Abstract
Access to health care services is a key concept in the formulation of health policies to improve the population’s health status and to mitigate inequities in health. Previous studies have significantly enhanced our understanding and knowledge of the role played by spatial distribution of health facilities in sustaining population health, with extensive research being devoted to the place-based accessibility theory, with special focus on the gravity-based methods. Although they represent a good starting point to analyse disparities across different regions, the results are not intelligible for policy-making purposes. Given the weaknesses of these methods and the multidimensional nature of the topic, this study intends to: (i) highlight the main measurements of access and their major challenges; and (ii) propose a framework based on multiple criteria decision analysis methods and GIS to appraise the population’s accessibility to health facilities. In particular, this framework is based on a new variant of the UTASTAR method, which requires decision makers and/or experts preference information, in the form of an ordinal ranking, similarly to the UTASTAR method, but to which cardinal information is also added. A numerical example is presented to illustrate the application of the proposed methodology.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
- Accessibility analysis
- Accessibility monitoring
- Multiple Criteria Decision Analysis (MCDA)
- UTASTAR
- Health facilities
1 Introduction
Although health access is not a recent issue in Portugal’s policy [1], only in the last decade has been an increasing effort to achieve the promotion and monitoring of this objective. This situation is transversal to other countries, with the European Commission, the European Council and the European Parliament recognizing access to health care as one of the pillars of social rights in Europe [2]. Within this context, it is critical to have a correct identification of the spatial accessibility to health facilities and having tools to assist analysing how to mitigate spatial inequalities. The inherent complexity given the multidimensional nature of access, as well as the scarcity of information seems to contribute to the weaknesses still present in this topic.
Previous studies have significantly enhanced our understanding of the role played by geographic distribution of healthcare facilities in sustaining population health, with extensive research being devoted to the place-based accessibility theory, with special focus on the gravity-based methods, including the two-step floating catchment area (2SFCA) method. In particular, these models (2SFCA) create an index for each territorial unit, based on a predefined catchment area for health facility and a specific travel time (distance), considering the availability of human resources in health and population contained therein [3]. The incorporation of this type of models in Geographic Information Systems (GIS) – e.g. ArcGIS software – contributed significantly to its dissemination [3]. However, despite being a good starting point for the study of spatial inequalities, many authors argue that the results are not intelligible [4]. As such, the topic remains on the list of priorities for several countries. Thus, this study proposes and describes how the articulation of the Multiple Criteria Decision Analysis (MCDA) methods with the GIS can support in the evaluation of the population's access to health facilities. In particular, the proposed methodology follows the logic of addressing some weaknesses of the mentioned models, exploiting the application of the combined approach of a new variant of the UTA (UTilités Additives) method with the ArcGIS software, to evaluate the spatial accessibility to Primary Health Care (PHC) facilities.
This paper is structured as follows: Sect. 2 presents a brief review of related literature. Section 3 contains the proposed methodology. Section 4 shows an example of application of the proposed methodology, followed by the concluding remarks.
2 Literature Review
The evaluation of geographic healthcare accessibility provides valuable information to public policy. Previous studies on this topic had focused on two dimensions: availability of human resources in health and/or proximity to health facilities [5]. In particular, several national and international studies have shown an uneven distribution of health facilities [2, 3, 6], in which GIS play a key role in the impacts’ measurement of geographic accessibility.
GIS are a spatial analysis tool that allows not only to identify spatial patterns, but also to provide an integrative view of the territory, hel** to make more informed decisions. Recent developments in the scope of spatial access have focused on gravitational models, which provide a joint measure of two components of access [5]: (i) the volume of services provided or human resources considering the population they serve; and (ii) proximity to the healthcare offer points, taking into account the population's location. These models result from a modified version of Newton's Law of Gravity, representing the potential interaction of a population point i to a provider j within a certain distance [7]. Given the computational and programming efforts that this model requires, simpler versions have emerged, such as the 2SFCA models, which generate an index through the definition of the service area of human health resources by a threshold travel time/distance while taking into account the availability of these professionals (e.g. physicians) by their surrounded requirements [8].
