Abstract
Background
Radial artery cannulation helps to maintain the stability of maternal hemodynamics and reduce complications; however, it is difficult for women with gestational hypertension. Subcutaneous nitroglycerin was found to improve the first attempt success rate of radial artery cannulation in pediatric patients. Therefore, this study evaluated the effect of subcutaneous nitroglycerin on the radial artery diameter and area, blood flow rate and the success rate of radial artery cannulation in women with pregnancy-induced hypertension.
Methods
A total of 94 women with gestational hypertension and risk of intraoperative bleeding undergoing cesarean section were identified and randomized into the subcutaneous nitroglycerin group and control group. The primary outcome was the success rate of left radial artery cannulation within 3 min after subcutaneous injecting (T2). The puncture time, number of attempts, the overall complications, and ultrasonographic measurements including radial artery diameter, cross-sectional area and depth were also recorded before subcutaneous injection (T1), 3 min after subcutaneous injection (T2) and immediately after radial artery cannulation (T3).
Results
The first attempt success rate of radial artery cannulation was significantly higher (97.9% vs. 76.6%, p = 0.004) and procedure time to success was significantly shorter (111 ± 18 s vs. 171 ± 70 s, p < 0.001) in the subcutaneous nitroglycerin group as compared to the control group. The subcutaneous nitroglycerin group also had a significantly less overall number of attempts as 1/2/3 attempts (n), 46/1/0 vs. 36/7/4 (p = 0.008). Compared with the control group, the diameter and cross-sectional area of radial artery increased significantly at the T2 and T3 points in the subcutaneous nitroglycerin group (p < 0.001), as well as percentage change of radial artery diameter and CSA. Vasospasm (6.4% vs. 31.9%; p = 0.003) was significantly lower in the subcutaneous nitroglycerin group; however, no difference was found in hematoma (2.1% vs. 12.8%; p = 0.111).
Conclusion
Subcutaneous nitroglycerin along with the routine local anesthetic preparation before radial artery cannulation increased the first attempt success rate of radial artery cannulation and decreased the overall number of cannulation attempts in women with gestational hypertension and risks of intraoperative bleeding undergoing cesarean section, it also decreased cannulation times and overall number of vasospasms.
Zusammenfassung
Hintergrund
Die Kanülierung der A. radialis trägt zur Aufrechterhaltung der maternalen Hämodynamik und zur Verringerung von Komplikationen bei. Bei Frauen mit Schwangerschaftshypertonie ist dies jedoch schwierig. Es wurde festgestellt, dass subkutanes Nitroglyzerin die Erfolgsquote beim ersten Versuch der Kanülierung der A. radialis bei pädiatrischen Patientinnen verbessert. Daher wurde in dieser Studie die Wirkung von subkutanem Nitroglyzerin auf den Durchmesser und die Fläche der A. radialis, die Blutflussrate und die Erfolgsrate der Kanülierung der A. radialis bei Frauen mit schwangerschaftsbedingter Hypertonie untersucht.
Methoden
Insgesamt 94 Frauen mit Schwangerschaftshypertonie und dem Risiko einer intraoperativen Blutung, die sich einem Kaiserschnitt unterziehen mussten, wurden identifiziert und nach dem Zufallsprinzip in eine Gruppe mit subkutanem Nitroglyzerin und eine Kontrollgruppe eingeteilt. Als primäres Ergebnis wurde die Erfolgsrate der Kanülierung der linken Radialarterie innerhalb von 3 min nach der subkutanen Injektion (T2) ermittelt. Die Punktionszeit, die Anzahl der Versuche, die Gesamtkomplikationen und die sonographischen Messungen einschließlich des Durchmessers der Radialarterie, der Querschnittsfläche und der Tiefe wurden ebenfalls vor der subkutanen Injektion (T1), 3 min nach der subkutanen Injektion (T2) und unmittelbar nach der Kanülierung der Radialarterie (T3) aufgezeichnet.
