Abstract
Purpose
To improve outcomes of anterior cruciate ligament reconstruction (ACLR), it is important to understand the reasons for failure of this procedure. This systematic review was performed to identify current failure modes of ACLR.
Methods
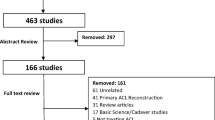
A systematic search was performed using PubMed, EMBASE, Cochrane, and annual registries for ACLR failures. Studies were included when failure modes were reported (I) of ≥ 10 patients and (II) at a minimum of two-year follow-up. Modes of failure were also compared between different graft types and in femoral tunnel positions.
Results
This review included 24 cohort studies and 4 registry-based studies (1 level I, 1 level II, 10 level III, and 16 level IV studies). Overall, a total of 3657 failures were identified. The most common single failure mode of ACLR was new trauma (38%), followed by technical errors (22%), combined causes (i.e. multiple failure mechanisms; 19%), and biological failures (i.e. failure due to infection or laxity without traumatic or technical considerations; 8%). Technical causes also played a contributing role in 17% of all failures. Femoral tunnel malposition was the most common cause of technical failure (63%). When specifically looking at the bone–patellar tendon–bone (BPTB) or hamstring (HT) autografts, trauma was the most common failure mode in both, whereas biological failure was more pronounced in the HT group (4% vs. 22%, respectively). Technical errors were more common following transtibial as compared to anteromedial portal techniques (49% vs. 26%).
Conclusion
Trauma is the single leading cause of ACLR failure, followed by technical errors, and combined causes. Technical errors seemed to play a major or contributing role in large part of reported failures, with femoral tunnel malposition being the leading cause of failure. Trauma was also the most common failure mode in both BPTB and HT grafts. Technical errors were a more common failure mode following transtibial than anteromedial portal technique.
Level of evidence
IV.

Similar content being viewed by others

References
Ahmed I, Salmon L, Roe J, Pinczewski L (2017) The long-term clinical and radiological outcomes in patients who suffer recurrent injuries to the anterior cruciate ligament after reconstruction. Bone Jt J 99B:337–343
Akhtar MA, Bhattacharya R, Ohly N, Keating JF (2011) Revision ACL reconstruction—causes of failure and graft choices. Br J Sports Med 45:A15–A16
Akhtar MA, Bhattacharya R, Keating JF (2016) Generalised ligamentous laxity and revision ACL surgery: Is there a relation? Knee 23:1148–1153
Anand BS, Feller JA, Richmond AK, Webster KE (2016) Return-to-sport outcomes after revision anterior cruciate ligament reconstruction surgery. Am J Sports Med 44:580–584
Balazs GC, Grimm PD, Donohue MA et al (2016) Revision anterior cruciate ligament reconstruction in military personal. J Knee Surg 1:285–305
Boyle C, Pagoti R, Eng KH et al (2019) Revision ACL reconstruction with autograft: long-term functional outcomes and influencing factors. Eur J Orthop Surg Traumatol 29:157–161
Cain EL Jr, Biggers MD, Beason DP et al (2017) Comparison of anterior cruciate ligament graft isometry between paired femoral and tibial tunnels. J Knee Surg 30:960–964
Chen JL, Allen CR, Stephens TE et al (2013) Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med 41:1571–1578
Chen Y, Chua KHZ, Singh A et al (2015) Outcome of single-bundle hamstring anterior cruciate ligament reconstruction using the anteromedial versus the transtibial technique: a systematic review and meta-analysis. Arthroscopy 31:1784–1794
Chen H, Tie K, Qi Y et al (2017) Anteromedial versus transtibial technique in single-bundle autologous hamstring ACL reconstruction: a meta-analysis of prospective randomized controlled trials. J Orthop Surg Res 12:167
Ciccotti MC, Secrist E, Tjoumakaris F et al (2017) Anatomic anterior cruciate ligament reconstruction via independent tunnel drilling: a systematic review of randomized controlled trials comparing patellar tendon and hamstring autografts. Arthroscopy 33:1062–1071.e5
Cristiani R, Sarakatsianos V, Engström B et al (2019) Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 27:381–388
Di Benedetto P, Di Benedetto E, Fiocchi A et al (2016) Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res 28:319–324
Dini F, Tecame A, Ampollini A et al (2019) Multiple ACL revision: failure analysis and clinical outcomes. J Knee Surg. https://doi.org/10.1055/s-0039-3400741
Engebretsen L, Benum P, Fasting O et al (1990) A prospective, randomized study of three surgical techniques for treatment of acute ruptures of the anterior cruciate ligament. Am J Sports Med 18:585–590
