Abstract
About 25% of the patients with diabetes will develop diabetic foot ulcers in their lifetime, with an incidence of 2–7% per year. The risk factors that concur to the development of a foot ulcer in diabetic patients are mostly the neuropathic foot and the vascular or ischemic foot. Infection may involve the soft tissues only (cellulitis and phlegmon) or deeper tissues and bone (osteomyelitis).
The techniques for diagnosing osteomyelitis include “probe to bone” probing, standard X-ray, MRI, and bone biopsy with microbiologic culture. Nuclear medicine techniques to diagnose infections in diabetic foot include three-phase bone scintigraphy, scintigraphy with radiolabeled leukocytes, and PET/CT with [18F] FDG.
The 2012 guidelines of the American College of Radiology suggest the use of leukocyte scintigraphy as the first-line nuclear medicine technique to evaluate patients with diabetic foot infection. When relying on single-photon emission imaging, SPECT/CT imaging provides advantages over planar scintigraphy, such as improved spatial resolution, better soft tissue contrast, and more precise anatomical localization of the infection.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
World Health Organization. Global report on diabetes. Geneva, Switzerland: World Health Organization; 2016. https://www.who.int/diabetes/global-report/en/
Armstrong DG, Boulton AJ, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367–75.
Lavery LA, Lavery DC, Hunt NA, La Fontaine J, Ndip A, Boulton AJ. Amputations and foot-related hospitalisations disproportionately affect dialysis patients. Int Wound J. 2015;12:523–6.
Lavery LA, Armstrong DG, Wunderlich RP, Mohler MJ, Wendel CS, Lipsky BA. Risk factors for foot infections in individuals with diabetes. Diabetes Care. 2006;29:1288–93.
Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ. Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care. 2003;26:1435–8.
Boulton AJ, Vileikyte L, Ragnarson Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366:1719–24.
Ince P, Abbas ZG, Lutale JK, Basit A, Ali SM, Chohan F, et al. Use of the SINBAD classification system and score in comparing outcome of foot ulcer management on three continents. Diabetes Care. 2008;31:964–7.
https://iwgdfguidelines.org/wp-content/uploads/2019/05/IWGDF-Guidelines-2019.pdf
NHS. National Diabetes Foot Care Audit third annual report. In: Partnership HQI, editor. https://www.hqip.org.uk/resource/national-diabetes-footcare-audit-third-annual-report-2014-2017.
Bravo-Molina A, Linares-Palomino JP, Vera-Arroyo B, Salmerón-Febres LM, Ros-Díe E. Inter-observer agreement of the Wagner, University of Texas and PEDIS classification systems for the diabetic foot syndrome. Foot Ankle Surg. 2016;24:60–4.
Giurato L, Uccioli L. The diabetic foot: Charcot joint and osteomyelitis. Nucl Med Commun. 2006;27:745–9.
Lavery LA, Ryan EC, Ahn J, Crisologo PA, Oz OK, La Fontaine J, Wukich DK. The infected diabetic foot: re-evaluating the IDSA diabetic foot infection classification. Clin Infect Dis. 2020;70(8):1573–9.
Lipsky BA, Berendt AR, Embil J, De Lalla F. Diagnosing and treating diabetic foot infections. Diabetes Metab Res Rev. 2004;20(Suppl 1):S56–64.
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, et al. Infectious Diseases Society of America. Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54:e132–73.
Filippi L, Uccioli L, Giurato L, Schillaci O. Diabetic foot infection: usefulness of SPECT/CT for 99mTc-HMPAO-labeled leukocyte imaging. J Nucl Med. 2009;50:1042–6.
Tan PL, Teh J. MRI of the diabetic foot: differentiation of infection from neuropathic change. Br J Radiol. 2007;80:939–48.
Palestro CJ, Love C. Nuclear medicine and diabetic foot infections. Semin Nucl Med. 2009;39:52–65.
Capriotti G, Chianelli M, Signore A. Nuclear medicine imaging of diabetic foot infection: results of meta-analysis. Nucl Med Commun. 2009;27:757–64.
Sanders LJ, Frykberg RG. Charcot neuroarthropathy of the foot. In: Levin ME, O’Neal LW, Bowker JH, Pfeifer MA, editors. The diabetic foot. 6th ed. St Louis: Mosby; 2001. p. 439–65.
Butalia S, Palda VA, Sargeant RJ, Detsky AS, Mourad O. Does this patient with diabetes have osteomyelitis of the lower extremity? JAMA. 2008;299:806–13.
