Abstract
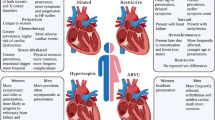
The impact of heart failure on women’s health is only now being fully realized. There has previously been a mistaken belief that heart failure was predominantly a man’s condition. However, research has demonstrated that the causes and treatments of heart failure differ between males and females. Females are exposed to unique stresses on their cardiovascular system (hypertensive disorders of pregnancy, gestational diabetes and chemotherapy for breast cancer) that can ultimately lead to increased risk of heart failure. As well, risk factors such as diabetes can have a larger impact in females as compared to males. Effective treatment for female heart failure patients has been hindered by challenges in accurately diagnosing the disease, the lack of relevant preclinical models, a historic underrepresentation of females in clinical trials and a lack of treatments for heart failure with preserved ejection fraction, the most common form of heart failure in females. Biological differences between males and females can account for some of the differences observed in heart failure outcomes but sex dependent impacts of social determinants of health can also account for some of the adverse outcomes for females with heart failure. In this review we will briefly describe the two major subtypes of heart failure and the use of new biomarkers to more effectively diagnose heart failure. We also discuss four specific risk factors for heart failure that predominantly affect heart failure incidence in females, the impacts of social determinants of health on heart failure risk, and how women may be more adversely impacted by them. Finally, we will propose approaches to narrow the gap in heart failure treatment for females in the future.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Amin HZ, Amin LZ, Pradipta A (2020) Takotsubo cardiomyopathy: a brief review. J Med Life 13(1):3–7. https://doi.org/10.25122/jml-2018-0067
Anaba U, Ishola A, Alabre A, Bui A, Prince M, Okafor H, Kola-Kehinde O, Joseph JJ, Mitchell D, Odei BC, Uzendu A, Williams KP, Capers Q, Addison D (2022) Diversity in modern heart failure trials: where are we, and where are we going. Int J Cardiol 348:95–101. https://doi.org/10.1016/j.ijcard.2021.12.018
Angelini P, Uribe C, Tobis JM (2021) Pathophysiology of takotsubo cardiomyopathy: reopened debate. Texas Heart Inst J 48(3):1–7. https://doi.org/10.14503/THIJ-20-7490
Awadallaa M, Hassana MZO, Alvia RM, Neilan TG (2018) Advanced imaging modalities to detect cardiotoxicity Magid. Curr Probl Cancer 42(4):386–396. https://doi.org/10.1016/j.currproblcancer.2018.05.005.Advanced
Beale AL, Meyer PMD, Marwick TH, Lam CSP, Kaye DM (2018) Sex differences in cardiovascular pathophysiology why women are overrepresented in heart failure with preserved ejection fraction. Circ 138(2):198–205. https://doi.org/10.1161/CIRCULATIONAHA.118.034271
Bhatia RT, Papadakis M (2022) Female sex and persistent inequalities in the care of patients with hypertrophic obstructive cardiomyopathy: a call to action. Eur J Prev Cardiol 29(11):1542–1544
Blenck CL, Harvey PA, Reckelhoff JF, Leinwand LA (2016) The importance of biological sex and estrogen in rodent models of cardiovascular health and disease. Circ Res 118(8):1294–1312
Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. In Nature reviews cardiology, 8(1):30–41. https://doi.org/10.1038/nrcardio.2010.165
Cediel G, Codina P, Spitaleri G, Domingo M, Santiago-Vacas E, Lupón J, Bayes-Genis A (2021) Gender-related differences in heart failure biomarkers. Front Cardiovasc Med 7(January):1–10. https://doi.org/10.3389/fcvm.2020.617705
