:2654–2664
Cancer Information Survice CANCER STATISTICS in JAPAN http://ganjoho.jp/en/professional/statistics/brochure/index.html
Takeuchi D, Koide N, Suzuki A et al (2015) Postoperative complications in elderly patients with gastric cancer. J Surg Res 198:317–326
Suzuki S, Kanaji S, Matsuda Y et al (2017) Long-term impact of postoperative pneumonia after curative gastrectomy for elderly gastric cancer patients. Ann Gatroenterol Surg 2:72–78
Damhuis RA, Tilanus HW (1995) The influence of age on resection rates and postoperative mortality in 2773 patients with gastric cancer. Eur J Cancer 31A:928–931
Kitamura K, Sugimachi K, Saku M (1999) Evaluation of surgical treatment for patients with gastric cancer who are over 80 years of age. Hepatogastroenterology 46:2074–2080
Kanda M, Mizuno A, Tanaka C et al (2016) Nutritional predictors for postoperative short-term and long-term outcomes of patients with gastric cancer. Medicine 95:e3781
Song GM, Tian X, Liang H et al (2015) Role of enteral immunonutrition in patients undergoing surgery for gastric cancer. Medicine 94:e1311
Ahmed T, Haboubi N (2010) Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging 5:207–216
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG et al (2005) CONUT score: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
Iwasaki I, Nagai T, Furukawa TA et al (2017) Prognostic value of malnutrition assessed by controlling nutritional status score for long-term mortality in patients with acute heart failure. Int J Cardiol 230:529–536
Fukushima K, Ueno Y, Kawagishi N et al (2011) The nutritional index ‘CONUT’ is useful for predicting long-term prognosis of patients with end-stage liver disease. Tohoku J Exp Med 224:215–219
Iseki Y, Shibutani M, Maeda K et al (2015) Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS ONE 10:e0132488
Hirahara N, Matsubara T, Hayashi H et al (2016) Prognostic importance of controlling nutritional status in patients undergoing curative thoracoscopic esophagectomy for esophageal cancer. Am J Ther. https://doi.org/10.1097/mut.0000000000000414
Shoji F, Haratake N, Akamine T et al (2017) The preoperative controlling nutritional status score predicts survival after curative surgery in patients with pathological stage I non-small cell lung cancer. Anticancer Res 37:741–747
Yoshida N, Baba Y, Shigaki H et al (2016) Preoperative nutritional assessment by controlling nutritional status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg 40:1910–1917. https://doi.org/10.1007/s00268-016-3549-3
Yoshida N, Harada K, Baba Y et al (2017) Preoperative controlling nutritional status (CONUT) is useful to estimate the prognosis after esophagectomy for esophageal cancer. Langenbecks Arch Surg 402:333–341
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma, 3rd English edition. Gastric Cancer 14:101–112
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–19
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Tokunaga M, Tanizawa Y, Bando E et al (2013) Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol 20:1575–1583
Hayashi T, Yoshikawa T, Aoyama T et al (2015) Impact of infectious complications on gastric cancer recurrence. Gastric Cancer 18:368–374
Hu WH, Cajas-Monson LC, Eisenstein S et al (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: as analysis of ACS-NSQIP. Nutr J. https://doi.org/10.1186/s12937-015-0081-5
Sakurai K, Ohira M, Tamura T et al (2016) Predictive potential of preoperative nutritional status in long-term outcome projections for patients with gastric cancer. Ann Surg Oncol 23:525–533
McMilan DC, Elahi MM, Sattar N et al (2001) Measurement of the systemic inflammation response predicts cancer-specific and non-cancer survival in patients with cancer. Nutr Cancer 41:64–69
Crumley ABC, Stuart RC, McKeranan M et al (2010) Is Hypoalbuminemia an independent prognostic factor in patients with gastric cancer? World J Surg 34:2393–2398. https://doi.org/10.1007/s00268-010-0641-y
Kuzuya M, Izawa S, Enoki H et al (2007) Is serum albumin a good marker for malnutrition in the physically impaired elderly? Clin Nutr 26:84–90
Hoffmann TK, Dworacki G, Tsukihiro T et al (2002) Spontaneuos apotosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res 8:2553–2562
Strasak AM, Pfeiffer RM, Brant LJ et al (2009) Time-dependent association of total serum cholesterol and cancer incidence in a cohort of 172210 men and women: a prospective 19-year follow-up study. Ann Oncol 20:1113–1120
Wang Q, Lau WY, Zhang B et al (2016) Preoperative total cholesterol predicts postoperative outcomes after partial hepatectomy in patients with chronic hepatitis B- or C-related hepatocellular carcinoma. Surgery 155:263–270
Cengiz O, Kocer B, Süemeil S et al (2006) Are pretreatment serum albumin and cholesterol levels prognostic tools in patients with colorectal carcinoma? Med Sci Monit 12:CR240–CR247
Toyokawa T, Kubo N, Tamura T et al (2016) The pretreatment controlling nutritional status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: results from a retrospective study. BMC Cancer 16:722–732
Makary MA, Segev DL, Pronovost PJ et al (2010) Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 210:901–908
Revenig LM, Canter DJ, Taylor MD et al (2013) Too frail for surgery? initial results of a large multidisciplinary prospective study examining preoperative variables predictive of poor surgical outcomes. J Am Coll Surg 217:665–670
Nashimoto A (2013) Current status of treatment strategy for elderly patients with gastric cancer. Int J Clin Oncol 18:969–970
Weimann A, Braga M, Carli F et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36:623–650
Jie B, Jiang ZM, Nolan MT et al (2012) Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 28:1022–2017
Mazaki T, Ishii Y, Murai I (2015) Immunoenhancing enteral and parental nutrition for gastrointestinal surgery a multiple-treatments meta-analysis. Ann Surg 261:662–669
MortensenK Nilsson M, Slim L et al (2014) Consensus guidelines for enhanced recovery after gastrectomy: enhanced recovery after surgery (ERAS(R)) society recommendations. Br J Surg 101:1209–1229
Tanaka R, Lee SW, Kawai M et al (2017) Protocol for enhanced recovery after surgery improves short-term outcomes for patients with gastric cancer: a randomized clinical trial. Gastric Cancer 20:861–871
Morgan J, Guinan E, McCormic P et al (2014) The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systemic review and meta-analysis. Surgery 155:124–133
Silver JK, Baima J (2013) Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil 92:715–727
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, S., Kanaji, S., Yamamoto, M. et al. Controlling Nutritional Status (CONUT) Score Predicts Outcomes of Curative Resection for Gastric Cancer in the Elderly. World J Surg 43, 1076–1084 (2019). https://doi.org/10.1007/s00268-018-04889-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-04889-6