Abstract
Background
Although some studies have suggested that women with schizophrenia are more likely to achieve positive outcomes, the evidence-base is fraught with inconsistencies. In this study we compare the long-term course and outcomes for men and women living with schizophrenia in rural Ethiopia.
Methods
The Butajira course and outcome study for severe mental disorders is a population-based cohort study. Community ascertainment of cases was undertaken between 1998 and 2001, with diagnostic confirmation by clinicians using the Schedules for Clinical Assessment in Neuropsychiatry. Findings from annual outcome assessments were combined with clinical records, patient and caregiver report, and psychiatric assessments at 10–13 years using the Longitudinal Interval Follow-up Evaluation- LIFE chart. For the sub-group of people with schizophrenia (n = 358), we compared course of illness and treatment, co-morbidity, recovery, social outcomes and mortality between men and women. Multivariable analyses were conducted for modelling associations identified in bivariate analyses according to blocks shaped by our a priori conceptual framework of the biological and social pathways through which gender might influence the course and outcome of schizophrenia.
Results
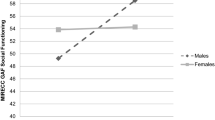
Looking into over 10–13 years of follow-up data, there was no difference in the functioning or recovery in women compared to men (AOR = 1.79, 95% CI = 0.91, 3.57). Women were less likely to report overall life satisfaction (AOR = 0.22, 95% CI = 0.09, 0.53) or good quality of spousal relationships (AOR = 0.09, 95% CI = 0.01–1.04). Men were more likely to have co-morbid substance use and there was a trend towards women being more likely to be prescribed an antidepressant (AOR = 2.38, 95% CI = 0.94, 5.88). There were no gender differences in the course of illness, number of psychotic episodes or adherence to medications.
Conclusion
In this rural African setting, we found little evidence to support the global evidence indicating better course and outcome of schizophrenia in women. Our findings are suggestive of a gendered experience of schizophrenia which varies across contexts. Further investigation is needed due to the important implications for the development of new mental health services in low and middle-income country settings.

Similar content being viewed by others
References
Haro JM et al (2011) Cross-national clinical and functional remission rates: Worldwide Schizophrenia Outpatient Health Outcomes (W-SOHO) study. Br J Psychiatry 199(3):194–201
Novick D et al (2016) Sex differences in the course of schizophrenia across diverse regions of the world. Neuropsychiatr Dis Treat 12:2927–2939
Ran MS et al (2015) Gender differences in outcomes in people with schizophrenia in rural China: 14-year follow-up study. Br J Psychiatry 206(4):283–288
Grossman LS et al (2008) Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry 49(6):523–529
Morgan VA, Castle DJ, Jablensky AV (2008) Do women express and experience psychosis differently from men? Epidemiological evidence from the Australian National Study of Low Prevalence (Psychotic) Disorders. Aust N Z J Psychiatry 42(1):74–82
Goldstein RZ et al (2002) Neurocognitive correlates of response to treatment in formal thought disorder in patients with first-episode schizophrenia. Neuropsychiatry Neuropsychol Behav Neurol 15(2):88–98
Thara R, Rajkumar S (1992) Gender differences in schizophrenia. Results of a follow-up study from India. Schizophr Res 7(1):65–70
Bergh S et al (2016) Predictors and longitudinal course of cognitive functioning in schizophrenia spectrum disorders, 10years after baseline: The OPUS study. Schizophr Res 175(1–3):57–63
Morgan C et al (2014) Reappraising the long-term course and outcome of psychotic disorders: the AESOP-10 study. Psychol Med 44(13):2713–2726
Newman SC, Bland RC, Thompson AH (2012) Long-term course and outcome in schizophrenia: a 34-year follow-up study in Alberta, Canada. Psychol Med 42(10):2137–2143
Harrison G et al (2001) Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 178:506–517
Munk-Jorgensen P, Mortensen PB (1992) Social outcome in schizophrenia: a 13-year follow-up. Soc Psychiatry Psychiatr Epidemiol 27(3):129–134
Morgan C et al (2016) The incidence of psychoses in diverse settings, INTREPID (2): a feasibility study in India, Nigeria, and Trinidad. Psychol Med 46(9):1923–1933
Harvey CA et al (2007) The Camden Schizophrenia Surveys III: Five-year outcome of a sample of individuals from a prevalence survey and the importance of social relationships. Int J Soc Psychiatry 53(4):340–356
Kebede D et al (2003) Onset and clinical course of schizophrenia in Butajira-Ethiopia—a community-based study. Soc Psychiatry Psychiatr Epidemiol 38(11):625–631