Ergebnisse
Die Erfolgsquote beim ersten Versuch der Kanülierung der A. radialis war in der subkutanen Nitroglyzerin-Gruppe im Vergleich zur Kontrollgruppe signifikant höher (97,9 % vs. 76,6 %; p = 0,004) und die Zeit bis zum Erfolg war signifikant kürzer (111 ± 18 s vs. 171 ± 70 s; p < 0,001). In der subkutanen Nitroglyzerin-Gruppe war auch die Gesamtzahl der Versuche signifikant geringer (1/2/3 Versuche [n], 46/1/0 vs. 36/7/4; p = 0,008). Im Vergleich zur Kontrollgruppe nahmen der Durchmesser und die Querschnittsfläche der A. radialis an den Punkten T2 und T3 in der subkutanen Nitroglyzerin-Gruppe signifikant zu (p < 0,001), ebenso wie die prozentuale Veränderung des Durchmessers und des CSA der A. radialis. Der Vasospasmus (6,4 % vs. 31,9 %; p = 0,003) war in der subkutanen Nitroglyzerin-Gruppe signifikant geringer. Es wurde jedoch kein Unterschied in Bezug auf Hämatome festgestellt (2,1 % vs. 12,8 %; p = 0,111).
Schlussfolgerung
Subkutanes Nitroglyzerin zusammen mit der routinemäßigen Vorbereitung auf die Lokalanästhesie vor der Kanülierung der A. radialis erhöhte die Erfolgsrate beim ersten Versuch der Kanülierung der A. radialis und verringerte die Gesamtzahl der Kanülierungsversuche bei Frauen mit Schwangerschaftshypertonie und dem Risiko einer intraoperativen Blutung, die sich einem Kaiserschnitt unterziehen. Außerdem verringerte es die Kanülierungszeiten und die Gesamtzahl der Gefäßspasmen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, about 10% of women have pregnancy-induced hypertension during pregnancy, and hypertensive disease is still a risk factor for maternal and neonatal morbidity and mortality [1, 2]. The incidence of pregnancy-induced hypertension may increase as the increased incidence of obesity, maternal age and comorbidities [1]. Women with gestational hypertension should receive the same standards of critical care as other acutely ill patients [1]. Radial artery cannulation was a common operation in critical care, which helps to maintain the stability of maternal hemodynamics and reduce complications. Radial artery cannulation has several advantages, including easy compressibility, superficial location, distance from vital nerves, and low rate of procedural complications [3, 4].
However, it is difficult for women with pregnancy-induced hypertension as the basic pathological feature of pregnancy-induced hypertension is systemic arteriole spasm [1]. Although ultrasound guidance can significantly increase radial artery cannulation success rate [5,6,7], the success rate of initial cannulation is still varied from 51% to 95%. Furthermore, the success rate of initial cannulation in patients with gestational hypertension is not clear [8,9,10,11,12].
Nitroglycerin is an effective vasodilator and topical nitroglycerin has been used to dilate arteries [13, 14]. A recent study even found that subcutaneous nitroglycerin improved the radial artery cannulation success rate in pediatric patients [15]; however, there was no evidence for women with gestational hypertension. Therefore, this study aimed to evaluate the effectiveness and safety of subcutaneous nitroglycerin on radial artery puncture in women with gestational hypertension.
Methods
Study design
The Ethics Committee of Hangzhou Women’s Hospital approved this study (IRB:2021-K(9)-02). This prospective, randomized, and double-blind trial was conducted from 3 January 2022 to 6 June 2022 after received written informed consent from all participants and finally 94 women were recruited.
Women with gestational hypertension and risks of intraoperative bleeding should receive intraoperative invasive arterial blood pressure monitoring undergoing elective cesarean section will be selected. Gestational hypertension includes mild preeclampsia and severe preeclampsia. Severe preeclampsia was defined as a blood pressure of 160/100 mm Hg or greater on two occasions at least 4 h apart while the patient was on bed rest. Risks of intraoperative bleeding were placental abruption, placental implantation, multiple cesarean sections according to the obstetrican’s judgment.
The exclusion criteria were emergency surgery, negative modified Allen’s test, infection or external injury at or near the puncture site, coagulopathy, and vascular diseases such as vasculitis.
Standard monitoring was applied, and we suggested applying intraoperative invasive arterial blood pressure monitoring for women with gestational hypertension and risks of intraoperative bleeding during cesarean section at our medical institution. All women were supine with the arm extended to 60° and supported on the arm plate during artery cannulation and ultrasonographic measurements.
