Abstract
Background: Kawasaki disease (KD) is an acute and systemic vasculitis. Its complications in coronary artery aneurysms (CAA) make KD one of the leading causes of acquired cardiovascular diseases in childhood. Low density lipoprotein receptor-related protein 1B (LRP1B) is abundantly expressed in the medial layer of coronary arteries and involved in endothelium inflammations.
Purpose: We aimed to identify the role of LRP1B in CAA formation during KD progression.
Methods: we investigated genetic variations in LRP1B in a Taiwanese cohort of 258 KD patients (83 with CAA and 175 without CAA complications). We used univariate and multivariate regression analyses to identify the associations between LRP1B genetic variations and KD patients.
Results: CAA formation in KD was significantly associated with the LRP1B (rs6707826) genetic variant (p = 0.007). By using multivariate regression analysis, significant correlations were observed between KD with CAA complications and the presence of the TT+TG genotypes for the LRP1B rs6707826 single-nucleotide polymorphism (full model: odds ratio = 2.82; 95% CI = 1.33–5.78).
Conclusion: Our results suggest that genetic polymorphism of LRP1B gene may be used as a genetic marker for the diagnosis and prognosis of the CAA formation in KD and contribute to genetic profiling studies for personalized medicine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Introduction
Kawasaki disease (KD) is a disease in which acute and systemic vasculitis is largely seen in infants and children under five years old [1-5]. The cause of KD is currently unknown, although there is often a pre-existing infection that may play a role in its pathogenesis. During the acute stage of KD, activation of vascular endothelial cells and increased serum levels of proinflammatory cytokines lead to inflammation and injury of blood vessels [6-8]. Coronary artery aneurysms (CAA), which is a complication during the progression of disease, makes KD one of the leading causes for acquired cardiovascular diseases in childhood.
Members of the low density lipoprotein (LDL) receptors family play a variety of roles in normal cell function and development due to their interactions with multiple ligands [9,10]. Histochemical studies have revealed that LDL receptors are markedly induced during progression of atherosclerotic lesions [11]. LDL receptors are highly expressed in smooth muscle cells (SMCs), macrophages and endothelial cells in the lesions. The low density lipoprotein receptor-related protein LRP1B is a new member of LDL receptor subgroup of this gene family. LRP1B is abundantly expressed in the medial layer of coronary arteries and to a lesser extent in thickened intimae [12]. During the acute stage of KD, activation of vascular endothelium cells with increased serum proinflammatory cytokines are involved in vessel inflammation and injury [13, 14]. Injured vascular tissues show subendothelial edema, vascular damage, gap formation, and fenestration of endothelial cells and contribute to the pathogenesis of this disorder. However, it remains unknown if LDL receptor proteins involve in the pathogenesis of KD.
We aimed to identify the role of LRP1B in CAA formation during KD progression by genetic association studies in a Taiwanese cohort of 258 KD patients (83 with CAA and 175 without CAA complications). The study identified LRP1B as a novel susceptibility locus. It is the first time to observe the association between genetic variants of LDL receptor and the CAA formation in KD and contribute to genetic profiling studies for personalized medicine [15].
2. Materials and methods
2.1. Ethical statement
This study was approved by the Human Studies Committee of China Medical University Hospital. Written informed consent was obtained from either the parents or the participants.
2.2. Study subjects
Unrelated individuals fulfilling the diagnostic criteria of KD (n = 258) were identified and enrolled in the study from the Department of Pediatrics at China Medical University Hospital in Taichung, Taiwan [16-20]. A total of 164 males and 94 females with an average age at diagnosis of 1.75 ± 1.61 years were included in the study. All patients were diagnosed according to KD criteria [16, 18], including fever lasting 5 days or more and at least 4 of the following symptoms: (1) changes in extremities (e.g., erythema, edema, or desquamation), (2) bilateral conjunctivitis, (3) polymorphous rash, (4) cervical lymphadenopathy, and (5) changes in lips or oral cavity (e.g., pharyngeal erythema, dry/fissured or swollen lips, strawberry tongue). All patients had regular echocardiography examinations during the acute stage, 2 months after onset, 6 months after onset, and once per year thereafter. CAA was identified when either the right coronary artery or the left coronary artery showed a dilated diameter ≥ 3 mm in children younger than 5 years of age, or ≥ 4 mm in older children [13]. Only Han Chinese individuals, who account for 98% of Taiwanese residents, were recruited. The ethnic background was assigned based on the results of the self-report questionnaires.