Leff J et al (1992) The international pilot study of Schizophrenia: five-year follow-up findings. Psychol Med 22(1):131–145
Gureje O, Bamidele R (1999) Thirteen-year social outcome among Nigerian outpatients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 34(3):147–151
Gureje O, Bamidele RW (1998) Gender and schizophrenia: association of age at onset with antecedent, clinical and outcome features. Aust N Z J Psychiatry 32(3):415–423
Alem A et al (2009) Clinical course and outcome of schizophrenia in a predominantly treatment-naive cohort in rural Ethiopia. Schizophr Bull 35(3):646–654
Shibre T et al (2015) Long-term clinical course and outcome of schizophrenia in rural Ethiopia: 10-year follow-up of a population-based cohort. Schizophr Res 161(2–3):414–420
Charlson FJ et al (2018) Global epidemiology and burden of Schizophrenia: Findings from the global burden of disease study 2016. Schizophr Bull 44(6):1195–1203
Kebede D et al (2004) The sociodemographic correlates of schizophrenia in Butajira, rural Ethiopia. Schizophr Res 69(2–3):133–141
Teferra S et al (2011) Five-year mortality in a cohort of people with schizophrenia in Ethiopia. BMC Psychiatry 11:165
Fekadu A et al (2015) Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. Br J Psychiatry 206(4):289–296
Eranti SV et al (2013) Gender difference in age at onset of schizophrenia: a meta-analysis. Psychol Med 43(1):155–167
Kebede D et al (2005) Short-term symptomatic and functional outcomes of schizophrenia in Butajira, Ethiopia. Schizophr Res 78(2–3):171–185
Shibre T et al (2008) Traditional treatment of mental disorders in rural Ethiopia. Ethiop Med J 46(1):87–91
Alem A et al (2004) Comparison of computer assisted scan diagnoses and clinical diagnoses of major mental disorders in Butajira, rural Ethiopia. Ethiop Med J 42(2):137–143
Sartorius N, Janca A (1996) Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol 31(2):55–69
Andreason NC (1984) Scale for the assessment of negative symptoms/scale for the assessment of positive symptoms. University of Iowa Press, Iowa City
Jones SH et al (1995) A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). Br J Psychiatry 166(5):654–659
Keller MB et al (1987) The longitudinal interval follow-up evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 44(6):540–548
Birmaher B, Axelson D (2006) Course and outcome of bipolar spectrum disorder in children and adolescents: a review of the existing literature. Dev Psychopathol 18(4):1023–1035
Ojserkis R et al (2017) The impact of lifetime PTSD on the seven-year course and clinical characteristics of OCD. Psychiatry Res 258:78–82
Kebede D et al (2019) The 10-year functional outcome of schizophrenia in Butajira, Ethiopia. Heliyon 5(3):e01272
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Pai S, Kapur RL (1981) The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry 138:332–335
Ohaeri JU (1993) Long-term outcome of treated schizophrenia in a Nigerian cohort. Retrospective analysis of 7-year follow-ups. J Nerv Ment Dis 181(8):514–516
Jaaskelainen E et al (2013) A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull 39(6):1296–1306
Shibre T et al (2001) Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol 36(6):299–303
Thara R, Kamath S (2015) Women and schizophrenia. Indian J Psychiatry 57(Suppl 2):S246–S251
Ran M et al (2001) Natural course of schizophrenia: 2-year follow-up study in a rural Chinese community. Br J Psychiatry 178:154–158
Morgan C et al (2015) Searching for psychosis: INTREPID (1): systems for detecting untreated and first-episode cases of psychosis in diverse settings. Soc Psychiatry Psychiatr Epidemiol 50(6):879–893
Hanlon C et al (2016) Task sharing for the care of severe mental disorders in a low-income country (TaSCS): study protocol for a randomised, controlled, non-inferiority trial. Trials 17:76
Lund C et al (2015) Generating evidence to narrow the treatment gap for mental disorders in sub-Saharan Africa: rationale, overview and methods of AFFIRM. Epidemiol Psychiatr Sci 24(3):233–240
Mugisha J et al (2017) Health systems context(s) for integrating mental health into primary health care in six Emerald countries: a situation analysis. Int J Ment Health Syst 11:7
Mayston R et al (2016) Participatory planning of a primary care service for people with severe mental disorders in rural Ethiopia. Health Policy Plan 31(3):367–376
Padmanathan P, De Silva MJ (2013) The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med 97:82–86
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mayston, R., Kebede, D., Fekadu, A. et al. The effect of gender on the long-term course and outcome of schizophrenia in rural Ethiopia: a population-based cohort. Soc Psychiatry Psychiatr Epidemiol 55, 1581–1591 (2020). https://doi.org/10.1007/s00127-020-01865-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01865-1