Abstract
Abstract
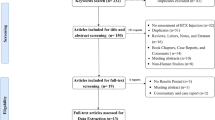
Botulinum toxin-A (BTX-A), a neurotoxin produced by Clostridium botulinum, was assessed for relieving implant-related pectoralis major muscle’s painful spasms. In detail, 100 units of BTX-A can reduce muscle activity and, as a consequence, muscle spasms. The latter is considered the leading cause of post-operative pain after the sub-pectoral tissue expansion, sometimes leading to early expanders’ removal. In addition, women choosing post-mastectomy reconstruction surgery seem to suffer worse post-operative pain than those who stop at the mastectomy stage. However, there is no unanimous consensus concerning the potential benefits of BTX-A in reducing pain related to the sub-pectoral placement of tissue expanders in breast reconstruction due to the exiguity of evidence. Therefore, this review aims to describe BTX-A-related evidence in this reconstruction setting.
No Level Assigned
This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern Basic Science, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
References
Tao Z, Shi A, Lu C, Song T, Zhang Z, Zhao J (2015) Breast cancer: epidemiology and etiology. Cell Biochem Biophys 72:333–338
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, Zackrisson S, Senkus E (2019) ESMO guidelines committee (2019) early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol 30:1194–1220
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, Barrios CH, Bergh J, Bhattacharyya GS, Biganzoli L, Boyle F, Cardoso MJ, Carey LA, Cortés J, El Saghir NS, Elzayat M, Eniu A, Fallowfield L, Francis PA, Gelmon K, Gligorov J, Haidinger R, Harbeck N, Hu X, Kaufman B, Kaur R, Kiely BE, Kim SB, Lin NU, Mertz SA, Neciosup S, Offersen BV, Ohno S, Pagani O, Prat A, Penault-Llorca F, Rugo HS, Sledge GW, Thomssen C, Vorobiof DA, Wiseman T, Xu B, Norton L, Costa A, Winer EP (2020) 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol Off J Eur Soc Med Oncol 31:1623–1649
American Society of Plastic Surgeons (2013) Plastic surgery statistics report
Grella R, D’Andrea F, Nicoletti GF, Lanzano G (2022) Tuberous breast management: a review of literature and novel technique refinements. Plast Reconstr Surg Glob Open 10:e4708
Radovan C (1982) Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 69:195–208
Ferraro GA, Lanzano G, Gentile C, Izzo S, Grella E, Gubitosi A, Nicoletti GF (2021) The «Five-flap» technique for nipple-areola complex reconstruction. Plast Reconstr Surg Glob Open 9:e3917
Disa JJ, Ad-El DD, Cohen SM, Cordeiro PG, Hidalgo DA (1999) The premature removal of tissue expanders in breast reconstruction. Plast Reconstr Surg 104:1662–1665
Pusic AL, Cordeiro PG (2003) An accelerated approach to tissue expansion for breast reconstruction: experience with intraoperative and rapid postoperative expansion in 370 reconstructions. Plast Reconstr Surg 111:1871–1875
Rimareix F, Masson J, Couturaud B, Revol M, Servant JM (1999) Breast reconstruction by inflatable anatomical implant. Retrospective study of 65 cases. Ann Chir Plast Esthet 44:239–245
Ferraro GA, Lanzano G, Grella E, Gubitosi A, Nicoletti GF (2022) Successful treatment of wound dehiscence by innovative type 1 collagen flowable gel: a case report. Plast Reconstr Surg Glob Open 10:e4360
Dassoulas KR, Wang J, Thuman J, Ndem I, Schaeffer C, Stovall M, Tilt A, Lee A, Lin KY, Campbell CA (2018) Reducing infection rates in implant-based breast reconstruction: impact of an evidence-based protocol. Ann Plast Surg 80:493–499
