Abstract
Background
Clinical severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outcomes could be influenced by genetic polymorphisms in angiotensin I-converting enzyme (ACE1) and ACE2. This study aims to examine three polymorphisms (rs1978124, rs2285666, and rs2074192) on the ACE2 gene and ACE1 rs1799752 (I/D) in patients who have coronavirus disease 2019 (COVID-19) with various SARS-CoV-2 variants.
Methods
Based on polymerase chain reaction-based genoty**, four polymorphisms in the ACE1 and ACE2 genes have been identified in 2023 deceased patients and 2307 recovered patients.
Results
The ACE2 rs2074192 TT genotype was associated with the COVID-19 mortality in all three variants, whereas the CT genotype was associated with the Omicron BA.5 and Delta variants. ACE2 rs1978124 TC genotypes were related to COVID-19 mortality in the Omicron BA.5 and Alpha variants, but TT genotypes were related to COVID-19 mortality in the Delta variant. It was found that ACE2 rs2285666 CC genotypes were associated with COVID-19 mortality in Delta and Alpha variants, and CT genotypes in Delta variants. There was an association between ACE1 rs1799752 DD and ID genotypes in the Delta variant and COVID-19 mortality, whereas there was no association in the Alpha or Omicron BA.5 variants. In all variants of SARS-CoV-2, CDCT and TDCT haplotypes were more common. In Omicron BA.5 and Delta, CDCC and TDCC haplotypes were linked with COVID-19 mortality. In addition to COVID-19 mortality, the CICT, TICT, and TICC were significantly correlated.
Conclusion
The ACE1/ACE2 polymorphisms had an impact on COVID-19 infection, and these polymorphisms had different effects in various SARS-CoV-2 variants. To confirm these results, however, more research needs to be conducted.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in increased mortality and morbidity rates around the globe [1]. With millions of cases confirmed around the world, it will be helpful to know the risk factors and protective factors of COVID-19 infection for the prevention, progression, and unfavorable outcomes of COVID-19 infections. Researchers have identified several risk factors for COVID-19 among adults, including underlying illnesses such as cardiovascular disease, hypertension, and chronic obstructive pulmonary disease, in addition to demographics such as age, ethnicity, gender, and host genetics. Various studies in Iran have evaluated the association of gene polymorphisms involved in SARS-CoV-2 infection, such as interferon lambda 3 and 4 (rs12979860, rs12980275, rs8099917, and rs368234815), tripartite motif containing-22 (rs7113258, rs7935564, and rs1063303), vitamin D receptor gene (ApaI, BsmI, BglI, TaqI, FokI, and Tru9I), interferon-induced transmembrane-protein 3 (rs6598045 and rs12252), transmembrane serine protease 2 (rs12329760), interleukin-10 (rs1800871, rs1800872, and rs1800896), and ABO rs657152 [2,3,4,5,6,7,8,9,10,11,12]. Infection and development of COVID-19 can be prevented with healthy eating habits, adequate nutrition, and COVID-19 vaccination. It has been suggested that these factors can reduce inflammation through increased anti-inflammatory cytokines and decreased expression of angiotensin-converting enzyme-2 (ACE2) [1]. By reducing SARS-CoV-2 binding sites and limiting viral entrance into cells, decreasing ACE2 expression would lead to people less susceptible to the virus. After binding the SARS-CoV-2 to ACE2, the expression of ACE2 is downregulated. However, it should be noted that lack of the positive effects of ACE2 may exacerbate lung injury through a number of different routes [13].
The SARS-CoV-2 enters the cells by the binding of the spike protein to the ACE2 receptor, a key actuator in the renin–angiotensin–aldosterone system (RAAS). Therefore, in COVID-19, RAAS has been directly linked to the development of acute respiratory distress syndrome (ARDS) as part of the host tissue response [14, 15]. However, these same drugs may also be helpful during the inflammation stage of the disease. ACE, ACE2, and AT1R expression has been shown to be altered by chronic treatment with ACE inhibitors [16, 17].
