Abstract
Background
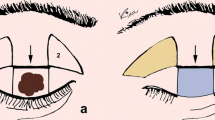
Large full-thickness lower eyelid defects are repaired by “one- or two-step” flap-flap or flap-graft combinations. I present the long-term surgical outcome of a novel “one-step” closure of full-thickness lower eyelid defects by using two autografts for the reconstruction of the anterior and posterior lamellas following malignant tumor removal.
Methods
Non-comparative case series of lower eyelid reconstructions were performed by a single surgeon between 2003 and 2020. Horizontal and vertical lengths of eyelid defects were measured. The required autografts were chosen from the ipsi-contralateral upper eyelid. Surgical success was defined as the achievement of satisfactory lower eyelid anatomy with the best esthetic and functional outcomes without needing further interventions.
Results
Thirty-nine lower eyelids (21 right,18 left) of 39 patients (25 men, 14 women) with a mean age of 65.2 ± 8.1 years (53–85) had reconstructive surgery by this method after malignant tumor resection. Eyelid defects involved more than 50% of their horizontal lengths with a mean size of 18.3 ± 2.8 mm horizontally and 8.7 ± 2.3 mm vertically. The mean follow-up time was 36.5 ± 12.3 months (3–58). Functional and esthetic outcomes were excellent or good in all cases and no patient needed additional interventions in the repaired area or demonstrated graft rejection. Postoperative complications were graft edema (n = 15), ecchymosis (n = 9), eyelid margin thinning (n = 3), mild lagophthalmos (n = 1), eyelid contour irregularity (n = 1), retraction (n = 1), and granuloma formation (n = 1).
Conclusions
“One-step” reconstruction of large full-thickness lower eyelid defects using two autografts seems to be effective, simple, and practical for the repair of the anterior and posterior lid lamellas with good esthetic and functional long-term results.
Level of evidence: Level IV, therapeutic study.





Similar content being viewed by others
References
Hughes WL (1937) A new method for rebuilding a lower lid: report of a case. Arch Ophthalmol 17:1008–1017
Zaky AD, Elmazar HMF, Elaziz MS (2016) Longevity results of modified Hughes procedure in reconstructing large lower eyelid defects. Clin Ophtahlmol 10:1825–1828
Hishmi AM, Koch KR, Matthaei M, Bölke E, Cursiefen C, Heindl LM (2016) Modified Hughes procedure for reconstruction of large full-thickness lower eyelid defects following tumor resection. Eur J Med Res 21:27
Leibsohn JM, Dryden R, Ross J (1993) Intentional buttonholing of the Hughes’ flap. Ophthal Plast Reconstr Surg 9:135–138
Bartley GB, Messenger MM (2002) Outcome of tarsoconjunctival flap dehiscence after eyelid reconstruction. Am J Ophthalmol 134:627–630
McNab AA, Martin P, Benger R, O’Donnel B, Kourt G (2001) A prospective randomized study comparing division of the pedicle of modified 1s flaps at two or four weeks. Ophthalmic Plast Reconstr Surg 17:317–319
Leibovitch I, Selva D (2004) Modified Hughes flap: division at 7 days. Ophthalmology 111:2164–2167
Memarzadeh K, Gustafsson L, Blohmé J, Malmsjö M (2016) Evaluation of the microvascular blood flow, oxygenation, and survival of tarsoconjunctival flaps following the modified Hughes procedure. Ophthalmic Plast Reconstr Surg 32:468–472
Mustarde JC (1966) Repair and reconstruction in the orbital region: a practical guide. Livingstone, Edinburgh, pp 126–133
Hargiss JL (1989) Bipedicle tarsoconjunctival flap. Ophthalmic Plast Reconstr Surg 5:99–103
Katz TL, Pennington TE, Yohendran J, Ghabrial R (2014) One-step reconstruction of large lower eyelid defects: technique and outcomes. Clin Exp Ophthalmol 42:889–892
Skippen B, Hamilton A, Evans S, Benger R (2016) One-stage alternatives to the Hughes procedure for reconstruction of large lower eyelid defects: surgical techniques and outcomes. Ophthalmic Plast Reconstr Surg 32:145–149
Hawes MJ (1987) Free autogenous grafts in eyelid tarsoconjunctival reconstruction. Ophthalmic Surg 18:37–41
Hawes MJ, Grove AS Jr, Hink EM (2011) Comparison of free tarsoconjunctival grafts and Hughes tarsoconjunctival grafts for lower eyelid reconstruction. Ophthalmic Plast Reconstr Surg 27:219–223
Boboridis KG (2005) Modified Hughes flap. Ophthalmology 112:2239–2240; author reply 2240–2241
Paridaens D, van den Bosch WA (2008) Orbicularis muscle advancement flap combined with free posterior and anterior lamellar grafts: a 1-stage sandwich technique for eyelid reconstruction. Ophthalmology 115:189–194
Hafez A (2010) Reconstruction of large upper eyelid defect with two composite lid margin grafts. Middle East Afr J Ophthalmol 17:161–164
Emesz M, Krall E, Nischler C, Rasp M, Dexl AK, Bauer F et al (2014) Hughes’ operation and combined procedures. Ophthalmologe 111:448–453
Funding
The author declares that no funds, grants, or other supports were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of the University of Erciyes approved this study (approval number: 2022/80).
Consent to participate
Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Conflict of interest
Cem Evereklioglu declares no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Evereklioglu, C. A novel one-step repair of large lower eyelid defects following tumor resection in adults: surgical technique and outcome. Eur J Plast Surg 45, 925–932 (2022). https://doi.org/10.1007/s00238-022-01970-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-022-01970-1