The incorporation of this type of models in a GIS environment contributed significantly to its dissemination and use [3]. The scope of these studies mainly focused on the dimensions of availability of human resources and proximity to health facilities [3, 5, 8], however some studies incorporated other dimensions [9, 10]. Although these models serve as a basis for assessing the population's access to health facilities and measuring geographic inequalities, their results, reported as an index, are pointed out as unintuitive and unintelligible [4]. In addition, their users should be aware that they do not respect important theoretical properties and they might generate inconsistencies in the management and planning of the healthcare network, given that:
-
1.
Gravity-based models do not include all the dimensions of access, which make any recommendation unsuitable, no matter how sophisticated the mathematical formulation and analytical assessment tools are. To be useful, the set of criteria/dimensions should be exhaustive, measurable, non-redundant, consensual and as concise as possible [11, 12]. For this reason, structuring the problem is paramount, that is, to identify the criteria on which accessibility should be evaluated according to the literature in the area, knowledge and experience of decision makers (DMs) and other relevant actors. Otherwise, the problem is formulated as if there were only one DM;
-
2.
The scores generated by the index are devoid of absolute meaning, as it is not possible to identify the intrinsic value of the population's accessibility at location i to the health facility j, being just possible to relatively compare the accessibility’s values in locations i and t [13]. In this sense, it does not reveal, for example, the threshold from which accessibility is recommended;
-
3.
Impact (e.g. travel time, patients per physician, among others) is not the same as value [11]. For instance, the difference between 10 and 20 minutes of travel time between population and physician locations may not have the same meaning as the difference between 20 and 30 min. Although, in terms of impact, the difference is the same (10 min), the perception or value may not be equivalent, depending on subjective information coming from experts, citizens and other relevant actors. This conversion of impact into value should not be carried out on an ad hoc basis, and it is essential to collect subjective information through the use of participatory methods [14];
-
4.
There is no reflection about the aggregation mechanism (compensatory versus non-compensatory) of the different criteria, that is, the trade-offs between different criteria are grounded on simplistic mechanisms without discussing the rationale behind them;
-
5.
And above all, the use of these methods can lead to suboptimal resource allocation (e.g., low accessibility’s values typically receive higher priority for treatment and mitigation, which might be inadequate), and there has been little rigorous empirical or theoretical evidence on how well these accessibility’s indices succeed in improving the population's accessibility to health facilities.
In short, despite an increasing interest from academia and organizations in the properly evaluation of the population’s accessibility to health facilities, further theoretical and applied research is needed.
3 Methodological Framework
This study proposes and describes how the articulation of MCDA methods with GIS can be used to improve the evaluation and monitoring of the population's accessibility to PHC units. Although the articulation of MCDA methods with GIS has been little explored in the context of the population’s accessibility to health facilities, in recent years several theoretical and empirical studies have recognized the potential of combining these systems in different sectors [15,16,17,18]. The GIS, in particular ArcGIS 10.5, plays a fundamental role both in the spatial representation of the problem, and in the determination of travel times (or physical distances) between demand and supply points, considering different means of transport. MCDA provides a set of methods with sound theoretical foundations [19] that can be used to evaluate the population’s accessibility to health facilities and help to overcome the weaknesses of gravity-based indices identified in the literature. First, MCDA methods allow for accounting multiple accessibility’s dimensions (proximity, availability, among others). Secondly, they allow for accounting different levels of quantitative and qualitative information of access, as well as for subjective preferences of DMs, which are key features in any evaluation process [19].
