Abstract
Pulmonary nodules present a diagnostic challenge when they appear as atypical metastases in pediatric oncology patients. Chest computed tomography (CT) is the primary imaging modality for assessing lung nodules. In pediatric populations, Wilms tumor and osteosarcoma are the cancers most likely to produce pulmonary metastasis, both typical and atypical. This pictorial essay provides a thorough description of the specific radiologic features of atypical pediatric pulmonary metastases, and their pathogenesis and differential diagnosis. We also address diagnostic approaches to incidental lung nodules in healthy children found in the literature. Our aim is to help radiologists identify atypical lung metastases on CT, ensuring that children receive prompt, and potentially lifesaving, treatment.











Similar content being viewed by others
References
Dishop MK, Kuruvilla S (2008) Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children’s hospital. Arch Pathol Lab Med 132:1079–1103
Roik D, Mosior T, Sopyło B et al (2010) Abscess mimicking lung metastasis in a 10-year-old boy – case report. Pol J Radiol 75:55–57
Durnali AG, Turkoz FP, Yukruk FA et al (2016) Outcomes of adolescent and adult patients with lung metastatic osteosarcoma and comparison of synchronous and metachronous lung metastatic groups. PLoS One 11:e0152621
Seo JB, Im JG, Chung MJ et al (2001) Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics 21:403–417
Arkoudis N-A, Pastroma A, Velonakis G et al (2019) Solitary round pulmonary lesions in the pediatric population: a pictorial review. Acta Radiol Open 8:2058460119851998
Cohen MC, Kaschula RO (1992) Primary pulmonary tumors in childhood: a review of 31 years’ experience and the literature. Pediatr Pulmonol 140:222–232
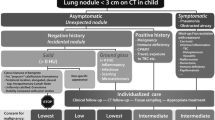
Westra SJ, Brody AS, Mahani MG et al (2015) The incidental pulmonary nodule in a child: part 1: recommendations from the SPR thoracic imaging committee regarding characterization, significance and follow-up. Pediatr Radiol 45:628–633
Westra SJ, Thacker PG, Podberesky DJ et al (2015) The incidental pulmonary nodule in a child: part 2: commentary and suggestions for clinical management, risk communication and prevention. Pediatr Radiol 45:634–639
Brillantino C, Rossi E, Minelli R et al (2019) Current role of imaging in the management of children with Wilms tumor according to the new UMBRELLA protocol. Transl Med 8:1–16
Voss SD, Reaman GH, Kaste SC, Slovis TL (2009) The ALARA concept in pediatric oncology. Pediatr Radiol 39:1142–1146
Lell MM, May M, Deak P et al (2011) High-pitch spiral computed tomography: effect on image quality and radiation dose in pediatric chest computed tomography. Investig Radiol 46:116–123
Renne J, Linderkamp C, Wacker F et al (2015) Prevalence and configuration of pulmonary nodules on multi-row CT in children without malignant diseases. Eur Radiol 25:2651–2656
Samim A, Littooij AS, van den Heuvel-Eibrink MM et al (2017) Frequency and characteristics of pulmonary nodules in children at computed tomography. Pediatr Radiol 47:1751–1758
Alves GRT, Marchiori E, Irion KL et al (2015) Mediastinal lymph nodes and pulmonary nodules in children: MDCT findings in a cohort of healthy subjects. AJR Am J Roentgenol 204:35–37
Meyer JS, Nadel HR, Marina N et al (2008) Imaging guidelines for children with Ewing sarcoma and osteosarcoma: a report from the children’s oncology group bone tumor committee. Pediatr Blood Cancer 51:163–170
Briccoli A, Rocca M, Salone MC et al (2009) “Bubble-like” lung metastases in osteosarcoma patients. Eur J Radiol 71:144–146
Rastogi R, Garg R, Thulkar S et al (2008) Unusual thoracic CT manifestations of osteosarcoma: review of 16 cases. Pediatr Radiol 38:551–558
Lee KC, Kang EY, Yong HS et al (2019) A stepwise diagnostic approach to cystic lung diseases for radiologists. Korean J Radiol 20:1368–1380
Kim NR, Han J (2012) Pathologic review of cystic and cavitary lung diseases. Korean J Pathol 46:407–414
Khan AN, Al-Jahdali HH, Allen CM et al (2010) The calcified lung nodule: what does it mean? Ann Thorac Med 5:67–79
Interiano RB, McCarville MB, Wu J et al (2015) Pneumothorax as a complication of combination antiangiogenic therapy in children and young adults with refractory/recurrent solid tumors. J Pediatr Surg 50:1484–1489
Lucaya J, Coma A (2014) High-resolution CT of the lung in children: technique, indications, anatomy, and features of lung disease. In: Gracia-Pena P, Guillerman RP (eds) Pediatric chest imaging, 3rd edn. Springer, New York, pp 111–134
Madafferi S, Catania VD, Accinni A et al (2015) Endobronchial tumor in children: unusual finding in recurrent pneumonia, report of three cases. World J Clin Pediatr 4:30–34
Roby BB, Drehner D, Sidman JD (2011) Pediatric tracheal and endobronchial tumors: an institutional experience. Arch Otolaryngol Head Neck Surg 137:925–929
Mazboudi O, Abboud MR, Muwakkit S et al (2010) Endobronchial metastasis of osteosarcoma presenting as position-dependent and variable airway obstruction of the trachea. Thorax 65:92
Latchana N, Daniel VC, Gould RW, Pollock RE (2017) Pulmonary tumor embolism secondary to soft tissue and bone sarcomas: a case report and literature review. World J Surg Oncol 15:168
Badia JGS, Caravajal JMG, Larruga BV et al (2007) [Pneumonectomy with extracorporeal circulation to treat pulmonary metastasis.] Arch Bronconeumol 43:180–182
Yedururi S, Morani AC, Gladish GW et al (2016) Cardiovascular involvement by osteosarcoma: an analysis of 20 patients. Pediatr Radiol 46:21–33
Kumar N, Price LC, Montero MA et al (2015) Pulmonary tumour thrombotic microangiopathy: unclassifiable pulmonary hypertension? Eur Respir J 46:1214–1217
Price LC, Wells AU, Wort SJ (2016) Pulmonary tumour thrombotic microangiopathy. Curr Opin Pulm Med 22:421–428
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scolnik, M., Glozman, L., Bar-Yoseph, R. et al. Atypical pulmonary metastases in children: the spectrum of radiologic findings. Pediatr Radiol 51, 1907–1916 (2021). https://doi.org/10.1007/s00247-021-05035-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05035-6