Randomization and blinding
The pregnant women were randomly divided into a control group and a nitroglycerin group at a 1:1 ratio by an independent researcher using numbered sealed envelopes. An independent researcher performed nitroglycerin injection or local anesthesia and was not involved in data collection. A doctor with much experience in vascular examinations performed the ultrasound examinations and was blind to the group allocation. The outcome assessor who was unaware of the group allocation evaluated the cross-sectional area and diameter of the radial artery according to ultrasonographic measurements. In addition, the included patients, surgical doctors, and data analysts were all blinded to the group assignments.
Subcutaneous nitroglycerin preparation and injection
A solution of lidocaine 0.2 ml of 0.8% lidocaine combined with 300 µg (0.3 ml) nitroglycerin (1 mg/ml) was subcutaneously injected in the nitroglycerin group, and 0.5 ml of 0.8% lidocaine without nitroglycerin was subcutaneously injected in the control group. Dosing was slowly administered for more than 5 s to avoid systemic vasodilation.
Ultrasonographic measurements
Baseline measurements (T1) were performed before subcutaneous injection. All variables were measured again at 3 min after subcutaneous injection (T2) and immediately after radial artery cannulation (T3).
The ultrasonic probe was placed longitudinally over the radial artery, and ultrasonographic measurements were recorded close to 2 cm from the radial styloid process. A mindray machine (M9, Shenzhen, Guangdong, China) with a 4–12 MHz variable frequency linear array transducer and a 1–5 MHz variable frequency convex array ultrasound transducer were applied. A set of vital signs and ultrasonographic parameters, such as internal diameter (cm, Fig. 1a), cross-sectional area (cm2, CSA) of radial artery (Fig. 1b) and depth (cm, Fig. 1a) under short axis (out of plane) view, were measured [5, 16]. Radial artery diameter is measured as the vertical distance between the inner walls of an artery by an electronic caliper on a machine [17], and the image corresponding to the end diastole is located by freezing the image at the end diastole. Radial artery depth is measured as the distance between the transducer and the near edge of the artery.
After activating pulsed wave Doppler ultrasound (PWD) mode, the volumetric gate was placed in the center of the arterial lumen, the arterial hemodynamics parameters were recorded. The ultrasound angle was kept between 30° and 60° in the process of the examination, which was defined as the angle between the direction of blood flow and the ultrasound beam. The time average maximal velocity (TAMAX, cm/s) was recorded as shown in Fig. 1c. According to a previous study [18], the volume of blood flow (ml/s) was also calculated as CSA × TAMAX (Fig. 1c).
Ultrasound-guided radial artery cannulation
The left radial artery was chosen and the puncture point was close to 2 cm from the radial styloid process. The operator performed ultrasound-guided puncture at 3 min after the intervention/control injection and the puncture time was recorded.
We applied the out-of-plane without guide wire technique and a 20-gauge arterial catheter to perform arterial cannulation [19, 20]. During ultrasound-guided arterial catheterization, the operator was not allowed to intentionally puncture either wall of the artery. However, guide wires were not allowed in order to eliminate the effect of other factors on outcomes. It was assumed that the cannulation had been completed when the arterial waveform was shown on the monitor. It was considered to have failed if cannulation was not accomplished in 10 min [15]. After the failure, a contralateral radial artery was used for cannulation without subcutaneous injection. The total operation time of arterial cannulation was recorded as the time between the first puncture of the skin with the needle catheter and the arterial waveform was shown on the monitor. We also recorded intraoperative complications, including hematoma and vasospasm, which were defined as the radial artery diameter decreasing by more than 25% after cannulation [4, 21,22,23,24,25,26]. The patients’ basic documentation was collected, including age, body mass index, and the American Society of Anesthesiologists physical (ASA) condition classification.
Primary outcome
The primary outcome was defined as the first attempt success rate of radial artery cannulation within 3 min after injecting. Secondary results included the puncture time, number of attempts, radial artery diameter, cross-sectional area and depth at T1, T2 and T3 points, and the overall complications.
Sample size
The radial artery cannulation success rate was 91.2% and 66.1% in the subcutaneous nitroglycerin group and the control group, respectively [15]. A two-tailed χ2 test with a type I error probability of 0.05 was performed and 94 patients were estimated to provide 80% power (G-Power version 3.1; The Institute for Experimental Psychology in Dusseldorf, Germany).