The mostly used MCDA methods (e.g. AHP, MACBETH, TOPSIS) are based on direct preferences information which requires from DM a huge amount of subjective preferences. Given the current pandemic context and the limited availability of DM and experts involved in this context, (i.e. health administrators and health professionals with limited availability as frontline soldiers against COVID-19), a novel approach based on a disaggregation model is proposed, requiring a reduced number of judgments from DMs. We believe that this will avoid the risk of triggering rejection by DM, without compromising the model accuracy and quality. Inspired by the UTASTAR method [20], the proposed approach is based on a preference disaggregation model and aims to assess decision models from preference data regarding a list of alternatives.
The methodology proposed in this article consists of the activities presented in Fig. 1, with the evaluation activity described in the next section in greater detail.
3.1 Model Structuring
This activity consists of an interactive learning process between the DMs (health professionals, health administrators, policy makers, among others) in order to: (1) specify the relevant criteria for the DMs; (2) operationalize each criterion; and (3) define the alternatives of comparison. Regarding the former, different strategies and techniques can be used and developed with the DMs (such as cognitive maps and Delphi technique [14]), to identify and describe the relevant criteria for evaluating the population’s accessibility. Secondly, a descriptor of impacts is assigned to each criterion in which is defined a set of plausible impact levels (g), intended to serve as a basis to appraise, as much possible objectively, PHC units’ impact on each criterion. Since this is not the focus of this paper, further details can be consulted in [11].
3.2 Evaluation Model
Main Concepts and Notation.
Consider a MCDA problem characterized by a set of alternatives a, which is valued by a family of criteria C = {C1,…,Cn}. The following notation will be used in the remaining paper:
-
A = {a1,…,am} is the finite set of alternatives;
-
AR is the reference set of alternatives (AR ⊆ A);
-
AH = {aH0, aH1,…aHn} is a set of hypothetical alternatives, where a0 is an hypothetical alternative with the worst impacts in all criteria, and aHi (i = 1,2,…,n) an hypothetical alternative with the best impact in the ith criterion and the worst impacts in all the other criteria, where n is the number of criteria under analysis;
-
aHB is an hypothetical alternative with the best impact in all criteria;
-
The impact scale of the ith criterion varies between gi*, the worst impact level, and gi*, the best impact level;
-
The utility function for the ith criterion, ui, converts impacts (gi) into value ui(gi) in a non-decreasing form, being assigned the value 0 to the worst level and 1 to the best level on each criterion (1). These utility functions are assumed to be piecewise linear, being necessary to divide the interval [gi*, gi*] into αi-1 equal sub-intervals, such that each criterion level gij and ui(gi(a)) are given by (2) and (3), respectively.
$$ u_{i} \left( {g_{i*} } \right) = 0; \, u_{i} \left( {g_{i}^{*} } \right),\forall i = 1,2, \ldots ,n $$(1)$$ g_{i}^{j} = \, g_{i*} + \, \left( {j \, - \, 1} \right)/(\alpha_{i} - \, 1) \times \left( {g_{i}^{*} - \, g_{i*} } \right),\forall j = 1,2, \ldots ,\alpha_{i} $$(2)$$ u_{i} \left( {g_{i} \left( a \right)} \right) \, = \, u_{i} \left( {g_{i}^{j} } \right) \, + \, \left( {g_{i} \left( a \right) \, - \, g_{i}^{j} } \right)/\left( { \, g_{i}^{j + 1} - \, g_{i}^{j} } \right)\times \, [u_{i} \left( {g_{i}^{j + 1} } \right) \, - \, u_{i} \left( {g_{i}^{j} } \right)] $$(3) -
Assuming an additive value model, the aggregated value of an alternative, u(g), is given by the expression (4) in which pi is the weight of criterion i.