Cesaroni G, Mureddu GF, Agabiti N, Mayer F, Stafoggia M, Forastiere F, Latini R, Masson S, Davoli M, Boccanelli A, Boccanelli A, Cacciatore G, Mureddu GF, Rizzello V, Agabiti N, Cesaroni G, Forastiere F, Perucci CA, Davoli M et al (2021) Sex differences in factors associated with heart failure and diastolic left ventricular dysfunction: a cross-sectional population-based study. BMC Public Health 21(1):1–13. https://doi.org/10.1186/s12889-021-10442-3
Chandramouli C, Teng THK, Tay WT, Yap J, MacDonald MR, Tromp J, Yan L, Siswanto B, Reyes EB, Ngarmukos T, Yu CM, Hung CL, Anand I, Richards AM, Ling LH, Regensteiner JG, Lam CSP, Anand I, Hung CL et al (2019) Impact of diabetes and sex in heart failure with reduced ejection fraction patients from the ASIAN-HF registry. Eur J Heart Fail 21(3). https://doi.org/10.1002/ejhf.1358
Clayton JA, Collins FS (2014). NIH to balance sex in cell and animal studies. Nat 509(7500). https://doi.org/10.1038/509282a
Dawson DK (2018) Acute stress-induced (takotsubo) cardiomyopathy. Heart 104(2):96–102. https://doi.org/10.1136/heartjnl-2017-311579
de la Fuente A, Santisteban M, Lupón J, Aramendía JM, Díaz A, Santaballa A, Hernándiz A, Sepúlveda P, Cediel G, López B, Picazo JML, Mazo MM, Rábago G, Gavira JJ, García-Bolao I, Díez J, González A, Bayés-Genís A, Ravassa S (2022) A fibrosis biomarker early predicts cardiotoxicity due to anthracycline-based breast cancer chemotherapy. Cancers 14(12):2941. https://doi.org/10.3390/cancers14122941
Dewan P, Rørth R, Jhund PS, Shen L, Raparelli V, Petrie MC, Abraham WT, Desai AS, Dickstein K, Køber L, Mogensen UM, Packer M, Rouleau JL, Solomon SD, Swedberg K, Zile MR, McMurray JJV (2019) Differential impact of heart failure with reduced ejection fraction on men and women. J Am Coll Cardiol 73(1):29–40. https://doi.org/10.1016/j.jacc.2018.09.081
Dewan P, Rørth R, Raparelli V, Campbell RT, Shen L, Jhund PS, Petrie MC, Anand IS, Carson PE, Desai AS, Granger CB, Køber L, Komajda M, McKelvie RS, O'Meara E, Pfeffer MA, Pitt B, Solomon SD, Swedberg K, Zile MR, McMurray JJV (2019) Sex-related differences in heart failure with preserved ejection fraction. Circ Heart Fail 12(12):e006539
Dunlay SM, Pack QR, Thomas RJ, Killian JM, Roger VL (2014) Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med 127(6). https://doi.org/10.1016/j.amjmed.2014.02.008
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602. https://doi.org/10.1038/nrcardio.2017.65
Duprez DA, Gross MD, Kizer JR, Ix JH, Hundley WG, Jacobs DR (2018) Predictive value of collagen biomarkers for heart failure with and without preserved ejection fraction: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Heart Assoc 7(5):13–16. https://doi.org/10.1161/JAHA.117.007885
Echouffo-Tcheugui JB, Guan J, Retnakaran R, Shah BR (2021) Gestational diabetes and incident heart failure: a cohort study. Diabetes Care 44(10). https://doi.org/10.2337/dc21-0552
Fahad Ullah M (2019) Breast cancer: current perspectives on the disease status. Adv Exp Med Biol 1152:51–64. https://doi.org/10.1007/978-3-030-20301-6_4
Farris C, McEnroe-Petittee D, Kanayama T (2014) Takotsubo cardiomyopathy: can hearts really break? Eur Cardiol Rev 32(7):410–414. https://doi.org/10.15420/ecr.2015.10.01.25
Gaggin HK, Januzzi JL (2013) Biomarkers and diagnostics in heart failure. Biochimica et Biophysica Acta—Mol Basis Dis 1832(12)–2442–2450. https://doi.org/10.1016/j.bbadis.2012.12.014
Ghali JK, Krause-Steinrauf HJ, Adams KF, Khan SS, Rosenberg YD, Yancy CW, Young JB, Goldman S, Peberdy MA, Lindenfeld J (2003) Gender differences in advanced heart failure: insights from the BEST study. J Am Coll Cardiol 42(12):2128–2134. https://doi.org/10.1016/j.jacc.2003.05.012