Fischer JP, Wes AM, Nelson JA, Basta M, Rohrbach JI, Wu LC, Serletti JM, Kovach SJ (2014) Propensity-matched, longitudinal outcomes analysis of complications and cost: comparing abdominal free flaps and implant-based breast reconstruction. J Am Coll Surg 219:303–312
Malahias M, Jordan DJ, Hughes LC, Hindocha S, Juma A (2016) A literature review and summary of capsular contracture: an ongoing challenge to breast surgeons and their patients. Int J Surg Open. 3:1–7
Legeby M, Segerdahl M, Sandelin K, Wickman M, Östman K, Olofsson Ch (2002) Immediate reconstruction in breast cancer surgery requires intensive post-operative pain treatment but the effects of axillary dissection may be more predictive of chronic pain. The Breast 11:156–162
May JW, Bucky LP, Sohoni S, Ehrlich HP (1994) Smooth versus textured expander implants: a double-blind study of capsule quality and discomfort in simultaneous bilateral breast reconstruction patients. Ann Plast Surg 32:225–32
Raposio E, Santi PL (1999) Topical application of DMSO as an adjunct to tissue expansion for breast reconstruction. Br J Plast Surg 52:194–197
Sinow JD, Cunningham BL (1992) Intraluminal lidocaine for analgesia after tissue expansion: a double-blind prospective trial in breast reconstruction. Ann Plast Surg 28:320–325
Turan Z, Sandelin K (2006) Local infiltration of anaesthesia with subpectoral indwelling catheters after immediate breast reconstruction with implants: a pilot study. Scand J Plast Reconstr Surg Hand Surg 40:136–139
Lanzano G, Faenza M, Lanzano G, Izzo S, Ferraro GA, Nicoletti GF (2022) Absorbable Vs. non-absorbable sutures in plastic and dermatologic surgery procedures during the covid-19 pandemic: which would you prefer? J Cutan Aesthetic Surg. 15:202–203
Li T, Liu Y, Zhang W (2018) Botulinum toxin a plays an important role in the placement of implants deep within the pectoralis major muscle for mammaplasty: a systematic review and meta-analysis. Aesthetic Plast Surg 42:1519–1530
Boon AJ, Smith J, Dahm DL, Sorenson EJ, Larson DR, Fitz-Gibbon PD, Dykstra DD, Singh JA (2010) Efficacy of intra-articular botulinum toxin type A in painful knee osteoarthritis: a pilot study. PM R 2:268–76
Singh JA, Fitzgerald PM (2010) Botulinum toxin for shoulder pain. Cochrane Database Syst Rev 9:CD008271
Abbott J (2009) Gynecological indications for the use of botulinum toxin in women with chronic pelvic pain. Toxicon Off J Int Soc Toxinol 54:647–653
Guyuron B, Reed D, Kriegler JS, Davis J, Pashmini N, Amini S (2009) A placebo-controlled surgical trial of the treatment of migraine headaches. Plast Reconstr Surg 124:461–468
Babcock MS, Foster L, Pasquina P, Jabbari B (2005) Treatment of pain attributed to plantar fasciitis with botulinum toxin a: a short-term, randomized, placebo-controlled, double-blind study. Am J Phys Med Rehabil 84:649–654
Wong SM, Hui ACF, Tong PY, Poon DWF, Yu E, Wong LKS (2005) Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 143:793–797
Schwartz MS, Wren DR, Filshie J (1998) Neuromyotonia in a muscle flap producing a convulsing breast: successful treatment with botulinum toxin. Mov Disord Off J Mov Disord Soc. 13:188–190
Hoefflin SM (1998) Botox alternatives. Plast Reconstr Surg 101:865
Figus A, Mazzocchi M, Dessy LA, Curinga G, Scuderi N (2009) Treatment of muscular contraction deformities with botulinum toxin type A after latissimus dorsi flap and sub-pectoral implant breast reconstruction. J Plast Reconstr Aesthetic Surg JPRAS. 62:869–75
Richards A, Ritz M, Donahoe S, Southwick G (2001) Botox for contraction of pectoral muscles. Plast Reconstr Surg 108:270–271