$$ u\left( g \right) = \sum\nolimits_{i} p_{i} u_{i} \left( {g_{i} } \right), \, \sum\nolimits_{i} p_{i} = 1 $$(4) -
Let us assume that the reference set of alternatives AR = {aR1 …aRm} is ordered so as aR1 is the best alternative and aRm the worst alternative. The difference of attractiveness between alternatives ak and ak+1, Δ(ak, ak+1), that could be of preference (ak ≻ ak+1) or indifference (ak ~ ak+1), is given by:
$$ \Delta(a_{k} , \, a_{k + 1} ) \, = \, \sum\nolimits_{i}^{n} \{ u_{i} [g_{i} (a_{k} )\left] { \, - \, u_{i} } \right[g_{i} (a_{k + 1} )] \, - \sigma^{ + } \left( {a_{k} } \right) \, + \sigma^{ - } \left( {a_{k} } \right) + \sigma^{ + } \left( {a_{k + 1} } \right) \, - \sigma^{ - } \left( {a_{k + 1} } \right)\}$$(5) -
The monotonicity condition is required (6–7), in which ε is a non-negative indifference threshold to avoid phenomena such as ui (gij+1) = ui (gij) when gij+1 ≻ gij.
$$ u_{i} \left( {g_{i} ^{1} } \right){\rm{ }} = {\rm{ }}0,{\rm{ }}u_{i} \left( {g_{i} ^{j} } \right){\rm{ }} = \sum\nolimits_{{t = 1}}^{j - 1} \;w_{{it}} ,\forall i{\rm{ }} = {\rm{ }}1, \ldots n $$(6)$$ w_{{ij}} = {\rm{ }}u_{i} \left( {g_{i} ^{{j + 1}} } \right){\rm{ }} - {\rm{ }}u_{i} \left( {g_{i} ^{j} } \right) \ge \varepsilon ,\forall i{\rm{ }} = {\rm{ }}1, \ldots n{\rm{ }}and{\rm{ }}j = 1, \ldots ,\alpha _{i} - 1 $$(7)
New Variant of the UTASTAR Algorithm.
Our proposed algorithm is an improvement of the original UTASTAR method, composed by the following activities:
Activity 1: Gathering the Preference Information.
In the UTASTAR method, the preference information given by the DM is elicited in the form of a ranked list of a reference set of alternatives, AR (ordinal information) [20]. Following the suggestion from a previous study, recommending “some additional judgements to perform a number of consistency checks” [21] (p. 228) and with the aim of increasing the model robustness so as to better reflect the DMs’ preferences, this study proposes the use of both ordinal and cardinal information in two steps:
-
In the comparison of the reference set of alternatives AR and aHB, in which the DMs are invited to order and to semantically judge the differences of attractiveness between two consecutive ordered alternatives, based on the seven qualitative categories (null, very weak, weak, moderate, strong, very strong and extreme) proposed in [22];
-
In the comparison of a set of hypothetical alternatives AH to determine the criteria weights, following the MACBETH procedure [22]. This step consists in asking the DMs to (i) order the hypothetical alternatives; and (ii) qualitatively judge the differences of attractiveness between any two consecutive ordered alternatives.
The latter adds to the model more information and concomitantly it is expected that the results will better reflect the DMs’ perspectives and preferences, compared to the ones provided by the UTASTAR model.
Activity 2: Testing for Existing Solutions Compatible with the Preference Information.
The judgments collected in the previous activity are introduced in the algorithm, with the compatibility being verified by means of the linear program 1 (LP1) – Eq. system (8) - represented by an Objective Function (OF), that aims to minimize the sum of overestimation and underestimation errors (σ−(ak) and σ+(ak), respectively) between the calculated and the real utility functions, under constraints that provides enforced properties of the additive utility function:
In which δ represents a small positive number and C a semantic category of difference in attractiveness (with ‘null’ = 0, ‘very weak’ = 1, ‘weak’ = 2, ‘moderate’ = 3, ‘strong’ = 4, ‘very strong’ = 5 and ‘extreme’ = 6).
If the OF is null, there is at least one solution that leads to a perfect representation of the preference information given by the DMs. In the case of a positive OF, other solutions, less good, can improve other relevant criteria, such as Kendall’s [20]. When no solution is found, this is the case of incompatibility, as no value function is compatible with the preference information. In such cases, we recommend the revision of some comparisons in order to obtain a compatible value function, as discussed by Greco [23].