Groenewegen A, Rutten FH, Mosterd A, Hoes AW (2020) Epidemiology of heart failure. Eur J Heart Fail 22(8):1342–1356. https://doi.org/10.1002/ejhf.1858
Hansen AL, Søndergaard MM, Hlatky MA, Vittinghof E, Nah G, Stefanick ML, Manson JAE, Farland, Lv, Wells GL, Mongraw-Chaffin M, Gunderson EP, van Horn L, Wild RA Liu B, Shadyab AH, Allison MA, Liu S, Eaton CB, Honigberg MC, Parikh NI (2021) Adverse pregnancy outcomes and incident heart failure in the women’s health initiative. JAMA Netw Open 4(12):e2138071. https://doi.org/10.1001/jamanetworkopen.2021.38071
Haykowsky MJ, Beaudry R, Brothers RM, Nelson MD, Sarma S, La Gerche A (2016) Pathophysiology of exercise intolerance in breast cancer survivors with preserved left ventricular ejection fraction. Clin Sci 130(24):2239–2244. https://doi.org/10.1042/CS20160479
Honigberg MC, Givertz MM (2019) Peripartum cardiomyopathy. BMJ 364:k5287
Honigberg MC, Riise HKR, Daltveit AK, Tell GS, Sulo G, Igland J, Klungsøyr K, Scott NS, Wood MJ, Natarajan P, Rich-Edwards JW (2020). Heart failure in women with hypertensive disorders of pregnancy: insights from the cardiovascular disease in Norway project. Hypertens 76(5):1506–1513
Iorgoveanu C, Zaghloul A, Ashwath M (2021) Peripartum cardiomyopathy: a review. Heart Fail Rev 26(6):1287–1296. https://doi.org/10.1007/s10741-020-10061-x
Kannel WB, McGee DL (1979) Diabetes and cardiovascular disease: the Framingham study. JAMA: J Am Med Assoc 241(19):2035. https://doi.org/10.1001/jama.1979.03290450033020
Kemp CD, Conte JV (2012) The pathophysiology of heart failure. Cardiovasc Pathol 21(5):365–371. https://doi.org/10.1016/j.carpath.2011.11.007
Khan MS, Shahid I, Siddiqi TJ, Khan SU, Warraich HJ, Greene SJ, Butler J, Michos ED (2020) Ten-year trends in enrollment of women and minorities in pivotal trials supporting recent us food and drug administration approval of novel cardiometabolic drugs. J Am Heart Assoc 9(11). https://doi.org/10.1161/JAHA.119.015594
Khan SU, Khan MZ, Raghu Subramanian C, Riaz H, Khan MU, Lone AN, Khan MS, Benson EM, Alkhouli M, Blaha MJ, Blumenthal RS, Gulati M, Michos ED (2020) Participation of women and older participants in randomized clinical trials of lipid-lowering therapies: a systematic review. JAMA Netw Open 3(5):e205202. https://doi.org/10.1001/jamanetworkopen.2020.5202
Kucharska-Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V (2011) Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the United States and Finland. Ann Epidemiol 21(8). https://doi.org/10.1016/j.annepidem.2011.04.006
Kwak S, Hwang IC, Park JJ, Park JH, Park JB, Cho GY (2021) Sex-specific impact of diabetes mellitus on left ventricular systolic function and prognosis in heart failure. Sci Rep 11(1). https://doi.org/10.1038/s41598-021-91170-x
Lam CSP, Voors AA, De Boer RA, Solomon SD, Van Veldhuisen DJ (2018) Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J 39(30):2780–2792. https://doi.org/10.1093/eurheartj/ehy301
Lenzen MJ, Rosengren A, Scholte op Reimer WJ, Follath F, Boersma E, Simoons ML, Cleland JG, Komajda M (2008) Management of patients with heart failure in clinical practice: differences between men and women. Heart (Br Cardiac Soc) 94(3):1–5. https://doi.org/10.1136/hrt.2006.099523
Lewinter C, Nielsen TH, Edfors LR, Linde C, Bland JM, LeWinter M, Cleland JGF, Køber L, Braunschweig F, Mansson-Broberg A (2022) A systematic review and meta-analysis of beta-blockers and renin-angiotensin system inhibitors for preventing left ventricular dysfunction due to anthracyclines or trastuzumab in patients with breast cancer. Eur Heart J 43(27):2562–2569