Senior MA, Fourie LR (2000) Botox and the management of pectoral spasm after subpectoral implant insertion. Plast Reconstr Surg 106:224–225
Smith TJ, Hill KK, Raphael BH (2005) Historical and current perspectives on Clostridium botulinum diversity. Res Microbiol 166:290–302
Rossetto O, Pirazzini M, Montecucco C (2014) Botulinum neurotoxins: genetic, structural and mechanistic insights. Nat Rev Microbiol 12:535–549
Rummel A (2015) The long journey of botulinum neurotoxins into the synapse. Toxicon Off J Int Soc Toxinol 107:9–24
Jankovic J (1994) Botulinum toxin in the treatment of dystonic tics. Mov Disord Off J Mov Disord Soc. 9:347–349
Albanese A, Lalli S (2009) Is this dystonia? Mov Disord Off J Mov Disord Soc. 24:1725–1731
Albanese A, Lalli S (2012) Update on dystonia. Curr Opin Neurol 25:483–490
Jackson JL, Kuriyama A, Hayashino Y (2012) Botulinum toxin A for prophylactic treatment of migraine and tension headaches in adults: a meta-analysis. JAMA 307:1736–45
Buonocore M, Demartini L, Mandrini S, Dall’Angelo A, Dalla Toffola E (2017) Effect of botulinum toxin on disabling neuropathic pain: a case presentation suggesting a new therapeutic strategy. PM R. 9:200–3
Guo Y, Lu Y, Liu T, Zhou Y, Yang P, Zhu J, Chen L, Yang Q (2015) Efficacy and safety of botulinum toxin type A in the treatment of glabellar lines: a meta-analysis of randomized, placebo-controlled, double-blind trials. Plast Reconstr Surg 136:310e-e318
Veronesi P, Ballardini B, De Lorenzi F, Magnoni F, Lissidini G, Caldarella P, Galimberti V (2011) Immediate breast reconstruction after mastectomy. Breast Edinb Scotl 20(Suppl 3):S104-107
Ward J, Cohen IK, Knaysi GA, Brown PW (1987) Immediate breast reconstruction with tissue expansion. Plast Reconstr Surg 80:559–566
Scott AB (1980) Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology 87:1044–1049
Münchau A, Bhatia KP (2000) Uses of botulinum toxin injection in medicine today. BMJ 320:161–165
Matak I, Bölcskei K, Bach-Rojecky L, Helyes Z (2019) Mechanisms of Botulinum Toxin Type A Action on Pain. Toxins 11:459
Layeeque R, Hochberg J, Siegel E, Kunkel K, Kepple J, Henry-Tillman RS, Dunlap M, Seibert J, Klimberg VS (2004) Botulinum toxin infiltration for pain control after mastectomy and expander reconstruction. Ann Surg 240:608–13
Gabriel A, Champaneria MC, Maxwell GP (2015) The efficacy of botulinum toxin A in post- mastectomy breast reconstruction: a pilot study. Aesthet Surg J 35:402–409
O’Donnell CJ (2011) Pectoral muscle spasms after mastectomy successfully treated with botulinum toxin injections. PM R 3:781–782
Lo KK, Aycock JK (2015) A blinded randomized controlled trial to evaluate the use of botulinum toxin for pain control in breast reconstruction with tissue expanders. Ann Plast Surg 74:281–283
Lemaine V, Lohse CM, Mandrekar JN, Ramaker SA, Convery PA, Nguyen MD, Tran NV (2020) Botulinum toxin a in tissue expander breast reconstruction: a double-blinded randomized controlled trial. Plast Reconstr Surg Glob Open 8:e3030
Winocour S, Murad MH, Bidgoli-Moghaddam M, Jacobson SR, Bite U, Saint-Cyr M, Tran NV, Lemaine V (2014) A systematic review of the use of Botulinum toxin type A with subpectoral breast implants. J Plast Reconstr Aesthetic Surg JPRAS. 67:34–41
Acknowledgement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferraro, G.A., Mattiello, S., Natriello, A. et al. Botulinum Toxin-A Infiltration to Control Post-Operative Pain after Mastectomy and Expander Reconstruction as Potentially Useful Tool: A Narrative Review. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-04034-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00266-024-04034-w