2.3. SNP genoty**
Five single-nucleotide polymorphisms (SNPs) from LRP1B were selected from the NCBI SNP database and HAPMAP website (Fig. 1 and Table 1) [21-23]. Selection criteria for including SNPs in the analysis were a minimum allele frequency of >0.05 in the Han Chinese population and Hardy–Weinberg equilibrium (HWE; p > 0.05). A summary of information regarding SNPs in the LRP1B gene (location, position, rs number, and genotype) is listed in Table 1. Briefly, genomic DNA was extracted from peripheral blood leukocytes according to standard protocols (Genomic DNA kit; Qiagen, Hilden, Germany). SNPs were genotyped using a custom-designed VeraCode GoldenGate Genoty** Assay System (Illumina) [24]; genoty** was performed as described at http://www.illumina.com/
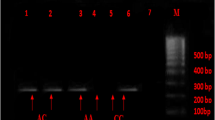
Primers and probes were designed using Custom VeraCode GoldenGate Genoty** Assay System software. Multiplex PCRs were performed with 144-plex VeraCode SNP arrays and genotype analyses were performed using custom 96-plex SAM arrays for 96 samples. Genotype calls were automatically generated using GenCall software version 3.1.3. We assessed 8 VeraCode runs individually for intra-plate inconsistencies, such as variations in fluorescent intensities. Genotype cluster plots generated by individual VeraCode and SAM assays were visually inspected for call quality. Plots that appeared to be “unusually” clustered (i.e., those that did not match the predicted spread in terms of software-generated HWE or distance between clusters [θ]) were investigated further by selecting samples via direct Sanger sequencing for genotype confirmation. Samples were sequenced using Big Dye Terminator v3.1 (AB, Foster City, CA, USA) according to the manufacturer’s guidelines and sequenced using an AB 3730 genetic analyzer.
2.4. Analysis of haplotype blocks
Based on HAPLOVIEW software, we used Lewontin D′ measure to estimate the intermarker coefficient of linkage disequilibrium (LD) of patients [23]. The confidence interval of LD was estimated using a resampling procedure and was used to construct haplotype blocks [25].
2.5. Statistical analysis
Statistical analyses were described previously[26]. Genotypes were obtained by direct counting followed by allele frequency calculations variables, and odds ratios (OR) and 95% confidence intervals (CI) were calculated for the factors under consideration. Forward stepwise multivariate regression analyses were also performed to identify factors contributing independently to CAA formation in KD (Table 2). All statistical analyses were performed using SPSS (v12.0) as described before [26].
3. Results
The genetic location of LRP1B was shown in Fig. 1; all SNPs were in Hardy-Weinberg equilibrium and had a successful genoty** frequency of >99%. The LD structure of this region was also established, with 1 haplotype block determined.
Genotype and genotype frequency data for all five SNPs were shown in Table 1. As shown, a statistically significant difference was observed for the LRP1B (rs6707826) genetic variant (p = 0.007). Frequencies of individuals carrying the TT+TG genotypes of LRP1B (rs6707826) were 86.8% for CAA-positive individuals in contrast to 70.4% for CAA-negative patients. The frequencies of TT and TG combined genotypes were significantly higher in KD with CAA formation (odds ratio = 2.77; 95% CI = 1.33-5.78) compared to those in KD without CAA formation.
To learn the genetic role of LRP1B, we used multivariate regression analyses to determine the associations of clinical characteristics and LRP1B genetic variations in KD. As shown in Table 2, after adjusting for those potential factors, significant associations between KD with CAA complication and the LRP1B (rs6707826) genetic variant was observed. Specifically, significant correlations were found between KD with CAA formation and the presence of the TT+TG genotypes of the LRP1B (rs6707826) SNP (Full model: odds ratio = 2.820; 95% CI = 1.33-5.78).
LRP1B , low density lipoprotein receptor-related protein 1B; IVIG, Intravenous immunoglobulin; CAA, Coronary artery aneurysm; CI, confidence interval. Full model shows results from a logistic regression model including the indicated predictors including Fever duration (days) and 1st IVIG used time (days after the first date with fever).
4. Discussion
In this study, we used a map** strategy focusing on the LRP1B gene and identified a SNP that contributes to the development of CAA formation in Taiwanese KD children of Han Chinese ethnic background. We observed a significant association between the LRP1B gene polymorphism and the occurrence of CAA in KD patients by using multivariate regression analysis. The combined frequency of the TT+TG genotypes of LRP1B (rs6707826) was higher in KD with CAA group than those in KD without CAA group. Our results suggest that LRP1B polymorphism may play a role in the formation of CAA in KD patients.