Activity 3: Stability Analysis. This activity consists on a post-optimality analysis problem of the UTASTAR algorithm that aims to exploit the existence of multiple or near solutions of LP1. In particular, it aims to maximize each criterion weight, through the implementation of n objective functions:
grounded by the constraints of the LP1 and bounded by a new constraint:
where γ is a very small positive number and z* is the optimal value of the LP1. The average of the results may be considered as the final solution of the problem.
4 Illustrative Example
In this section, we present a numerical example to illustrate the application of the proposed methodology in the evaluation of the population’s accessibility to PHC units (with focus on the evaluation activities previously described). In particular, this study considers PHC units from Portugal mainland, in which the reference set of alternatives, AR, is composed by four PHC units. Suppose that the DM is interested only in the following criteria of spatial accessibility: (i) General Practitioners (GP) per 10 000 patients; (ii) nurses per 10 000 patients, and (iii) travel time between population and GP locations.
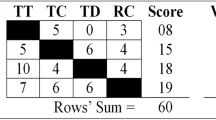
For the illustration of the first activity of the evaluation process, consider Table 1 that reunite data concerning: (i) the impacts of the reference and hypothetical sets of PHC units (AR and AH, respectively) and aHB and (ii) the preference information on the referred sets. For instance, in the comparison of the PHC units from the set AR, the most preferred alternative is A followed by B, C and D. The difference of attractiveness between the considered desirable PHC unit (aHB or I) and A is ‘very weak’, and the difference between A and B is ‘weak’. Regarding the comparison between PHC units from the set AH, three comparisons were elicited between each pair of consecutive ordered alternatives. The data shows that GP per 10 000 patients is the most important criteria, followed by the travel time and nurses per 10 000 patients.
For each criterion, we considered the following breakpoints ordered from the least to the most preferred impact levels.
-
Criterion 1 (GP per 10 000 patients): [1, 2.4, 3.8, 5.2];
-
Criterion 2 (Nurses per 10 000 patients): [1, 2.4, 3.8, 5.2];
-
Criterion 3 (Travel time/ minutes): [61, 41, 21, 1].
Given these impact scales, the utility/value of the PHC units can be determined by linear interpolation (4). For instance:
Then, through the transformation of variables (6), we are able to check for existing solutions compatible with the preference information, by applying LP1 (Table 2) – activity 2.
The results are consistent with the DM’s preferences, with a null OF and concomitantly null over- and underestimation errors. Since the solution is not unique (OF = 0), we proceed to the post-optimality analysis (activity 3) to search for more characteristic solutions, which maximizes the weights of each criterion (10) – LP2. The solutions are present in Table 3, being the average of the three results taken as the most representative solution of the problem.
The final solution leads to the (normalized) utility functions, criteria weights and the aggregated utilities of the PHC units (A-D) presented in Fig. 2. Based on this information, we are able to estimate the aggregated value of the remaining PHC units from Portugal mainland and to spatial represent the results, by using GIS.
5 Concluding Remarks
Evaluation of the spatial accessibility is an under-researched subject, with the complexities involved in the spatial planning and management of health facilities growing as fast or faster than the development of tools and methodologies to manage these challenges in real contexts. This is particularly relevant considering the spread and utilization of gravity-based models, which do not respect important theoretical properties. This study aims to bridge that gap by proposing a novel methodology to improve the evaluation and monitoring of the population’s accessibility to PHC units. In particular, this study proposes a MCDA/GIS-based approach, in which the proposed MCDA method consists on a new variant of the UTASTAR approach.
Compared to other MCDA methods, UTASTAR-based methods are less time-consuming as they require from DMs a lower number of subjective preferences, without compromising the model’s accuracy and quality. This is even more critical considering the current pandemic situation and the limited availability of DMs and experts involved in the context.