Apelqvist J, Bakker K, van Houtum WH, Nabuurs-Franssen MH, Schaper NC. International consensus on the diabetic foot & practical guidelines on the management and prevention of the diabetic foot, by the International Working Group on the Diabetic Foot. Diabetes Metab Res Rev. 2000;16(Suppl 1):s 84–92.
Clohisy DR, Thompson RC Jr. Fractures associated with neuropathic arthropathy in adults who have juvenile-onset diabetes. J Bone Joint Surg Am. 1988;70:1192–200.
Wraight PR, Lawrence SM, Campbell DA, Colman PG. Creation of a multidisciplinary, evidence based, clinical guideline for the assessment, investigation and management of acute diabetes related foot complications. Diabet Med. 2005;22:127–36.
Baglioni P, Malik M, Okosieme OE. Acute Charcot foot. BMJ. 2012;344:e1397.
Tan PL, Teh J. MRI of the diabetic foot: differentiation of infection from neuropathic change. Br J Radiol. 2001;80:939–48.
Palestro CJ, Mehta HH, Patel M, Freeman SJ, Harrington WN, Tomas MB, Marwin SE. Marrow versus infection in the Charcot joint: indium-111 leukocyte and technetium-99m sulfur colloid scintigraphy. J Nucl Med. 1998;39:346–50.
Prandini N, Lazzeri E, Rossi B, Erba P, Parisella MG, Signore A. Nuclear medicine imaging of bone infections. Nucl Med Commun. 2006;27:633–44.
Nawaz A, Torigian DA, Siegelman ES, Basu S, Chryssikos T, Alavi A. Diagnostic performance of FDG-PET, MRI, and plain film radiography (PFR) for the diagnosis of osteomyelitis in the diabetic foot. Mol Imaging Biol. 2010;12:335–42.
Heiba SI, Kolker D, Mocherla B, Kapoor K, Jiang M, Son H, et al. The optimized evaluation of diabetic foot infection by dual isotope SPECT/CT. Imaging protocol. J Foot Ankle Surg. 2010;49:529–36.
Ruiz-Bedoya CA, Gordon O, Mota F, Abhishek S, Tucker EW, Ordonez AA, Jain SK. Molecular imaging of diabetic foot infections: new tools for old questions. Int J Mol Sci. 2019;20(23):5984. https://doi.org/10.3390/ijms20235984.
Eser Sanverdi S, Ergen B, Oznur A. Current challenges in imaging of the diabetic foot. Diabet Foot Ankle. 2012;3 https://doi.org/10.3402/dfa.v3i0.18754.
Beaman FD, von Herrmann PF, Kransdorf MJ, Adler RS, Amini B, Appel M, et al. ACR Appropriateness Criteria® suspected osteomyelitis, septic arthritis, or soft tissue infection (excluding spine and diabetic foot). J Am Coll Radiol. 2017;14:S326–37.
Basu S, Chryssikos T, Houseni M, Scot MD, Shah J, Zhuang H, et al. Potential role of FDG PET in the setting of diabetic neuro-osteoarthropathy: can it differentiate uncomplicated Charcot’s neuroarthropathy from osteomyelitis and soft-tissue infection? Nucl Med Commun. 2007;28:465–72.
Treglia G, Sadeghi R, Annunziata S, Zakavi SR, Caldarella C, Muoio B, et al. Diagnostic performance of fluorine-18-fluorodeoxyglucose positron emission tomography for the diagnosis of osteomyelitis related to diabetic foot: a systematic review and a meta-analysis. Foot (Edinb). 2013;23:140–8.
Lipsky B, Senneville E, Abbas Z, Aragón-Sánchez J, Diggle M, Embil J. Guideline on the diagnosis and treatment of foot infection in persons with diabetes (WGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3280. https://doi.org/10.1002/dmrr.3280.
Familiari D, Glaudemans AW, Vitale V, Prosperi D, Bagni O, Lenza A, et al. Can sequential 18F-FDG PET/CT replace WBC imaging in the diabetic foot? J Nucl Med. 2011;52:1012–9.
Lauri C, Tamminga M, Glaudemans AW, Orozco LEJ, Erba PA, Jutte PC, et al. Detection of osteomyelitis in the diabetic foot by imaging techniques: a systematic review and meta-analysis comparing MRI, white blood cell scintigraphy, and FDG-PET. Diabetes Care. 2017;40:1111–20.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Clinical Cases
Clinical Cases
12.1.1 Case 12.1
A 58-year-old female with history of type 1 diabetes (chronic therapy with insulin). Various amputations in the left foot (third and fourth metatarsal bones); wee** wound in the left foot treated by hyperbaric oxygen therapy and antibiotics (amoxicillin clavulanate + levofloxacin) until 10 days before bone scintigraphy (June 2011).