It has been hypothesized that single-nucleotide polymorphisms (SNPs) in the ACE2 gene could affect both its expression and its binding affinity to SARS-CoV-2, affecting both COVID-19 severity and susceptibility to SARS-CoV-2 infection [18, 19]. One of the most extensively studied SNPs in ACE2 is located in the splice region (rs2285666, G>A, Intron 3/4). It has been shown to be associated with coronary heart disease, hypertension, and diabetes associated with stroke [20, 21].
An ACE (17q23.3) is another commonly mentioned gene that produces angiotensin-converting enzyme. It converts angiotensin I (Ang I) to Ang II and activates the AT1R, which has vasoconstrictor, pro-inflammatory, and fibrotic properties [22]. It has also been suggested that COVID-19 may be affected by the deletion/insertion (D/I) of an Alu repeat at the ACE locus (rs1799752, Intron 16) [13]. The serum ACE levels of ACE1 rs1799752 D-allele carriers are considerably higher than those of I-variant carriers. In addition to being associated with an elevated risk of myocardial infarction and left ventricular hypertrophy, the D-allele is a risk factor for onset and progression of ARDS and SARS [20, 23].
There is a possible role for ACE2 rs1978124, located in the intron of chromosome Xp22, in affecting gene function. There is also a link between the ACE2 rs1978124 and dyslipidemia, the risk of diabetes-related left ventricular remodeling, and the severity of COVID-19 [24, 25].
The ACE2 rs2074192 is located in intron 16. Based on analysis of this SNP, rs2074192 is thought to alter donor location and protein features. It has been reported that it is associated with left ventricular hypertrophy [26].
As part of our previous study on the possibility of using a personalized approach in the selection of therapy for COVID-19 patients [3,4,5,6,7,8,9,10,11], we investigated four different SNPs that are relevant to the ACE1 and ACE2 genes and their haplotype combinations in predicting susceptibility to SARS-CoV-2 infection or COVID-19 severity. This prompted us to conduct a pilot study that examined the gene variants of ACE2 rs1978124, rs2285666, and rs2074192 as well as ACE1 rs1799752 (I/D) in individuals with different SARS-CoV-2 variants that were clinically divided into improved and deceased individuals.
Materials and methods
Sample collection
The study involved 4330 patients with COVID-19 recruited from a hospital in Ilam City, Kurdish region, between October 2020 and March 2022 during the three peaks of infection for COVID-19 (Omicron BA.5, Delta, and Alpha).
According to the inclusion criteria, only 4330 patients out of 13,450 cases were selected. There are several inclusion criteria, including being eager to participate in the study, Iranian nationality combined with a common ethnicity, no previous infection or vaccination against COVID-19, being selected from only one hospital, having a positive reverse transcription polymerase chain reaction test result, and no underlying comorbidities, including lung, heart, liver, kidney, cancer, pregnancy, immunocompromised diseases, and obesity, that COVID-19 infection severity could be affected by these factors.
By World Health Organization guidelines, 4330 participants were split into two groups: 2307 recovered COVID-19 patients (outpatients) as control group, and 2023 deceased patients of the same gender and age as case group. In the absence of healthy control subjects, we considered recovered patients with mild and moderate symptoms as controls while deceased patients (inpatients) with severe or critical symptoms were considered cases [27].
We obtained all clinical characteristics upon entering the hospital, including liver enzymes, lipid profiles, uric acid, creatinine, complete blood count (CBC), erythrocyte sedimentation rate (ESR), fasting blood glucose (FBS), C-reactive protein (CRP), 25-hydroxyvitamin D levels, and real-time PCR cycle threshold (Ct) values.
ACE2 SNPs and ACE1 rs1799752 (I/D) genoty**
The total DNA of buffy coat samples was extracted according to manufacturer's instructions using a blood DNA extraction kit (Arman Gene Tajhiz Co.). Then, gel electrophoresis was performed and the DNAs were tested for quality and purity using NanoDrop spectrophotometers (Thermo Scientific, USA).