Statistical analysis
Categorical variables were expressed as frequency (percentage age), normally and nonnormally distributed variables were expressed as the mean ± SD and the medians with interquartile ranges, respectively. The Pearson test was used for the correlation analysis. Between the groups and the different times, repeated measurements data were analyzed by repeated measured variables. Differences between the groups measured at the same time points were performed using Student’s two-sample t test or the Mann-Whitney U test. The limit of statistical significance was set to p < 0.05 when two-sided p values are performed (SPSS V. 18.0, XXX, Chicago, IL, USA).
Results
Baseline clinical parameters
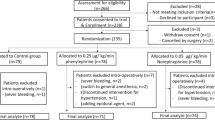
Of 108 women with gestational hypertension and risks of intraoperative bleeding who underwent cesarean section, 94 patients were identified and completed the follow-up, and 14 patients met the exclusion criteria as shown in Fig. 2. The basic parameters of the two groups are summarized in Table 1, and no difference was found.
The average age of the study population was 31 years, the average body mass index (BMI) was 28, the average estimated gestational age was 38 weeks, 12.8% had severe preeclampsia, and the other patients had mild preeclampsia.
Over time, no statistically significant differences were observed in blood pressure and HR (heart rate) between the two groups (Supplemental Fig. 1).
Radial artery cannulation
Compared to the control group, the first attempt success rate of radial artery cannulation was significantly higher (97.9% vs. 76.6%, p = 0.004) and procedure time to success within the first attempt was significantly shorter (111 ± 18 s vs. 171 ± 70 s, p < 0.001) in the nitroglycerin group. The nitroglycerin group also had a significantly lower overall number of attempts (1/2/3 attempts n, 46/1/0 vs. 36/7/4, p = 0.008). However, there was no difference in second attempt success rate within 10 min (100% vs. 91.5%; p = 0.117) between the two groups. Vasospasm (6.4% vs. 31.9%; p = 0.003) was significantly lower in the subcutaneous nitroglycerin group. However, no difference was found in hematoma (2.1% vs. 12.8%; p = 0.111). (Table 2).
Ultrasonographic measurements
Over time, the diameter and CSA of radial artery showed significant differences between the two groups (p < 0.001). Compared with control group, the diameter and CSA of radial artery increased significantly at the T2 and T3 points in nitroglycerin group (p < 0.001), as well as the percentage change in radial artery diameter and CSA. No differences were found in the depth at the T1, T2 and T3 points between the groups (P = 0.289) (Table 3, Fig. 3a for diameter, Fig. 3b for CSA and Fig. 3c for depth).
Results of ultrasonographic measurements: a radial artery diameter (mm), b cross-sectional area (CSA, cm2), c depth (mm), d time average maximal velocity (TAMAX, cm/sec), e volume of blood flow (ml/sec). T1 = baseline; T2 = 3 min after subcutaneous injection; T3 = immediately after radial artery cannulation
No differences were found in the TAMAX (P > 0.05) at the T1 and T2 points between the two groups. The volume of blood flow (P < 0.001) was significantly increased in the nitroglycerin group at the T2 point, but no difference was found at the T1 point (P = 0.447) (Table 3, Fig. 3d for TAMAX and Fig. 3e for blood flow).
Discussion
The main finding of this study was that subcutaneous nitroglycerin increased the first attempt success rate of radial artery cannulation in women with gestational hypertension undergoing cesarean section. The relatively large diameter of the radial artery in the subcutaneous nitroglycerin group and improvement in palpability of radial pulse may contribute to the improved success rate, which is consistent with previous studies [15, 27]. We also found that subcutaneous nitroglycerin decreased cannulation times and overall number of cannulation attempts.
Successful radial artery cannulation was challenging for pregnant women with gestational hypertension. First, the anesthesiologists have less experience in ultrasound-guided arterial cannulation in this obstetrics and gynecology hospital. Second, the main challenge for successful radial artery catheterization in patients was the small diameter of the artery [15]. Generalized vasoconstriction is a feature of gestational hypertension [28]. Vasospasm or hematoma caused by failed attempts further reduces the artery’s inner diameter and the cannulation success rate [21, 23] As the radial artery was dominated by α1-adrenergic receptors [29], the radial artery was prone to vasospasm during cannulation attempts. Second, the effect of lidocaine injection on diameter of radial artery was paradoxical, one study showed expansion effects [27] and another study reported vasoconstriction [30]. On the other hand, radial artery was more sensitive to nitroglycerin as compared to other muscular arteries [31], and subcutaneously infiltrated nitroglycerin could result in marked radial artery vasodilation. This lead to avoidance of precannulation spasm and enhance palpability of the radial pulse, and thus improved the puncture of radial artery [27].