The genetic association study showed that significant associations between KD with CAA formation and the LRP1B (rs6707826) were still observed by using multivariate regression analysis. The genotypic frequencies harboring one or two copies of T allele were higher in KD patients with CAA formation. These results suggest that the LRP1B gene polymorphism is involved in KD pathogenesis. Patients with one or more copies of T allele at the LRP1B gene tend to develop CAA. This genetic variant is located at the 3′UTR of the LRP1B gene and is putatively involved in posttranscriptional mRNA regulation. In addition, the SNP we identified (rs6707826) showed a linkage disequilibrium with the SNP (rs17760152) (Supplementary Table 1; D′ = 1). LRP1B expression has previously been shown to be significantly associated with the SNP (rs17760152) (p = 0.03996) (http://app3.titan.uio.no/biotools/tool.php?app=snpexp).
The low density lipoprotein receptor gene, LRP1B is located at chromosome 2q22.1 [27]. Its genomic DNA contains 91 exons and spans more than 500 kb. LRP1B protein has four putative ligand-binding domains which bind or endocytose different ligands including urokinase-type plasminogen activator (uPA), tissue-type plasminogen activator (tPA), plasminogen activator inhibitor-1 (PAI-1) and receptor-associated protein (RAP) [9]. In specimens of coronary arteries, LRP1B is clearly observed in intimal and medial smooth muscle cells [12]. The increased expression of LRP1B is shown to attenuate the migration of smooth muscle cells by reducing membrane localization of urokinase and platelet-derived growth factor (PDGF) receptors. LRP1B shares striking similarities to LRP1 protein. Knockout of LRP1 have been also shown to increase the atherosclerotic lesion area and regulate inflammatory responses [28]. Furthermore, studies in the LRP1 genetic variants are associated with an increased risk of coronary artery diseases [29-31]. KD is a multisystemic disorder with the possible underlying pathology of immune-mediated vasculitis and CAA complications [1, 32]. The roles of LRP1B receptor in regulating the vascular inflammation is yet to be investigated. Our data together suggest that LRP1B polymorphism may be involved in the formation of CAA in KD pathogenesis.
In conclusion, our results indicate that LRP1B is significantly associated with the CAA formation in KD progression in Taiwanese children with Han Chinese ethnic background. Genetic polymorphism of LRP1B gene may be used as a genetic marker for the diagnosis and prognosis of the CAA formation in KD.
Acknowledgements
Support for this research was provided by CMU (CMU100-S-01), CMUH (DMR-103-100), and the Republic of China National Science Council (NSC 99-2628-B-039-001- MY3; NSC100-2320-B-039-012-MY3).
References
Burns JC, Glode MP. Kawasaki syndrome. Lancet 2004; 364:533–544.
Kawasaki T. Kawasaki disease: a new disease? Acta Paediatr Taiwan 2001; 42:8–10.
Chang LY, Chang IS, Lu CY, Chiang BL, Lee CY, Chen PJ, et al. Epidemiologic features of Kawasaki disease in Taiwan, 1996-2002. Pediatrics 2004; 114:e678–682.
Burgner D, Davila S, Breunis WB, Ng SB, Li Y, Bonnard C, et al. A genome-wide association study identifies novel and functionally related susceptibility Loci for Kawasaki disease. PLoS Genet 2009; 5:e1000319.
Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 1996; 94:1379–1385.
Gitiaux C, Kossorotoff M, Bergounioux J, Adjadj E, Lesage F, Boddaert N, et al. Cerebral vasculitis in severe Kawasaki disease: early detection by magnetic resonance imaging and good outcome after intensive treatment. Dev Med Child Neurol 2012; 54:1160–1163.
Iannetti L, Zito R, Bruschi S, Papetti L, Ulgiati F, Nicita F, et al. Recent understanding on diagnosis and management of central nervous system vasculitis in children. Clin Dev Immunol 2012; 2012:698327.
Takanashi J, Shirai K, Sugawara Y, Okamoto Y, Obonai T, Terada H. Kawasaki disease complicated by mild encephalopathy with a reversible splenial lesion (MERS). J Neurol Sci 2012; 315:167–169.
Liu CX, Li Y, Obermoeller-McCormick LM, Schwartz AL, Bu G. The putative tumor suppressor LRP1B, a novel member of the low density lipoprotein (LDL) receptor family, exhibits both overlap** and distinct properties with the LDL receptor-related protein. J Biol Chem 2001; 276:28889–28896.