Genoty** of ACE2 SNPs was performed by polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP). For ACE2 rs1978124 polymorphism, PCR products of 553 bp were amplified using primers f-5′-CAACCACACATACCACAAT-3′ and r-5′-TTTCCTTTAGCCTACAATATCAAT-3′. An overnight treatment with one unit (U) of the Echo471 (Ava II) (Thermo Fisher Scientific™, USA) restriction enzyme was then performed on the PCR product. After digestion, the sizes of the products were 464 and 89 bp for CC genotypes and 553 bp for TT genotypes [27].
To analyze the ACE2 rs2285666 polymorphism, the f-5′-AAACCACTGAAATGACTTACTTACTG-3′ and r-5′-GCCTCACTGTCCTATGACTTTAT-3′ were used to produce 673 bp fragments. In a 16-h digest with 1 U of AluI (Fermentas, Vilnius, Lithuania), PCR products were digested at 37 °C [21]. The product size for TT genotypes was 177 and 496 bp, and for CC genotypes it was 673 bp.
To genotype ACE2 rs2074192, in-house tetra-primer amplification refractory mutation system PCR method was used. With the help of the PRIMER1 website (http://primer1.soton.ac.uk/primer1.html), the outer forward (5′-AAGGGGACACTTAGACAAAATAAAA-3′), outer reverse (5′-GATCCAGAATGTTCTCCATATCAT-3′), inner forward (5′-GTGTGGAAATGTATAAATGGTTTGT-3′) and inner reverse (5′-ACAGCAGTCACAAATGAATAACTG-3′) primers were designed. In order to facilitate accurate differentiation between the two alleles, a mismatched nucleotide was added in the third position from the 3' end terminal of the primers. The result of rs2074192 genotypes was 777 bp + 379 bp for TT genotype and for CC genotype was 777 bp + 447 bp.
The ACE1 rs1799752 intronic Alu insertion (I) or deletion (D) polymorphism was genotyped using PCR with specific primers (f-5′-CTGGAGACCACTCCCATCCTTTCT-3′ and r-5′-GATGTGGCCATCACATTCGTCAGAT-3′). In the DD genotype, the product was 191 bp, in the II genotype, 480 bp, and in the ID genotype, 480 bp + 191 bp [27].
For confirmation of PCR findings, at least 10% of the samples were randomly genotyped using the Sanger sequencing method on an ABI 3500 DX Genetic Analyzer (ABI, Thermo Fisher Scientific, MA, USA). Using Mega Version 11.0 (https://www.megasoftware.net/), the findings were assessed.
Statistical analyses
Statistical analyses were directed using SPSS 22.0. (SPSS. Inc, Chicago, IL, USA). Continuous data were evaluated using the Mann–Whitney test, and numerical variables were reported as mean ± standard deviation (SD). SNP frequencies were expressed as numbers (%) in each group, and Chi-square test was used to analyze the results. The SNPStats software (http://bioinfo.iconcologia.net/SNPStats) was used to assess all genetic models, including dominant, recessive, co-dominant, and over-dominant models of inheritance for four SNPs. Using the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC), the best model was determined. Additionally, using SNPStats, haplotype frequencies were found for ACE1 and ACE2 based on the expectation maximization algorithm. The software SNPStats also determined the Hardy–Weinberg equilibrium (HWE) and the minor allele frequency (MAF). The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to estimate the strength of the association. The analysis was conducted using two-sided tests, and a P value ≤ 0.05 was considered statistically significant. Multiple comparisons were Bonferroni-corrected.
Results
General characteristics of patients
In this study, 4330 patients participated, including 1395 Alpha variant, 1425 Delta variant, and 1510 Omicron BA.5 variant. The mean age of patients with the Alpha, Delta, and Omicron BA.5 variants were 54.7 ± 12.5, 57.3 ± 12.1, and 52.4 ± 13.1, respectively, which was statistically significant. The frequency of deceased patients was 632 (45.3%), 913 (64.1%), and, 478 (31.7%) in the Alpha, Delta, and Omicron BA.5 variants, respectively.