López-Vilella R, Marqués-Sulé E, Laymito Quispe R, del P, Sánchez-Lázaro I, Donoso Trenado V, Martínez Dolz L, Almenar Bonet L (2021) The female sex confers different prognosis in heart failure: same mortality but more readmissions. Front Cardiovasc Med 8(Mar):1–8. https://doi.org/10.3389/fcvm.2021.618398
Lu D, Chatterjee S, **ao K, Riedel I, Huang CK, Costa A, Cushman S, Neufeldt D, Rode L, Schmidt A, Juchem M, Leonardy J, Büchler G, Blume J, Gern OL, Kalinke U, Wen Tan WL, Foo R, Vink A, van Laake LW, van der Meer P, Bär C, Thum T (2022) A circular RNA derived from the insulin receptor locus protects against doxorubicin-induced cardiotoxicity. Eur Heart J 43(42):4496–4511
Lyon AR, Citro R, Schneider B, Morel O, Ghadri JR, Templin C, Omerovic E (2021) Pathophysiology of Takotsubo syndrome: JACC state-of-the-art review. J Am Coll Cardiol 77(7):902–921. https://doi.org/10.1016/j.jacc.2020.10.060
Martínez-Sellés M, Doughty RN, Poppe K, Whalley GA, Earle N, Tribouilloy C, McMurray JJV, Swedberg K, Køber L, Berry C, Squire I (2012) Gender and survival in patients with heart failure: interactions with diabetes and aetiology. Results from the MAGGIC individual patient meta-analysis. Eur J Heart Fail 14(5). https://doi.org/10.1093/eurjhf/hfs026
Mensah GA (2021) The implementation frontier: impact on cardiovascular health in racial and ethnic minority populations, pp 35–45. https://doi.org/10.1007/978-3-030-81034-4_5
Mentzer G, Hsich EM (2019) Heart failure with reduced ejection fraction in women. Heart Fail Clin 15(1):19–27. https://doi.org/10.1016/j.hfc.2018.08.003
Mishra S, Kass DA (2015) Cellular and molecular pathobiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 18(6):400–423. https://doi.org/10.1038/s41569-020-00480-6.Cellular
Mosquera PA, San Sebastian M, Waenerlund AK, Ivarsson A, Weinehall L, Gustafsson PE (2016) Income-related inequalities in cardiovascular disease from mid-life to old age in a Northern Swedish cohort: a decomposition analysis. Soc Sci Med 149:135–144
Naaktgeboren WR, Groen WG, Jacobse JN, Steggink LC, Walenkamp AME, van Harten WH, Stuiver MM, Aaronson NK, Aleman BMP, van der Meer P, Schaapveld M, Sonke GS, Gietema JA, van Leeuwen FE, May AM (2022) Physical activity and cardiac function in long-term breast cancer survivors: a cross-sectional study. JACC: Cardio Oncol 4(2):183–191. https://doi.org/10.1016/j.jaccao.2022.02.007
Nair N (2020) Epidemiology and pathogenesis of heart failure with preserved ejection fraction. Rev Cardiovasc Med 21(4):531–540. https://doi.org/10.31083/J.RCM.2020.04.154
O’Kelly AC, Lau ES (2020) Sex differences in HFpEF. Curr Treat Options Cardiovasc Med 22(12). https://doi.org/10.1007/s11936-020-00856-4
Oni-Orisan A, Mavura Y, Banda Y, Thornton TA, Sebro R (2021) Embracing genetic diversity to improve black health. N Engl J Med 384(12):1163–1167
Powell-Wiley TM, Ngwa J, Kebede S, Lu D, Schulte PJ, Bhatt DL, Yancy C, Fonarow GC, Albert MA (2018) Impact of body mass index on heart failure by race/ethnicity from the get with the guidelines–heart failure (GWTG–HF) registry. JACC: Heart Failure 6(3):233–242. https://doi.org/10.1016/j.jchf.2017.11.011
Raafs A, Verdonschot J, Ferreira JP, Wang P, Collier T, Henkens M, Björkman J, Boccanelli A, Clark AL, Delles C, Diez J, González A, Girerd N, Jukema JW, Pinet F, Rossignol P, Thum T, Vodovar N, de Boer RA et al (2021) Identification of sex-specific biomarkers predicting new-onset heart failure. ESC Heart Failure 8(5):3512–3520. https://doi.org/10.1002/ehf2.13476
Rådholm K, Zhou Z, Clemens K, Neal B, Woodward M (2019) Effects of SGLT2 inhibitors in type 2 diabetes, comparing women to men. Diabetes Obes Metab 46(May):1–4
Ramlakhan KP, Johnson MR, Roos-Hesselink JW (2020) Pregnancy and cardiovascular disease. Nat Rev Cardiol 17(11). https://doi.org/10.1038/s41569-020-0390-z
