Abstract
Background
This study aimed to analyze the factors influencing warfarin-related major gastrointestinal bleeding (GIB) and to develop a score that would provide a reference for assessing the risk of major GIB associated with warfarin treatment.
Methods
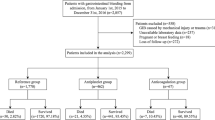
This was a retrospective analysis of clinical and follow-up data from warfarin-treated patients. Scores were analyzed using logistic regression. The area under the subject working characteristic curve (AUC), sensitivity, specificity, and Hosmer-Lemeshow test were used to evaluate the scoring performance.
Results
A total of 1591 patients who met the requirements for warfarin use were included in this study, and 46 developed major GIB. After univariate analysis as well as multivariate logistic regression analysis, nine factors were found to be associated with increased risk of major GIB, namely age ≥ 65 years, history of peptic ulcer, history of major bleeding, abnormal liver function, abnormal renal function, cancer, anemia, labile international normalized ratio, and combination of antiplatelet agents/non-steroidal anti-inflammatory drugs. The Alfalfa-Warfarin-GIB score was constructed using these nine factors. The AUC and Bootstrap method-corrected AUC of the Alfalfa-Warfarin-GIB score were 0.916 (95% CI: 0.862–0.970, P < 0.001) and 0.919 (95% CI: 0.860–0.967, P < 0.001), respectively, which were higher than those of the HAS-BLED score (AUC = 0.868, 95% CI: 0.812–0.924, P < 0.001).
Conclusion
Based on nine risk factors, the Alfalfa-Warfarin-GIB score was constructed to predict the risk of warfarin-related major GIB. The newly developed Alfalfa-Warfarin-GIB score has a better predictive value than the HAS-BLED score and may be an effective tool to help reduce the occurrence of major GIB in patients on warfarin.




Similar content being viewed by others
Availability of data and material
The data presented in this study are available on request from the corresponding author.
References
Gu ZC, Wei AH, Zhang C et al (2020) Risk of Major Gastrointestinal Bleeding With New vs Conventional Oral Anticoagulants: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 18(4):792-799.e61
Chen WC, Chen YH, Hsu PI et al (2014) Gastrointestinal hemorrhage in warfarin anticoagulated patients: incidence, risk factor, management, and outcome. Biomed Res Int 2014:463767
Hirsh J, Fuster V, Ansell J et al (2003) American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. Circulation 107(12):1692–1711
Jacobs LG (2008) Warfarin pharmacology, clinical management, and evaluation of hemorrhagic risk for the elderly. Cardiol Clin 26(2):157–67
Sun Y (2013) Chinese expert consensus on warfarin anticoagulant therapy. Chinese J Int Med 01:76–82
Rubin TA, Murdoch M, Nelson DB (2003) Acute GI bleeding in the setting of supratherapeutic international normalized ratio in patients taking warfarin: endoscopic diagnosis, clinical management, and outcomes. Gastrointest Endosc 58(3):369–373
Di Minno A, Spadarella G, Spadarella E et al (2015) Gastrointestinal bleeding in patients receiving oral anticoagulation: Current treatment and pharmacological perspectives. Thromb Res 136(6):1074–1081
Pisters R, Lane DA, Nieuwlaat R et al (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138(5):1093–1100
Gage BF, Yan Y, Milligan PE et al (2006) Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF). Am Heart J 151(3):713–719
Fang MC, Go AS, Chang Y et al (2011) A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study. J Am Coll Cardiol 58(4):395–401
Strate LL, Gralnek IM (2016) ACG clinical guideline: Management of patients with acute lower gastrointestinal bleeding. Am J Gastroenterol 111:459–474
Laine L, Jensen DM (2012) Management of patients with ulcer bleeding. Am J Gastroenterol 107:345,60; quiz 361
Shimomura A, Nagata N, Shimbo T et al (2018) New predictive model for acute gastrointestinal bleeding in patients taking oral anticoagulants: A cohort study. J Gastroenterol Hepatol 33(1):164–171
