Abstract
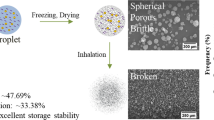
We previously developed a unique four-fluid nozzle spray drier that can produce water-soluble microspheres containing water-insoluble drug nanoparticles in one step without any common solvent between the water-insoluble drug and water-soluble carrier. In the present study, we focused on maltosyl-β-cyclodextrin (malt-β-CD) as a new water-soluble carrier and it was investigated whether drug/malt-β-CD microspheres could improve the bioavailability compared with our previously reported drug/mannitol (MAN) microspheres. The physicochemical properties of bare drug microparticles (ONO-2921, a model water-insoluble drug), drug/MAN microspheres, and drug/malt-β-CD microspheres were evaluated. In vitro aerosol performance, in vitro dissolution rate, and the blood concentration profiles after intratracheal administration were compared between these formulations. The mean diameter of both drug/MAN and drug/malt-β-CD microspheres was approximately 3–5 μm and both exhibited high aerosol performance (>20% in stages 2–7), but drug/malt-β-CD microspheres had superior release properties. Drug/malt-β-CD microspheres dissolved in an aqueous phase within 2 min, while drug/MAN microspheres failed to dissolve in 30 min. Inhalation of drug/malt-β-CD microspheres enhanced the area under the curve of the blood concentration curve by 15.9-fold than that of bare drug microparticles and by 6.1-fold than that of drug/MAN microspheres. Absolute bioavailability (pulmonary/intravenous route) of drug/malt-β-CD microspheres was also much higher (42%) than that of drug/MAN microspheres (6.9%). These results indicate that drug/malt-β-CD microspheres prepared by our four-fluid nozzle spray drier can improve drug solubility and pulmonary delivery.




Similar content being viewed by others
REFERENCES
Merisko-Liversidge E, Liversidge GG, Cooper ER. Nanosizing: a formulation approach for poorly-water-soluble compounds. Eur J Pharm Sci. 2003;18(2):113–20.
Rasenack N, Hartenhauer H, Muller BW. Microcrystals for dissolution rate enhancement of poorly water-soluble drugs. Int J Pharm. 2003;254(2):137–45.
Rasenack N, Muller BW. Dissolution rate enhancement by in situ micronization of poorly water-soluble drugs. Pharm Res. 2002;19(12):1894–900.
Merisko-Liversidge E, Liversidge GG. Nanosizing for oral and parenteral drug delivery: a perspective on formulating poorly-water soluble compounds using wet media milling technology. Adv Drug Deliv Rev. 2011;63(6):427–40.
Nagarwal RC, Kumar R, Dhanawat M, Das N, Pandit JK. Nanocrystal technology in the delivery of poorly soluble drugs: an overview. Curr Drug Deliv. 2011;8(4):398–406.
Shegokar R, Muller RH. Nanocrystals: industrially feasible multifunctional formulation technology for poorly soluble actives. Int J Pharm. 2010;399(1–2):129–39.
Keck CM, Muller RH. Drug nanocrystals of poorly soluble drugs produced by high pressure homogenisation. Eur J Pharm Biopharm. 2006;62(1):3–16.
Kenth S, Sylvestre JP, Fuhrmann K, Meunier M, Leroux JC. Fabrication of paclitaxel nanocrystals by femtosecond laser ablation and fragmentation. J Pharm Sci. 2011;100(3):1022–30.
Dong Y, Ng WK, Hu J, Shen S, Tan RB. A continuous and highly effective static mixing process for antisolvent precipitation of nanoparticles of poorly water-soluble drugs. Int J Pharm. 2010;386(1–2):256–61.
Yamamoto H, Hoshina W, Kurashima H, Takeuchi H, Kawashima Y, Yokoyama T, Tsujimoto H. Engineering of poly(DL-lactic-co-glycolic acid) nanocomposite particles for dry powder inhalation dosage forms of insulin with the spray-fluidised bed granulating system. Adv Powder Tech. 2007;18:2125–228.
Grenha A, Seijo B, Remunan-Lopez C. Microencapsulated chitosan nanoparticles for lung protein delivery. Eur J Pharm Sci. 2005;25(4–5):427–37.
Patomchaiviwat V, Paeratakul O, Kulvanich P. Formation of inhalable rifampicin-poly(L-lactide) microparticles by supercritical anti-solvent process. AAPS PharmSciTech. 2008;9(4):1119–29.
Rodrigues M, Li J, Padrela L, Almeida A, Matos H, Azevedo E. Anti-solvent effect in the production of lysozyme nanoparticles by supercritical fluid-assisted atomization processes. J Supercrit Flu. 2009;48(3):253–60.
Mizoe T, Beppu S, Ozeki T, Okada H. One-step preparation of drug-containing microparticles to enhance the dissolution and absorption of poorly water-soluble drugs using a 4-fluid nozzle spray drier. J Contr Release. 2007;120(3):205–10.
Mizoe T, Ozeki T, Okada H. Preparation of drug nanoparticle-containing microparticles using a 4-fluid nozzle spray drier for oral, pulmonary, and injection dosage forms. J Contr Release. 2007;122(1):10–5.
Mizoe T, Ozeki T, Okada H. Application of a four-fluid nozzle spray drier to prepare inhalable rifampicin-containing mannitol microparticles. AAPS PharmSciTech. 2008;9(3):755–61.
