Abstract
Objective
To assess the accuracy of an artificial intelligence (AI) software (BoneMetrics, Gleamer) in performing automated measurements on weight-bearing forefoot and lateral foot radiographs.
Methods
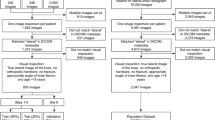
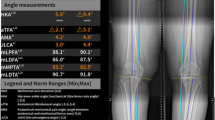
Consecutive forefoot and lateral foot radiographs were retrospectively collected from three imaging institutions. Two senior musculoskeletal radiologists independently annotated key points to measure the hallux valgus, first–second metatarsal, and first–fifth metatarsal angles on forefoot radiographs and the talus–first metatarsal, medial arch, and calcaneus inclination angles on lateral foot radiographs. The ground truth was defined as the mean of their measurements. Statistical analysis included mean absolute error (MAE), bias assessed with Bland–Altman analysis between the ground truth and AI prediction, and intraclass coefficient (ICC) between the manual ratings.
Results
Eighty forefoot radiographs were included (53 ± 17 years, 50 women), and 26 were excluded. Ninety-seven lateral foot radiographs were included (51 ± 20 years, 46 women), and 21 were excluded. MAE for the hallux valgus, first–second metatarsal, and first–fifth metatarsal angles on forefoot radiographs were respectively 1.2° (95% CI [1; 1.4], bias = − 0.04°, ICC = 0.98), 0.7° (95% CI [0.6; 0.9], bias = − 0.19°, ICC = 0.91) and 0.9° (95% CI [0.7; 1.1], bias = 0.44°, ICC = 0.96). MAE for the talus–first, medial arch, and calcaneal inclination angles on the lateral foot radiographs were respectively 3.9° (95% CI [3.4; 4.5], bias = 0.61° ICC = 0.88), 1.5° (95% CI [1.2; 1.8], bias = − 0.18°, ICC = 0.95) and 1° (95% CI [0.8; 1.2], bias = 0.74°, ICC = 0.99). Bias and MAE between the ground truth and the AI prediction were low across all measurements. ICC between the two manual ratings was excellent, except for the talus–first metatarsal angle.
Conclusion
AI demonstrated potential for accurate and automated measurements on weight-bearing forefoot and lateral foot radiographs.






Similar content being viewed by others
Data availability
The dataset used and analyzed for the current study is available from the corresponding author upon reasonable request. The dataset used for develo** the AI model, as well as the AI model itself, are components of proprietary software and are therefore not publicly available.
Abbreviations
- AI:
-
Artificial intelligence
- MSK:
-
Musculoskeletal
- MAE:
-
Mean absolute error
- ICC:
-
Intraclass coefficient
References
Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:1–9.
Saltzman CL, Nawoczenski DA, Talbot KD. Measurement of the medial longitudinal arch. Arch Phys Med Rehabil. 1995;76(1):45–9.
Resch S, Ryd L, Stenström A, Johnsson K, Reynisson K. Measuring hallux valgus: a comparison of conventional radiography and clinical parameters with regard to measurement accuracy. Foot Ankle Int. 1995;16(5):267–70.
Gupta P, Kingston KA, O’Malley M, Williams RJ, Ramkumar PN. Advancements in artificial intelligence for foot and ankle surgery: a systematic review. Foot Ankle Orthopaedics. 2023;8(1):24730114221151080.
van Leeuwen KG, Schalekamp S, Rutten MJ, van Ginneken B, de Rooij M. Artificial intelligence in radiology: 100 commercially available products and their scientific evidence. Eur Radiol. 2021;31:3797–804.
Regnard NE, Lanseur B, Ventre J, et al. Assessment of performances of a deep learning algorithm for the detection of limbs and pelvic fractures, dislocations, focal bone lesions, and elbow effusions on trauma X-rays. Eur J Radiol. 2022;154:110447.
Canoni-Meynet L, Verdot P, Danner A, et al. Added value of an artificial intelligence solution for fracture detection in the radiologist’s daily trauma emergencies workflow. Diagn Interv Imaging. 2022;103:594–600.
Duron L, Ducarouge A, Gillibert A, et al. Assessment of an AI aid in detection of adult appendicular skeletal fractures by emergency physicians and radiologists: a multicenter cross-sectional diagnostic study. Radiology. 2021;300(1):120–9.