The frequency of ACE2 rs2074192 CC genotype in the Omicron BA.5 variant (54.9%) was higher than both variants and ACE2 rs2074192 TT genotype in the Delta variant (35.1%) was higher than the Alpha (25.9%) and Omicron BA.5 variants (24.8%), which was statistically significant (P < 0.001) (Table 1).
The frequency of ACE2 rs1978124 TT, TC, and CC genotypes in different SARS-CoV-2 variants was tabulated in Table 1. It was statistically significant (P < 0.001) that the frequency of ACE2 rs1978124 TT genotype in the Delta variant (64.4%) was higher than that in both variants, and the frequency of CC genotype in the Omicron BA.5 variant (20.4%) was higher than that in both variants of Alpha (23.9%) and Delta (26.0%).
According to Table 1, the frequency of ACE2 rs2285666 CC genotype in Omicron BA.5 variants (37.7%) was lower than both variants, while the Delta variant's TT genotype (21.1%) was higher than that of Alpha (17.2%) and Omicron BA.5 (12.8%), which was statistically significant (P < 0.001).
Relationship between ACE2 SNPs and ACE1 rs1799752 (I/D) polymorphism and COVID-19 mortality adjusted by SARS-CoV-2 variants
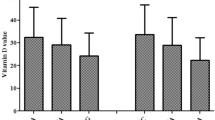
As shown in Fig. 1, the mortality rate of COVID-19 was significantly higher in patients with ACE2 rs2074192 TT (P < 0.001), ACE2 rs2285666 CC (P < 0.001), and ACE1 rs1799752 DD (P < 0.001) genotypes than in those with the other genotypes, while there was no relationship between ACE2 rs1978124 polymorphism and rate of the COVID-19 mortality (P = 0.090).
Table 2 summarizes the results of the inheritance model analysis of ACE2 SNPs and ACE1 rs1799752 (I/D) polymorphisms in the patients. The best-fitting models for all ACE2 SNPs and ACE1 rs1799752 (I/D) were codominant heredity models with the lowest BIC and AIC values. It was shown that ACE2 rs2074192 TT genotypes (P < 0.0001, OR 2.43, 95% CI 2.09–2.83) were associated with a higher risk of COVID-19 mortality. The ACE2 rs1978124 TC genotype (P < 0.0001, OR 1.72, 95% CI 1.41–2.10), ACE2 rs2285666 CC genotype, and ACE1 rs1799752 D/D genotype were related to an increased risk of COVID-19 mortality.
Based upon an adjustment for gender in ACE2 rs2074192, the COVID-19 mortality rate was associated with TT (P < 0.0001, OR 2.28, 95% CI 1.79–2.09) and CT (P < 0.0001, OR 1.54, 95% CI 1.24–1.92) genotypes in female and TT genotype (P < 0.0001, OR 3.05, 95% CI 2.41–3.85) in male patients (Additional file 1: Table S1).
The results of gender adjustment for ACE2 rs1978124 showed an association between the COVID-19 mortality rate and TC genotype (P < 0.0001, OR 1.70, 95% CI 1.38–2.09) in female and TT genotype (P < 0.0001, OR 1.28, 95% CI 1.08–1.52) in male patients (Additional file 1: Table 2).
As mentioned in supplementary Table 3, all genetic correlations were significant after Bonferroni correction.
ACE2 SNPs and ACE1 rs1799752 (I/D) polymorphisms were incompatible with HWE in both recovered and deceased individuals (P < 0.0001). It is important to note that these variants are not found in HWE, which may help to explain why they are associated with the COVID-19 infection.
Distributions of ACE2 SNPs and ACE1 rs1799752 (I/D) polymorphism among SARS-CoV-2 variants
Different variants of the SARS-CoV-2 were closely linked to mortality rate. The Delta and Omicron BA.5 were associated with high and low mortality rates (P < 0.001), respectively.