12.1.1.1 Clinical Presentation
Pain and loss of function of left foot; scar of previous wee** wound; red and swollen skin in left foot.
12.1.1.2 Previous Diagnostic Work-Up
X-rays of left foot; angio-CT and morphologic CT of the left foot; the patient needs a differential diagnosis between Charcot’s foot and osteomyelitis (Figs. 12.10 and 12.11). MRI cannot be performed because of spinal cord implantable stimulator.
12.1.1.3 Suspected Site of Infection
Anterior part of left foot, near previous amputations.
12.1.1.4 Radiopharmaceutical Activity
Bone scan (740 MBq); 99mTc-HMPAO-leukocyte scan (814 MBq).
12.1.1.5 Imaging
Gamma camera type: Gamma camera that combines variable angle dual-detector with a dual slice CT scanner (Symbia-T2); parallel holes collimator (low energy); Zoom: 1; SPECT matrix: 256 × 256. CT slice thickness: 1 mm. Display used for SPECT/CT fusion: 2D orthogonal MPR (multiplanar reformatting) (Figs. 12.12, 12.13, 12.14 and 12.15). Bone scan: (a) early scan (5 min after injection, 300 s) feet laid upon collimator; (b) late scan (3 h after injection, 498 s); leukocyte scan: (a) early scan, pool scan (1 h after injection, scan from pelvis to feet, 617 s); second scan (3 h after injection, scan from pelvis to feet, 928 s); late scan (20 h after injection, scan from pelvis to feet, 1856 s); SPECT/CT (20 h after injection).
12.1.1.6 Conclusion/Teaching Point
Since the patient only had inflammation of the left foot (Charcot’s foot) with no infection, she did not go back to her hyperbaric and antibiotic therapy. She is still well now.
12.1.2 Case 12.2
A 55-year-old male with the history of type 1 diabetes. Several amputations in both the feet; wee** wound in the left foot. Patient underwent no treatment until the examination was performed.
12.1.2.1 Clinical Presentation
Pain and loss of function of the left foot; red and swollen skin in the left foot.
12.1.2.2 Previous Diagnostic Work-Up
A tampon culture was performed; Pseudomonas aeruginosa was found. Patient needs a differential diagnosis, between infection of soft tissues only and osteomyelitis, to develop an appropriate treatment plan.
12.1.2.3 Suspected Site of Infection
Anterior part of the back of left foot, near previous amputations.
12.1.2.4 Radiopharmaceutical Activity
99mTc-HMPAO-leukocyte scintigraphy. Activity injected, 740 MBq.
12.1.2.5 Imaging
Gamma camera type: Gamma camera that combines variable angle dual-detector with a dual slice CT scanner (Symbia-T2); parallel holes collimator (low energy); Zoom, 1; SPECT matrix, 256 × 256; CT slice thickness, 1 mm; display used for SPECT/CT fusion, 2D orthogonal MPR (Figs. 12.16, 12.17, 12.18, and 12.19). Leukocyte scan: (a) early scan, pool scan (1 h after injection, scan from pelvis to feet, 636 s); second scan (3 h after injection, scan from pelvis to feet, 958 s); late scan (20 h after injection, scan from pelvis to feet, 1917 s); SPECT/CT (20 h after injection).
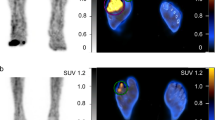
99mTc-HMPAO-leukocyte scintigraphy scan. An increased uptake of leukocytes (inflammation) can be seen (left) that rises and focuses in the 3 h (middle) and 20 h (right) scans in the left foot (signs of septic inflammation, as in osteomyelitis). In the left groin, we can see another spot of leukocytes in the 20 h scan, which may be reactive lymph nodes
12.1.2.6 Conclusion/Teaching Point
Scintigraphy with radiolabeled leukocytes demonstrated osteomyelitis of the second metatarsal bone , in addition to the infection of soft tissues by Pseudomonas aeruginosa. The patient underwent an antibiotic specific therapy (imipenem + cilastatin). Finally, hyperbaric oxygen therapy was performed.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Prandini, N., Bedini, A. (2021). Nuclear Medicine Imaging of Diabetic Foot. In: Lazzeri, E., et al. Radionuclide Imaging of Infection and Inflammation. Springer, Cham. https://doi.org/10.1007/978-3-030-62175-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-62175-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-62174-2
Online ISBN: 978-3-030-62175-9
eBook Packages: MedicineMedicine (R0)