Gillquist J, Andersson M, Odensten L, Good J (1989) Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament. A randomized study with long-term follow-up. J Bone Jt Surg 71:965–974
Grassi A, Carulli C, Innocenti M et al (2018) New trends in anterior cruciate ligament reconstruction: a systematic review of national surveys of the last 5 years. Joints 6:177–187
Hettrich CM, Dunn WR, Reinke EK et al (2013) The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med 41:1534–1540
Iio K, Tsuda E, Tsukada H et al (2017) Characteristics of elongated and ruptured anterior cruciate ligament grafts: An analysis of 21 consecutive revision cases. Asia-Pac J Sport Med Arthrosc Rehabil Technol 8:1–7
Inderhaug E, Raknes S, Østvold T et al (2017) Increased revision rate with posterior tibial tunnel placement after using the 70-degree tibial guide in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25:152–158
Jaecker V, Zapf T, Naendrup JH et al (2018) Differences between traumatic and non-traumatic causes of ACL revision surgery. Arch Orthop Trauma Surg 138:1265–1272
Johnson WR, Makani A, Wall AJ et al (2015) Patient outcomes and predictors of success after revision anterior cruciate ligament reconstruction. Orthop J Sport Med 3:1–7
Kaeding CC, Aros B, Pedroza A et al (2011) Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a moon prospective longitudinal cohort. Sports Health 3:73–81
Kamath GVG, Redfern JCJ, Greis PEP, Burks RRT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Kim HS, Seon JK, Jo AR (2013) Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res 25:165–173
Kuršumović K, Charalambous CP (2016) Graft salvage following infected anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Bone Jt J 98-B:608–615
Lee DW, Kim JG, Cho SI, Kim DH (2019) Clinical outcomes of isolated revision anterior cruciate ligament reconstruction or in combination with anatomic anterolateral ligament reconstruction. Am J Sports Med 47:324–333
Lefevre N, Klouche S, Mirouse G et al (2017) Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST cohort. Am J Sports Med 45:34–41
Legnani C, Peretti G, Borgo E et al (2017) Revision anterior cruciate ligament reconstruction with ipsi- or contralateral hamstring tendon grafts. Eur J Orthop Surg Traumatol 27:533–537
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 17:117–124
Lynch TS, Parker RD, Patel RM et al (2015) The impact of the multicenter orthopaedic outcomes network (MOON) research on anterior cruciate ligament reconstruction and orthopaedic practice. J Am Acad Orthop Surg 23:154–163
Magnussen RA, Taylor DC, Toth AP, Garrett WE (2012) ACL graft failure location differs between allografts and autografts. Sport Med Arthrosc Rehabil Ther Technol 4:22
Magnussen RA, Trojani C, Granan LP et al (2015) Patient demographics and surgical characteristics in ACL revision: a comparison of French, Norwegian, and North American cohorts. Knee Surg Sports Traumatol Arthrosc 23:2339–2348
Mahmoud SSS, Odak S, Coogan S, McNicholas MJ (2014) A prospective study to assess the outcomes of revision anterior cruciate ligament reconstruction. Int Orthop 38:1489–1494
MARS Study Group (2016) The development and early to midterm findings of the multicenter revision anterior cruciate ligament study. J Knee Surg 29:528–532
Matava MJ, Arciero RA, Baumgarten KM et al (2015) Multirater agreement of the causes of anterior cruciate ligament reconstruction failure: a radiographic and video analysis of the MARS cohort. Am J Sports Med 43:310–319
Ménétrey J, Duthon VB, Laumonier T, Fritschy D (2008) “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc 16:224–231
Mengdi SuM, Jia X, Zhang Z et al (2019) Medium-term (least 5 years) comparative outcomes in anterior cruciate ligament reconstruction using 4SHG, allograft, and LARS ligament. Clin J Sport Med. https://doi.org/10.1097/JSM.0000000000000730
Mirouse G, Rousseau R, Casabianca L et al (2016) Return to sports and functional results after revision anterior cruciate ligament reconstruction by fascia lata autograft. Orthop Traumatol Surg Res 102:863–866
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Mohtadi N, Barber R, Chan D et al (2016) Complications and adverse events of a randomized clinical trial comparing 3 graft types for ACL reconstruction. Clin J Sport Med 26:182–189
Morgan JA, Dahm D, Levy B et al (2012) Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg 25:361–368
Nagaraj R, Kumar MN (2019) Revision anterior cruciate ligament reconstruction in the nonathlete population. Indian J Orthop 53:154–159