Up to 57% of cases would experience temporary vasospasm immediately after puncture of radial artery [32], and sustained vasospasm was reported in 4–20% during adult transradial cardiac catheterization [21]. A total of 15 patients (31.9%) experienced vascular spasm in the control group but only 3 (6.4%) patients in the nitroglycerin group. As a result, after the occurrence of vasospasm, the radial artery was successfully cannulated in 11 cases and failed in 4 cases of the 15 patients in the control group. The control group had a higher risk of vasospasm or complete occlusion. The radial artery catheterization was successful in 3 cases in the subcutaneous nitroglycerin group. In the control group, cannulation after vascular spasm failed in 4 (8.5%) patients. The relatively large radial artery inner diameter of subcutaneous nitroglycerin administration may increase the success rate of second attempts and reduce catheter failures. We found that subcutaneous nitroglycerin increases the diameter and CSA of radial artery, which is consistent with previous study [15]; however, few studies were concerned with the effect of subcutaneous nitroglycerin on TAMAX, or blood flow velocity. Additionally, a previous study has noticed that the depth of radial artery would affect ultrasound-guided cannulation [33]. A radial artery depth between 2 and 4 mm would get a higher first attempt success rate than those that are less than 2 mm or 4 mm or more in small pediatric patients [33]. Therefore, a small volume (0.5 ml) of local anesthetic or combined nitroglycerin solution was adopted to optimize the depth of radial artery. After subcutaneous injection, the mean radial artery depth of the two groups was in the range of 2–4 mm, and no significant difference was found between the two groups.
Different approaches, such as local [13], subcutaneous [34] and intra-arterial [26] approaches, were used in adult patients with radial artery dilatation administered with nitroglycerin. Intra-arterial nitroglycerin could decrease vasospasm and radial artery occlusion in adult cardiac patients, but not in arterial puncture patients, causing hematoma and reducing arterial diameter. Noninvasive vasodilation of the radial artery was the advantage of topical nitroglycerin cream; however, it should be smeared to the skin for at least 30 min before puncture of radial artery. Subcutaneous nitroglycerin stayed extravascular and acted locally for a longer duration to produce vasodilation than sublingual route of nitroglycerin administration [35]. Therefore, the authors chose subcutaneous nitroglycerin injection above the radial artery, which was the most effective method with minimal possible systemic side effects.
According to previous studies [27], 400–500 μg nitroglycerin is subcutaneously injected to facilitate radial artery cannulation without systemic hypotension in adult cardiac patients. Therefore, we determined the dose of 300 µg/0.3 ml nitroglycerin based on the pretest in the current study. In the current study, diameter of radial artery was significantly increased and no systemic side effect was observed in the subcutaneous nitroglycerin group, which is consistent with previous studies [15, 27, 36].
Limitations
The current study has some limitations. First, the total sample was relatively small. Second, subcutaneous nitroglycerin should be injected near the target site as the radial artery dilatation occurs locally near the injection site. Third, subcutaneous injection may mask the ultrasound image of the radial artery, so it should be carefully injected under direct ultrasound without bubbles. Fourth, we evaluated radial artery diameter and distal perfusion only intraoperatively. As the timing of catheter removal varies with the type of surgery and clinical situation, we were unable to assess the radial artery diameter and distal perfusion after catheter removal.