Guermazi A, Tannoury C, Kompel AJ, et al. Improving radiographic fracture recognition performance and efficiency using artificial intelligence. Radiology. 2022;302(3):627–36.
Hayashi D, Kompel AJ, Ventre J, et al. Automated detection of acute appendicular skeletal fractures in pediatric patients using deep learning. Skeletal Radiol. 2022;51(11):2129–39.
Dallora AL, Anderberg P, Kvist O, Mendes E, Diaz Ruiz S, Sanmartin BJ. Bone age assessment with various machine learning techniques: a systematic literature review and meta-analysis. PLoS ONE. 2019;14(7):e0220242.
Nguyen T, Hermann AL, Ventre J, Ducarouge A, Pourchot A, Marty V, Regnard NE, Guermazi A. High performance for bone age estimation with an artificial intelligence solution. Diagn Interv Imaging. 2023;104(7–8):330–6.
Jensen J, Graumann O, Overgaard S, Gerke O, Lundemann M, Haubro MH, Varnum C, Bak L, Rasmussen J, Olsen LB, Rasmussen BSB. A deep learning algorithm for radiographic measurements of the hip in adults—a reliability and agreement study. Diagnostics. 2022;12(11):2597.
Stotter C, Klestil T, Röder C, Reuter P, Chen K, Emprechtinger R, Hummer A, Salzlechner C, DiFranco M, Nehrer S. Deep learning for fully automated radiographic measurements of the pelvis and hip. Diagnostics. 2023;13(3):497.
Simon S, Schwarz GM, Aichmair A, Frank BJH, Hummer A, DiFranco MD, Dominkus M, Hofstaetter JG. Fully automated deep learning for knee alignment assessment in lower extremity radiographs: a cross-sectional diagnostic study. Skeletal Radiol. 2022;51(6):1249–59. https://doi.org/10.1007/s00256-021-03948-9.
Pei Y, Yang W, Wei S, Cai R, Li J, Guo S. Automated measurement of hip–knee–ankle angle on the unilateral lower limb X-rays using deep learning. Phys Eng Sci Med. 2021;44:53–62.
Archer H, Reine S, **a S, et al. Deep learning generated lower extremity radiographic measurements are adequate for quick assessment of knee angular alignment and leg length determination. Skeletal Radiol. 2023;53(5):923–33.
Pan Y, Chen Q, Chen T, et al. Evaluation of a computer-aided method for measuring the Cobb angle on chest X-rays. Eur Spine J. 2019;28:3035–43.
Wu C, Meng G, Lian J, et al. A multi-stage ensemble network system to diagnose adolescent idiopathic scoliosis. Eur Radiol. 2022;32(9):5880–9.
Yang CH, Chou KT, Chung MB, Chuang KS, Huang TC. Automatic detection of calcaneal-fifth metatarsal angle using radiograph: a computer-aided diagnosis of flat foot for military new recruits in Taiwan. PLoS ONE. 2015;10(6):e0131387.
Li T, Wang Y, Qu Y, Dong R, Kang M, Zhao J. Feasibility study of hallux valgus measurement with a deep convolutional neural network based on landmark detection. Skeletal Radiol. 2022;51(6):1235–47. https://doi.org/10.1007/s00256-021-03939-w.
Kao EF, Lu CY, Wang CY, Yeh WC, Hsia PK. Fully automated determination of arch angle on weight-bearing foot radiograph. Comput Methods Programs Biomed. 2018;154:79–88.
Benchoufi M, Matzner-Lober E, Molinari N, Jannot AS, Soyer P. Interobserver agreement issues in radiology. Diagn Interv Imaging. 2020;101(10):639–41.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63.
Nery C, Coughlin MJ, Baumfeld D, Ballerini FJ, Kobata S. Hallux valgus in males–part 1: demographics, etiology, and comparative radiology. Foot Ankle Int. 2013;34(5):629–35. https://doi.org/10.1177/1071100713475350.
Funding
This study was funded by Gleamer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LL, NER, JV, VM, LC, ZZ, NN, and JDL are employees of Gleamer. AG is shareholder of BICL, LLC, and consultant to Pfizer, Novartis, TrialSpark, Coval, ICM, Medipost, and TissueGene.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lassalle, L., Regnard, Ne., Ventre, J. et al. Automated weight-bearing foot measurements using an artificial intelligence–based software. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04726-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04726-z