May P, Woldt E, Matz RL, Boucher P. The LDL receptor-related protein (LRP) family: an old family of proteins with new physiological functions. Ann Med 2007; 39:219–228.
Yla-Herttuala S. Expression of lipoprotein receptors and related molecules in atherosclerotic lesions. Curr Opin Lipidol 1996; 7:292–297.
Tanaga K, Bujo H, Zhu Y, Kanaki T, Hirayama S, Takahashi K, et al. LRP1B attenuates the migration of smooth muscle cells by reducing membrane localization of urokinase and PDGF receptors. Arterioscler Thromb Vasc Biol 2004; 24:1422–1428.
Akagi T, Rose V, Benson LN, Newman A, Freedom RM. Outcome of coronary artery aneurysms after Kawasaki disease. J Pediatr 1992; 121:689–694.
Matsubara T, Furukawa S, Yabuta K. Serum levels of tumor necrosis factor, interleukin 2 receptor, and interferon-gamma in Kawasaki disease involved coronary-artery lesions. Clin Immunol Immunopathol 1990; 56:29–36.
Liao WL, Tsai FJ. Personalized medicine: A paradigm shift in healthcare. BioMedicine 2013;3:66–72.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 2004; 114:1708–1733.
Falcini F. Kawasaki disease. Curr Opin Rheumatol 2006; 18:33–38.
Kim S, Dedeoglu F. Update on pediatric vasculitis. Curr Opin Pediatr 2005; 17:695–702.
Wu SF, Chang JS, Wan L, Tsai CH, Tsai FJ. Association of IL-1Ra gene polymorphism, but no association of IL-1beta and IL-4 gene polymorphisms, with Kawasaki disease. J Clin Lab Anal 2005; 19:99–102.
Wu SF, Chang JS, Peng CT, Shi YR, Tsai FJ. Polymorphism of angiotensin-1 converting enzyme gene and Kawasaki disease. Pediatr Cardiol 2004; 25:529–533.
Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 2001; 29:308–311.
Sherry ST, Ward M, Sirotkin K. Use of molecular variation in the NCBI dbSNP database. Hum Mutat 2000; 15:68–75.
Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 2005; 21:263–265.
Tindall EA, Petersen DC, Nikolaysen S, Miller W, Schuster SC, Hayes VM. Interpretation of custom designed Illumina genotype cluster plots for targeted association studies and next-generation sequence validation. BMC Res Notes 2010; 3:39.
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, et al. The structure of haplotype blocks in the human genome. Science 2002; 296:2225–2229.
Bergant M, Banks L. SNX17 facilitates infection with diverse papillomavirus types. J Virol 2013; 87:1270–1273.
Liu CX, Musco S, Lisitsina NM, Yaklichkin SY, Lisitsyn NA. Genomic organization of a new candidate tumor suppressor gene, LRP1B. Genomics 2000; 69:271–274.
Gordts PL, Reekmans S, Lauwers A, Van Dongen A, Verbeek L, Roebroek AJ. Inactivation of the LRP1 intracellular NPxYxxL motif in LDLR-deficient mice enhances postprandial dyslipidemia and atherosclerosis. Arterioscler Thromb Vasc Biol 2009; 29:1258–1264.
Benes P, Muzik J, Benedik J, Elbl L, Vasku A, Siskova L, et al. The C766T low-density lipoprotein receptor related protein polymorphism and coronary artery disease, plasma lipoproteins, and longevity in the Czech population. J Mol Med (Berl) 2001;79:116–120.
Pocathikorn A, Granath B, Thiry E, Van Leuven F, Taylor R, Mamotte C. Influence of exonic polymorphisms in the gene for LDL receptor-related protein (LRP) on risk of coronary artery disease. Atherosclerosis 2003; 168:115–121.
Schulz S, Birkenmeier G, Schagdarsurengin U, Wenzel K, Muller-Werdan U, Rehfeld D, et al. Role of LDL receptor-related protein (LRP) in coronary atherosclerosis. Int J Cardiol 2003; 92:137–144.
Burns JC. Commentary: translation of Dr. Tomisaku Kawasaki’s original report of fifty patients in 1967. Pediatr Infect Dis J 2002; 21:993–995.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Open Access. This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Declaration of Interest: Authors declare no conflicts of interest for this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, YJ., Liu, X., Chang, JS. et al. Coronary artery aneurysms occurrence risk analysis between Kawasaki disease and LRP1B gene in Taiwanese children. BioMed 4, 10 (2014). https://doi.org/10.7603/s40681-014-0010-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.7603/s40681-014-0010-5