Conclusion
Subcutaneous nitroglycerin combined with local anesthetics before cannulation increased the first attempt success rate of radial artery cannulation and decreased the overall number of cannulation attempts in women with gestational hypertension and risks of intra-operative bleeding undergoing cesarean section. It also decreased cannulation times and overall number of vasospasms. It may be useful for those anesthesiologists with less experience in radial artery cannulation.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CSA:
-
Cross-sectional area
- TAMAX:
-
Time-average maximum velocity
References
Russell R (2020) Preeclampsia and the anaesthesiologist: current management. Curr Opin Anaesthesiol 33(3):305–310
Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800
Kim EH, Lee JH, Song IK, Kim JT, Lee WJ, Kim HS (2017) Posterior tibial artery as an alternative to the radial artery for arterial cannulation site in small children: a randomized controlled study. Anesthesiology 127(3):423–431
Brzezinski M, Luisetti T, London MJ (2009) Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg 109(6):1763–1781
Song IK, Choi JY, Lee JH et al (2016) Short-axis/out-of-plane or long-axis/in-plane ultrasound-guided arterial cannulation in children: a randomised controlled trial. Eur J Anaesthesiol 33(7):522–527
Ishii S, Shime N, Shibasaki M, Sawa T (2013) Ultrasound-guided radial artery catheterization in infants and small children. Pediatr Crit Care Med 14(5):471–473
Schwemmer U, Arzet HA, Trautner H, Rauch S, Roewer N, Greim CA (2006) Ultrasound-guided arterial cannulation in infants improves success rate. Eur J Anaesthesiol 23(6):476–480
Kiberenge RK, Ueda K, Rosauer B (2018) Ultrasound-guided dynamic needle tip positioning technique versus palpation technique for radial arterial cannulation in adult surgical patients: a randomized controlled trial. Anesth Analg 126(1):120–126
Kim N, Kim HI, Kim DH, Park D, Song SH, Byon HJ (2021) A novel electromagnetic guidance ultrasound system on radial artery cannulation: a prospective randomized controlled trial. BMC Anesthesiol 21(1):21
White L, Halpin A, Turner M, Wallace L (2016) Ultrasound-guided radial artery cannulation in adult and paediatric populations: a systematic review and meta-analysis. Br J Anaesth 116(5):610–617
Tangwiwat S, Pankla W, Rushatamukayanunt P, Waitayawinyu P, Soontrakom T, Jirakulsawat A (2016) Comparing the success rate of radial artery cannulation under ultrasound guidance and palpation technique in adults. J Med Assoc Thai 99(5):505–510
Ueda K, Bayman EO, Johnson C, Odum NJ, Lee JJ (2015) A randomised controlled trial of radial artery cannulation guided by Doppler vs. palpation vs. ultrasound. Anaesthesia 70(9):1039–1044
Beyer AT, Ng R, Singh A et al (2013) Topical nitroglycerin and lidocaine to dilate the radial artery prior to transradial cardiac catheterization: a randomized, placebo-controlled, double-blind clinical trial: the PRE-DILATE Study. Int J Cardiol 168(3):2575–2578
Majure DT, Hallaux M, Yeghiazarians Y, Boyle AJ (2012) Topical nitroglycerin and lidocaine locally vasodilate the radial artery without affecting systemic blood pressure: a dose-finding phase I study. J Crit Care 27(5):532.e9–532.13
Jang YE, Ji SH, Kim EH et al (2020) Subcutaneous nitroglycerin for radial arterial catheterization in pediatric patients: a randomized controlled trial. Anesthesiology 133(1):53–63
Varga EQ, Candiotti KA, Saltzman B et al (2013) Evaluation of distal radial artery cross-sectional internal diameter in pediatric patients using ultrasound. Paediatr Anaesth 23(5):460–462
Badal JJ, Kiesau A, Boyle P (2010) Effects of median nerve block on radial artery diameter and peak velocity. Local Reg Anesth 3:5–10
Sinha C, Kumar A, Kumari P, Kumar A, Bhar D, Singh V (2021) Does radial or median nerve blocks affect the area and blood flow of radial artery. Anaesth Crit Care Pain Med 40(2):100831
Quan Z, Tian M, Chi P, Cao Y, Li X, Peng K (2014) Modified short-axis out-of-plane ultrasound versus conventional long-axis in-plane ultrasound to guide radial artery cannulation: a randomized controlled trial. Anesth Analg 119(1):163–169
Goh G, Tan C, Weinberg L (2013) Dynamic ultrasound-guided, short axis, out-of-plane radial artery cannulation: the ‘follow the tip’ technique. Anaesth Intensive Care 41(3):431–432
Ho HH, Jafary FH, Ong PJ (2012) Radial artery spasm during transradial cardiac catheterization and percutaneous coronary intervention: incidence, predisposing factors, prevention, and management. Cardiovasc Revasc Med 13(3):193–195