The proposed new variant adopts all features of the UTASTAR algorithm and takes additional information into account, in the form of comparisons of intensities of preference between alternatives (cardinal information). Furthermore, the process of gathering the preference information follows the logical of comparing not only a reference set of alternatives, but also a hypothetical set of alternatives in order to determine the criteria weights, according to the MACBETH procedure as suggested by Bana e Costa et al. [22]. Altogether, these will lead to a higher robustness of the model, better reflecting the DMs’ preferences and perspectives, compared to the results provided by the UTASTAR approach.
Within the DRIVIT-UP (DRIVIng forces of urban Transformation: assessing pUblic Policies) project, we are develo** the proposed methods, as well as we are applying them to the evaluation of the population’s spatial accessibility to PHC units in Portugal mainland. The proposed methods follow a socio-technical approach, with the social component being defined by the use of participatory methods to gather preferences and to build a compromise between DMs; and the technical component by the preferences’ modelling. Nevertheless, in this paper we do not cover the social aspects related with the design and use of the proposed methodology. The application of the proposed methods will be supported by decision support systems including several components of the ArcGIS software. We believe that the results of applying the proposed methods to improve the spatial accessibility’s evaluation will correct existing problems in this topic and thus improve the spatial planning of health facilities. Notwithstanding, it is important to highlight some challenges worth for future research:
-
For some spatial accessibility problems/contexts it may be worth investigating the appropriateness of noncompensatory multicriteria models and classification procedures;
-
There are many uncertainties associated with the evaluation of the population’s accessibility, such as uncertainties regarding the measurement of impacts (e.g., imprecise measurement) and of DMs preferences. Few studies have discussed these issues within this context;
-
Finally, it is important to apply the proposed methodology to other contexts (e.g. school accessibility) and to study the extent to which its application translates into better spatial planning and management of the health network, in comparison to the use of gravity-based models.
References
Assembleia da República. Lei n.o 48/1990: Lei de Bases da Saúde. Diário da República. Série I-:3452–9 (1990)
OECD/European Observatory on Health Systems and Policies. Portugal: Perfil de Saúde do País. Paris: OECD Publishing (2017). https://doi.org/10.1787/9789264285385-pt
Luo, W., Whippo, T.: Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 18, 789–795 (2012). https://doi.org/10.1016/j.healthplace.2012.04.002
Lopes, H.S., Ribeiro, V., Remoaldo, P.C.: Spatial accessibility and social inclusion: the impact of Portugal’s last health reform. Geohealth 3, 356–368 (2019). https://doi.org/10.1029/2018GH000165
Gao, F., Kihal, W., Souris, M., Deguen, S.: Assessment of the spatial accessibility to health professionals at French census block level. Int. J. Equity Health 15, 1–14 (2016). https://doi.org/10.1186/s12939-016-0411-z
Ribeiro, V., Remoaldo, P., Gutiérrez, J., Ribeiro, J.C.: Accessibility and GIS on health planning. An approach based on location-allocation models. Acessibilidade e SIG no planeamento em saúde: uma abordagem baseada em modelos de alocação-localização. Rev Port Estud Reg 38 (2015)
Joseph, E., Bantock, P.: Measuring potential physical accessibility to general practitioners in rural areas: a method and case study. Soc. Sci. Med. 16, 85–90 (1982). https://doi.org/10.1016/0277-9536(82)90428-2
Luo, W., Wang, F.: Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 30, 865–884 (2003). https://doi.org/10.1068/b29120