Lv M, Jiang S, Wu T, Huang N, Chen X, Chen C, Zhang J (2022) A new model to predict the risk of major gastrointestinal bleeding in patients on direct oral anticoagulants (dabigatran and rivaroxaban). Br J Clin Pharmacol. https://doi.org/10.1111/bcp.15491
Schulman S, Kearon C (2005) Subcommittee on control of anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694
Yin MY, Ruckel S, Kfoury AG et al (2018) Novel Model to Predict Gastrointestinal Bleeding During Left Ventricular Assist Device Support. Circ Heart Fail 11(11):e005267
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5(9):1315–1316
Nable JV, Graham AC (2016) Gastrointestinal Bleeding. Emerg Med Clin North Am 34(2):309–325
Srygley FD, Gerardo CJ, Tran T et al (2012) Does this patient have a severe upper gastrointestinal bleed?. JAMA 307(10):1072–1079
Pirmohamed M, James S, Meakin S et al (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 329(7456):15–19
Mercadante S, Barresi L, Casuccio A et al (2000) Gastrointestinal bleeding in advanced cancer patients. J Pain Symptom Manage 19(3):160–162
Abrignani MG, Gatta L, Gabrielli D et al (2021) Gastroprotection in patients on antiplatelet and/or anticoagulant therapy: a position paper of National Association of Hospital Cardiologists (ANMCO) and the Italian Association of Hospital Gastroenterologists and Endoscopists (AIGO). Eur J Intern Med 85:1–13
Olsen AS, McGettigan P, Gerds TA et al (2020) Risk of gastrointestinal bleeding associated with oral anticoagulation and non-steroidal anti-inflammatory drugs in patients with atrial fibrillation: a nationwide study. Eur Heart J Cardiovasc Pharmacother 6(5):292–300
Masclee GM, Valkhoff VE, Coloma PM et al (2014) Risk of upper gastrointestinal bleeding from different drug combinations. Gastroenterology 147(4):784–792.e9; quiz e13–4
Johannsdottir GA, Onundarson PT, Gudmundsdottir BR et al (2012) Screening for anemia in patients on warfarin facilitates diagnosis of gastrointestinal malignancies and pre-malignant lesions. Thromb Res 130(3):e20–e25
Lanas-Gimeno A, Lanas A (2017) Risk of gastrointestinal bleeding during anticoagulant treatment. Expert Opin Drug Saf 16(6):673–685
Alcalá-González L, Jiménez C, Cortina V et al (2022) Severity of gastrointestinal bleeding is similar between patients receiving direct oral anticoagulants or vitamin K antagonists. Rev Esp Enferm Dig
He X, Chen Y (2012) Study of coagulation indexes in patients with cirrhosis. Chinese journal of medicine guide 10(14):126–127
Gerson LB (2013) Causes of gastrointestinal hemorrhage in patients with chronic renal failure. Gastroenterology 145:895,7; discussion 897
Holtz BE (2021) Patients Perceptions of Telemedicine Visits Before and After the Coronavirus Disease 2019 Pandemic. Telemed J E Health 27(1):107–112
Funding
This study was funded by the Science and Technology Innovation Startup Foundation of Fujian Provincial Maternal and Child Health Hospital (YCXY23-02).
Author information
Authors and Affiliations
Contributions
JZ initiated the study. JZ, SW, ML, FM, FZ, and GF collected and entered the data. ML and FM performed data collation. SW and ML performed data extraction and analyses. SW drafted the first version of the manuscript. JZ, SW, ML, FM, FZ, and GF critically reviewed and revised the manuscript. SW and FZ worked on data validation. SJ performed the graphical revisions. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study complies with the Declaration of Helsinki and was authorized by The Ethics Committee of Fujian Medical University Union Hospital.
Informed consent
The requirement for patient consent was waived due to its retrospective nature.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, S., Lv, M., Ma, F. et al. A new model (Alfalfa-Warfarin-GIB) for predicting the risk of major gastrointestinal bleeding in warfarin patients. Eur J Clin Pharmacol 79, 1195–1204 (2023). https://doi.org/10.1007/s00228-023-03533-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03533-0