Reding KW, Cheng RK, Barac A, Vasbinder A, Hovsepyan G, Stefanick M, Simon MS (2022). Toward a better understanding of the differential impact of heart failure phenotypes after breast cancer. J Clin Oncol 40(32):3688–3691
Roger VL (2021) Epidemiology of heart failure: a contemporary perspective. Circ Res 128(10):1421–1434. https://doi.org/10.1161/CIRCRESAHA.121.318172
Rosenkaimer S, Sieburg T, Winter L, Mavratzas A, Hofmann WK, Hofheinz RD, Akin I, Duerschmied D, Hohneck A (2022) Adverse cardiovascular effects of anti-tumor therapies in patients with breast cancer: a single-center cross-sectional analysis. Anticancer Res 42(6):3075–3084. https://doi.org/10.21873/anticanres.15795
Saeed A, Kampangkaew J, Nambi V (2017) Prevention of cardiovascular disease in women. Methodist DeBakey Cardiovasc J 13(4):185–192. https://doi.org/10.14797/mdcj-13-4-185
Saiki H, Petersen IA, Scott CG, Bailey KR, Dunlay SM, Finley RR, Ruddy KJ, Yan E, Redfield MM (2018) Women after contemporary radiotherapy for breast cancer. 135(15):1388–1396. https://doi.org/10.1161/CIRCULATIONAHA.116.025434.Risk
Schiattarella GG, Altamirano F, Tong D, French KM, Villalobos E, Kim SY, Luo X, Jiang N, May HI, Wang Zv, Hill TM, Mammen PPA, Huang J, Lee DI, Hahn VS, Sharma K, Kass DA, Lavandero S, Gillette TG, Hill JA (2019) Nitrosative stress drives heart failure with preserved ejection fraction. Nat 568(7752):351–356. https://doi.org/10.1038/s41586-019-1100-z
Schreuder MM, Schuurman A, Akkerhuis KM, Constantinescu AA, Caliskan K, van Ramshorst J, Germans T, Umans VA, Boersma E, Roeters van Lennep JE, Kardys I (2021) Sex-specific temporal evolution of circulating biomarkers in patients with chronic heart failure with reduced ejection fraction. Int J Cardiol 334:126–134. https://doi.org/10.1016/j.ijcard.2021.04.061
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA, Sperling LS (2018) Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circ 137(20):2166–2178. https://doi.org/10.1161/CIRCULATIONAHA.117.029652
Sciomer S, Moscucci F, Salvioni E, Marchese G, Bussotti M, Corrà U, Piepoli MF (2020). Role of gender, age and BMI in prognosis of heart failure. Eur J Prev Cardiol 27(2_suppl):46–51. https://doi.org/10.1177/2047487320961980
Silverman MG, Patel B, Blankstein R, Lima JAC, Blumenthal RS, Nasir K, Blaha MJ (2016) Impact of race, ethnicity, and multimodality biomarkers on the incidence of new-onset heart failure with preserved ejection fraction (from the multi-ethnic study of atherosclerosis). Am J Cardiol 117(9):1474–1481. https://doi.org/10.1016/j.amjcard.2016.02.017
Siu SC, Lee DS, Rashid M, Fang J, Austin PC, Silversides CK (2021) Long-term cardiovascular outcomes after pregnancy in women with heart disease. J Am Heart Assoc 10(11). https://doi.org/10.1161/JAHA.120.020584
Sobhani K, Nieves Castro DK, Fu Q, Gottlieb RA, Van Eyk JE, Noel Bairey Merz C (2018) Sex differences in ischemic heart disease and heart failure biomarkers. Biol Sex Differ 9(1):1–13. https://doi.org/10.1186/s13293-018-0201-y
Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Lindholm D, Wilderäng U, Öhrn F, Claggett B, Langkilde AM, Petersson M, McMurray JJV (2021) Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial. Eur J Heart Fail 23(7). https://doi.org/10.1002/ejhf.2249
Solomon SD, McMurray JJV, Claggett B, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Desai AS, Jhund PS, Belohlavek J, Chiang C-E, Borleffs CJW, Comin-Colet J, Dobreanu D, Drozdz J et al (2022) Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 387(12):1089–1098. https://doi.org/10.1056/NEJMoa2206286
Stirbu I, Looman C, Nijhof GJ, Reulings PG, Mackenbach JP (2012) Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Community Health 66(12). https://doi.org/10.1136/jech-2011-200924