Yildirim V, Akay HT, Bingol H et al (2007) Pre-emptive stellate ganglion block increases the patency of radial artery grafts in coronary artery bypass surgery. Acta Anaesthesiol Scand 51(4):434–440
Coppola J, Patel T, Kwan T et al (2006) Nitroglycerin, nitroprusside, or both, in preventing radial artery spasm during transradial artery catheterization. J Invasive Cardiol 18(4):155–158
Mehta Y, Juneja R (1994) Continuous axillary block for ischemia following failed radial artery cannulation. J Cardiothorac Vasc Anesth 8(2):257
Scheer B, Perel A, Pfeiffer UJ (2002) Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care 6(3):199–204
Dharma S, Kedev S, Patel T, Kiemeneij F, Gilchrist IC (2015) A novel approach to reduce radial artery occlusion after transradial catheterization: postprocedural/prehemostasis intra-arterial nitroglycerin. Catheter Cardiovasc Interv 85(5):818–825
Ezhumalai B, Satheesh S, Jayaraman B (2014) Effects of subcutaneously infiltrated nitroglycerin on diameter, palpability, ease-of-puncture and pre-cannulation spasm of radial artery during transradial coronary angiography. Indian Heart J 66(6):593–597
Sharma SK, McIntire DD, Wiley J, Leveno KJ (2004) Labor analgesia and cesarean delivery: an individual patient meta-analysis of nulliparous women. Anesthesiology 100(1):142–148 (discussion 6A)
He GW, Yang CQ (1998) Characteristics of adrenoceptors in the human radial artery: clinical implications. J Thorac Cardiovasc Surg 115(5):1136–1141
Abe S, Meguro T, Endoh N et al (2000) Response of the radial artery to three vasodilatory agents. Catheter Cardiovasc Interv 49(3):253–256
Shapira OM, Xu A, Aldea GS, Vita JA, Shemin RJ, Keaney JF Jr. (1999) Enhanced nitric oxide-mediated vascular relaxation in radial artery compared with internal mammary artery or saphenous vein. Circulation 100(19 Suppl):II322–II327
Kim JM, Arakawa K, Bliss J (1975) Arterial cannulation: factors in the development of occlusion. Anesth Analg 54(6):836–841
Nakayama Y, Nakajima Y, Sessler DI et al (2014) A novel method for ultrasound-guided radial arterial catheterization in pediatric patients. Anesth Analg 118(5):1019–1026
Chen Y, Ke Z, **ao J et al (2018) Subcutaneous injection of nitroglycerin at the radial artery puncture site reduces the risk of early radial artery occlusion after transradial coronary Catheterization: a randomized, placebo-controlled clinical trial. Circ Cardiovasc Interv 11(7):e6571
Pancholy SB, Coppola J, Patel T (2006) Subcutaneous administration of nitroglycerin to facilitate radial artery cannulation. Catheter Cardiovasc Interv 68(3):389–391
Gori T, Parker JD (2002) Nitrate tolerance: a unifying hypothesis. Circulation 106(19):2510–2513
Funding
This study was supported by National Health Commission Scientific Research Fund—Major Science and Technology Program of Medicine and Health of Zhejiang Province (grant WKJ-ZJ-1911), the Health Commission of Zhejiang Province (No. 2018KY225) and the Hang Zhou municipal Health Commission (No. A20210287). The funders afforded part of the research fee, but they were not involved in the design of the study, collection, analysis, and interpretation of data and in writing the manuscript.
Author Contribution
ZZf and MX: these authors helped design the study and wrote the paper. WQ and CP: these authors helped perform statistical analysis. SHy, HWs and CY: these authors helped do the work of patient recruitment and data collecting. All authors have read the manuscript and approved the final paper submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
X. Men,Q. Wang, P. Chen, W.‑s. Hu, Y. Chai, H.‑y. Shou and Z.‑f. Zhou declare that they have no competing interests.
This study was approved by The Ethics Committee of Hangzhou Women’s Hospital (IRB:2021-K(9)-02) and written informed consent was obtained from all subjects participating in the study. All methods were performed in accordance with the relevant guidelines and regulations. Clinical trial number and registry URL: ChiCTR2100052981;http://www.chictr.org.cn, Principal investigator: **n Men, date of registration: 7 November2021.
The supplement containing this article is not sponsored by industry.
Additional information
Availability of data and material
The datasets used during the current study are available from the corresponding author on reasonable request.

Scan QR code & read article online
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Men, X., Wang, Q., Chen, P. et al. Subcutaneous nitroglycerin increased the success rate of radial artery cannulation in women with gestational hypertension undergoing cesarean section. Anaesthesiologie 72 (Suppl 1), 28–35 (2023). https://doi.org/10.1007/s00101-023-01264-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-023-01264-6