Ohashi K, Kabasawa T, Ozeki T, Okada H. One-step preparation of rifampicin/poly(lactic-co-glycolic acid) nanoparticle-containing mannitol microspheres using a four-fluid nozzle spray drier for inhalation therapy of tuberculosis. J Contr Release. 2009;135(1):19–24.
Ozeki T, Beppu S, Mizoe T, Takashima Y, Yuasa H, Okada H. Preparation of polymeric submicron particle-containing microparticles using a 4-fluid nozzle spray drier. Pharm Res. 2006;23(1):177–83.
Szejtli J, Szente L. Interaction between indometacin and beta-cyclodextrin. Pharmazie. 1981;36(10):694–8.
Frank DW, Gray JE, Weaver RN. Cyclodextrin nephrosis in the rat. Am J Pathol. 1976;83(2):367–82.
Irie T, Otagiri M, Sunada M, Uekama K, Ohtani Y, Yamada Y, Sugiyama Y. Cyclodextrin-induced hemolysis and shape changes of human erythrocytes in vitro. J Pharmacobiodyn. 1982;5(9):741–4.
Holvoet C, Vander Heyden Y, Plaizier-Vercammen J. Inclusion complexation of lorazepam with different cyclodextrins suitable for parenteral use. Drug Dev Ind Pharm. 2005;31(6):567–75.
Rajewski RA, Traiger G, Bresnahan J, Jaberaboansari P, Stella VJ, Thompson DO. Preliminary safety evaluation of parenterally administered sulfoalkyl ether beta-cyclodextrin derivatives. J Pharm Sci. 1995;84(8):927–32.
Tokihiro K, Arima H, Tajiri S, Irie T, Hirayama F, Uekama K. Improvement of subcutaneous bioavailability of insulin by sulphobutyl ether beta-cyclodextrin in rats. J Pharm Pharmacol. 2000;52(8):911–7.
Nishi M, Ishikawa T, Matsumoto Y, Katsube N, Takeishi N, Yonamine H, Matsui T, Okano K, Nakanishi O. Biochemical and physical treatment in rat neuropathic pain and nerve growth factor. Pain Res. 2004;19(4):141–9.
Suzuki A, Omori H, Kinoshita M, Akaike A, Satoh M, Kaneko S. A novel analgesic, ONO-2921, cause a use-dependent inhibition of human N-type (.Alpha.1B) Ca2+ channels and increases inactivated state. Jpn J Pharmacol. 2002;88(1):162.
Komada F, Iwakawa S, Yamamoto N, Sakakibara H, Okumura K. Intratracheal delivery of peptide and protein agents: absorption from solution and dry powder by rat lung. J Pharm Sci. 1994;83(6):863–7.
Weibel ER, Gil J. Structure-function relationship at the alveolar level. In: West JB, editor. Bioengineering Aspects of the Lung. New York: Marcel Dekker; 1977. p. 1–81.
Watanabe M, Ozeki T, Shibata T, Murakoshi H, Takashima Y, Yuasa H, Okada H. Effect of shape of sodium salicylate particles on physical property and in vitro aerosol performance of granules prepared by pressure swing granulation method. AAPS PharmSciTech. 2003;4(4):E64.
European Pharmacopoeia. Section 2.9.18 preparations for inhalation: aerodynamic assessment of fine particles. In EP. 3rd ed. Strasbourg: Council of Europe; 2001.
United States Pharmacopoeia. Chapter 601. Physical tests and determinations: aerosols. 2003. p. 2105–23.
Podczrck P. Optimization of the operation conditions of an Andersen-Cascade impactor and the relationship to centrifugal adhension measurements to aid the development of dry powder inhalations. Int J Pharm. 1997;149:51–61.
Higuchi T, Conners K. Advance in analytical chemistry and instrumentation. New York: CN Reilly Interscience; 1965.
Newman SP, Hollingsworth A, Clark AR. Effect of different modes of inhalation on drug delivery from a dry powder inhaler. Int J Pharm. 1994;102:127–32.
Vidgren M, Karkkainen A, Karjalainen P, Paronen P, Nuutinen J. Effect of powder inhaler design on drug deposition in the respiratory tract. Int J Pharm. 1988;42:211–6.
Okimoto K, Miyake M, Ohnishi N, Rajewski RA, Stella VJ, Irie T, Uekama K. Design and evaluation of an osmotic pump tablet (OPT) for prednisolone, a poorly water soluble drug, using (SBE)7 m-beta-CD. Pharm Res. 1998;15(10):1562–8.
Okimoto K, Rajewski RA, Stella VJ. Release of testosterone from an osmotic pump tablet utilizing (SBE)7 m-beta-cyclodextrin as both a solubilizing and an osmotic pump agent. J Contr Release. 1999;58(1):29–38.
Author information
Authors and Affiliations
Corresponding author
ELECTRONIC SUPPLEMENTARY MATERIAL
Below is the link to the electronic supplementary material.
ESM 1
(PPT 181 kb)
Rights and permissions
About this article
Cite this article
Ozeki, T., Kano, Y., Takahashi, N. et al. Improved Bioavailability of a Water-Insoluble Drug by Inhalation of Drug-Containing Maltosyl-β-Cyclodextrin Microspheres Using a Four-Fluid Nozzle Spray Drier. AAPS PharmSciTech 13, 1130–1137 (2012). https://doi.org/10.1208/s12249-012-9826-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-012-9826-z