Obremskey WT, Pappas N, Attallah-Wasif E et al (2005) Level of evidence in orthopaedic journals. J Bone Jt Surg Ser A 87:2632–2638
Parkinson B, Robb C, Thomas M et al (2017) Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 45:1529–1536
Pascual-Garrido C, Carbo L, Makino A (2014) Revision of anterior cruciate ligament reconstruction with allografts in patients younger than 40 years old: A 2 to 4 year results. Knee Surg Sports Traumatol Arthrosc 22:1106–1111
Prentice HA, Lind M, Mouton C et al (2018) Patient demographic and surgical characteristics in anterior cruciate ligament reconstruction: a description of registries from six countries. Br J Sports Med 52:716–722
Rahardja R, Zhu M, Love H et al (2019) Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL Registry. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05773-z
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC (2013) Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: Results from the danish knee ligament reconstruction register. Arthroscopy 29:98–105
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. Am J Sports Med 42:278–284
Redler A, Iorio R, Monaco E et al (2018) Revision anterior cruciate ligament reconstruction with hamstrings and extra-articular tenodesis: a mid- to long-term clinical and radiological study. Arthroscopy 34:3204–3213
Reverte-Vinaixa MM, Minguell J, Joshi N et al (2014) Revision anterior cruciate ligament reconstruction using tibial or hamstring tendon allografts. J Orthop Surg 22:60–64
Robin BN, Jani SS, Marvil SC et al (2015) Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 31:1412–1417
Rousseau R, Labruyere C, Kajetanek C et al (2019) Complications after anterior cruciate ligament reconstruction and their relation to the type of graft: a prospective study of 958 cases. Am J Sports Med 47:2543–2549
Schlumberger M, Schuster P, Schulz M et al (2017) Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc 25:1535–1541
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Steadman JR, Matheny LM, Jason MP et al (2015) Patient-centered outcomes and revision rate in patients undergoing acl reconstruction using bone-patellar tendon-bone autograft compared with bone-patellar tendon-bone allograft: a matched case-control study. Arthroscopy 31:1–7
Takazawa Y, Ikeda H, Saita Y et al (2015) Case series: Revision anterior cruciate ligament reconstructions using patellar tendon autografts. Knee 22:569–573
Trojani C, Sbihi A, Djian P et al (2011) Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc 19:196–201
Vališ P, Sklenský J, Repko M et al (2014) Most frequent causes of autologous graft failure in anterior cruciate ligament replacement. Acta Chir Orthop Traumatol Cech 81:371–379
Vap AR, Persson A, Fenstad AM et al (2019) Re-revision anterior cruciate ligament recoonstruction: an evaluation from the Norwergina knee ligament registry. Arthroscopy 35:1695–1701
Waltz RA, Solomon DJ, Provencher MT (2014) A radiographic assessment of failed anterior cruciate ligament reconstruction: can magnetic resonance imaging predict graft integrity? Am J Sports Med 42:1652–1660
Wang C, Lee YH, Siebold R (2014) Recommendations for the management of septic arthritis after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 22:2136–2144
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Wiggins AJ, Grandhi RK, Schneider DK et al (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 44:1861–1876
Wright RW, Huston LJ, Spindler KP et al (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38:1979–1986
Wright RW, Gill CS, Chen L et al (2012) Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Jt Surg 94:531–536
Yabroudi MA, Björnsson H, Lynch AD et al (2016) Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sport Med 4:1–7
Yoon KH, Kim JS, Park SY, Park SE (2018) The influence of segond fracture on outcomes after anterior cruciate ligament reconstruction. Arthroscopy 34:1900–1906
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gregory S. DiFelice declares he is a paid consultant and receives research grants from Arthrex (Naples, FL, USA). Gino M.M.J Kerkhoffs declares that the Department of Orthopedic Surgery of the Amsterdam University Medical Centers received an unrestricted research Grant from Arthrex (Naples, FL, USA).
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vermeijden, H.D., Yang, X.A., van der List, J.P. et al. Trauma and femoral tunnel position are the most common failure modes of anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 28, 3666–3675 (2020). https://doi.org/10.1007/s00167-020-06160-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06160-9