Dai, D., Wang, F.: Geographic disparities in accessibility to food stores in southwest Mississippi. Environ. Plan. B Plan. Des. 38, 659–677 (2011)
Polzin, P., Borges, J., Coelho, A.: An extended kernel density two-step floating catchment area method to analyze access to health care. Environ. Plan. B Plan. Des. 41, 717–735 (2014). https://doi.org/10.1068/b120050p
Keeney, R.L.: Value-Focused Thinking: A Path to Creative Decision making. Harvard University Press, Cambridge (1992)
Bana e Costa, C.A., Beinat, E.: Model-structuring in public decision-aiding, vol. 05.79-Lo (2005)
Blumenthal, A.L.: The Process of Cognition. Prenctice-Hall, Upper Saddle River (1977)
Marttunen, M., Lienert, J., Belton, V.: Structuring problems for multi-criteria decision analysis in practice: a literature review of method combinations. Eur. J. Oper. Res. 263 (2017). https://doi.org/10.1016/j.ejor.2017.04.041
Alzouby, A.M., Nusair, A.A., Taha, L.M.: GIS based multi criteria decision analysis for analyzing accessibility of the disabled in the greater irbid municipality area, Irbid, Jordan. Alexandria Eng. J. 58, 689–698 (2019). https://doi.org/10.1016/j.aej.2019.05.015
Malczewski, J.: Multiple criteria decision analysis and geographic information systems. In: Ehrgott, Matthias, Figueira, José Rui., Greco, Salvatore (eds.) Trends in Multiple Criteria Decision Analysis, pp. 369–395. Springer US, Boston, MA (2010). https://doi.org/10.1007/978-1-4419-5904-1_13
Zucca, A., Sharifi, M., Fabbri, A.: Application of spatial multi-criteria analysis to site selection for a local park: A case study in the Bergamo Province, Italy. J Environ. Manag. 88, 752–769 (2008). https://doi.org/10.1016/j.jenvman.2007.04.026
Cerreta, M., Panaro, S., Poli, G.: A spatial decision support system for multifunctional landscape assessment: A transformative resilience perspective for vulnerable inland areas. Sustainability 13 (2021). https://doi.org/10.3390/su13052748
Belton, V., Stewart, T.: Multiple Criteria Decision Analysis. Springer, Boston (2002). https://doi.org/10.1007/978-1-4615-1495-4
Siskos, Y., Grigoroudis, E., Matsatsinis, N.: UTA methods. Mult. Criteria Decis. Anal. State Art Surv. Int. Ser. Oper. Res. Manag. Sci., pp. 297–343. Springer, New York (2005). https://doi.org/10.1007/0-387-23081-5_8
von Winterfeldt, D., Edwards, W.: Decision Analysis and Behavioral Research. Cambridge University Press, New York (1986)
Bana e Costa, C.A., De Corte, J.M., Vansnick, J.C.: On the mathematical foundation of MACBETH. In: Figueira, J., Greco, S., Ehrogott, M. (eds.) Multiple Criteria Decision Analysis: State of the Art Surveys, pp. 409–437. Springer New York, New York, NY (2005). https://doi.org/10.1007/0-387-23081-5_10
Greco, S., Mousseau, V., Slowinski, R.: Ordinal regression revisited: multiple criteria ranking using a set of additive value functions. Eur. J. Oper. Res. 191, 416–436 (2008). https://doi.org/10.1016/j.ejor.2007.08.013
Acknowledgments
This work is based on the PhD thesis in progress (SFRH/BD/133124/2017), funded by FCT, I.P. (Fundação para a Ciência e a Tecnologia). This work has also been supported by Portuguese national and EU funds through FCT, I.P., in the context of the JUST_PLAN project (PTDC/GES-OUT/2662/20) and the DRIVIT-UP project (POCI-01–0145-FEDER-031905).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this paper
Cite this paper
Lopes, D.F., Marques, J.L., Castro, E.A. (2021). A MCDA/GIS-Based Approach for Evaluating Accessibility to Health Facilities. In: Gervasi, O., et al. Computational Science and Its Applications – ICCSA 2021. ICCSA 2021. Lecture Notes in Computer Science(), vol 12952. Springer, Cham. https://doi.org/10.1007/978-3-030-86973-1_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-86973-1_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-86972-4
Online ISBN: 978-3-030-86973-1
eBook Packages: Computer ScienceComputer Science (R0)