Suthahar N, Lau ES, Blaha MJ, Paniagua SM, Larson MG, Psaty BM, Benjamin EJ, Allison MA, Bartz TM, Januzzi JL, Levy D, Meems LMG, Bakker SJL, Lima JAC, Cushman M, Lee DS, Wang TJ, deFilippi CR, Herrington DM et al (2020) Sex-specific associations of cardiovascular risk factors and biomarkers with incident heart failure. J Am Coll Cardiol 76(12):1455–1465. https://doi.org/10.1016/j.jacc.2020.07.044
Suthahar N, Meems LMG, Ho JE, de Boer RA (2020) Sex-related differences in contemporary biomarkers for heart failure: a review. Eur J Heart Fail 22(5):775–788. https://doi.org/10.1002/ejhf.1771
Tanai E, Frantz S (2016) Pathophysiology of heart failure. Compr Physiol 6(1):187–214. https://doi.org/10.1002/cphy.c140055
Tibrewala A, Yancy CW (2019) Heart failure with preserved ejection fraction in women. Heart Fail Clin 15(1):9–18. https://doi.org/10.1016/j.hfc.2018.08.002
Toma M, Mak GJ, Chen V, Hollander Z, Shannon CP, Lam KKY, Ng RT, Tebbutt SJ, Wilson-McManus JE, Ignaszewski A, Anderson T, Dyck JRB, Howlett J, Ezekowitz J, McManus BM, Oudit GY (2017) Differentiating heart failure phenotypes using sex-specific transcriptomic and proteomic biomarker panels. ESC Heart Fail 4(3):301–311. https://doi.org/10.1002/ehf2.12136
Tong D, Schiattarella GG, Jiang N, May HI, Lavandero S, Gillette TG, Hill JA (2019) Female sex is protective in a preclinical model of heart failure with preserved ejection fraction. Circ 140(21):1769–1771. Lippincott Williams and Wilkins. https://doi.org/10.1161/CIRCULATIONAHA.119.042267
Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, Gottdiener JS, Psaty BM, Vasan RS (2018) Temporal trends in the incidence of and mortality associated with heart failure with preserved and reduced ejection fraction. JACC: Heart Fail 6(8):678–685. https://doi.org/10.1016/j.jchf.2018.03.006
Varghese SS, Johnston WJ, Eekhoudt CR, Keats MR, Jassal DS, Grandy SA (2021) Exercise to reduce anthracycline-mediated cardiovascular complications in breast cancer survivors. Curr Oncol 28(5):4139–4156. https://doi.org/10.3390/curroncol28050351
Wei S, Le N, Zhu JW, Breathett K, Greene SJ, Mamas MA, Zannad F, Van Spall HGC (2022) Factors associated with racial and ethnic diversity among heart failure trial participants: a systematic bibliometric review. Circul Heart Fail 15(3):E008685. https://doi.org/10.1161/CIRCHEARTFAILURE.121.008685
Ma Y, Shi Y, Ma W, Yang D, Hu Z, Wang M, Cao X, Zhang C, Luo X, He S, Zhang M, Duan Y, Cai H (2022) A prospective study on sex differences in functional capacity, quality of life and prognosis in patients with heart failure. Medicine (Baltimore) 101(26):e29795
Youmans QR, Okwuosa IS, Yancy CW (2021) Heart failure in African Americans and Hispanic Americans: a persistent and disproportionate burden in underrepresented minorities. In: Cardiovascular disease in racial and ethnic minority populations, pp 55–74
Yu Y, Arah OA, Liew Z, Cnattingius S, Olsen J, Sørensen HT, Qin G, Li J (2019) Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up. BMJ 367:l6398
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
McBride, J.A.M., Wigle, J.T. (2023). Sex-Dependent Differences in the Diagnosis, Treatment and Causes of Heart Failure. In: Kirshenbaum, L., Rabinovich-Nikitin, I. (eds) Biology of Women’s Heart Health. Advances in Biochemistry in Health and Disease, vol 26. Springer, Cham. https://doi.org/10.1007/978-3-031-39928-2_16
Download citation
DOI: https://doi.org/10.1007/978-3-031-39928-2_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-39927-5
Online ISBN: 978-3-031-39928-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)