All three COVID-19 variants were associated with the ACE2 rs2074192 TT genotype after adjusting for SARS-CoV-2 variants with ACE2 rs2074192 genotypes. As for patients infected with the Omicron BA.5 and Delta variants, ACE2 rs2074192 CT genotype was associated with COVID-19 mortality, whereas the Alpha variant did not show the same association (Table 3).
As a result of adjusting SARS-CoV-2 variants with ACE2 rs1978124 genotypes, only the ACE2 rs1978124 TC genotype in the Omicron BA.5 and Alpha variants was related to the mortality of COVID-19, whereas the TT genotype in the Delta variant was related to COVID-19 mortality (Table 3).
When SARS-CoV-2 variants were adjusted for ACE2 rs228566 genotypes, there was an association between the ACE2 rs228566 CC genotype in Delta and Alpha variants and the COVID-19 mortality. Additionally, ACE2 rs2285666 CT genotypes are associated with COVID-19 mortality in patients with Delta variants, but not with Omicron BA.5 variants (Table 3).
As shown in Table 1, the frequency of ACE1 rs1799752 DD genotype in the Delta variant (37.8%) was higher than both variants and II genotype in the Omicron BA.5 variant (23.8%) was higher than the Alpha (21.1%) and Delta variants (21.0%), which was statistically significant (P < 0.001).
A relationship between COVID-19 mortality and the ACE1 rs1799752 DD and ID genotype was found in the Delta variant after adjusting SARS-CoV-2 variants for ACE1 rs1799752 (I/D) genotypes, whereas this relationship did not exist in Alpha and Omicron BA.5 variants (Table 3).
Haplotype analysis
Haplotype analysis was conducted using ACE2 rs2074192, rs1978124, rs2285666 and ACE1 rs1799752 (I/D), and ten significant haplotypes were identified. In all SARS-CoV-2 variants, CDCT and TDCT haplotypes were more common. In Delta and Omicron BA.5 variants, CDCC and TDCC haplotypes were associated with COVID-19 mortality. As reported in Table 4, CICT, TICT, and TICC all showed significant associations with COVID-19 mortality.
Discussion
This comprehensive study evaluated the several SNPs located on ACE1 rs1799752 (I/D) and ACE2 (rs1978124, rs2285666, and rs2074192) genes in a cohort of 4330 Iranian patients positive for different SARS-COV-2 variants, divided into 2307 recovered and 2023 deceased COVID-19 patients.
There was a significant increase in COVID-19 mortality in patients with the ACE2 rs2074192 T allele in this study. The T allele as MAF in the studied patients was 0.39, and it was lower in the recovered patients (0.31) than in the deceased patients (0.48). Other regions in which MAF is found in the NCBI dbSNP database include Asians (0.421), South Asians (0.239), East Asians (0.425), other Asians (0.400), Africans (0.316), African Americans (0.315), Europeans (0.446), and Latin Americans (0.419) (https://www.ncbi.nlm.nih.gov/snp/rs2074192).
In the current study, the ACE2 rs2074192 TT genotype was related to COVID-19 mortality in all three variants. Additionally, the ACE2 rs2074192 CT genotype was associated with COVID-19 mortality in Omicron BA.5 and Delta variant-infected patients, while it was not observed in Alpha variant-infected patients. It is suggested that the T allele is significantly more common in the symptomatic group of the rs2074192 SNP in both females and males as compared to the asymptomatic ones [28]. The findings of this study are also consistent with the findings of a recent large analysis of 1644 COVID-19 patients from the UK Biobank, which showed that the T allele is associated with worse outcomes from SARS-COV2 infection [29].
COVID-19 severity is associated with comorbidities such as cardiovascular risk, retinopathy in people with hypertension, type-2 diabetes, and hypertensive left ventricular hypertrophy in people with the T variant of the rs2074192 polymorphism [26, 30].
It is known that circulating Ang (1–7) levels in hypertensive females can be influenced by the rs2074192 polymorphism [31]. Since this SNP is intronic, it is unlikely to have an impact on the ACE2 protein sequence and, consequently, the effectiveness of the binding between the SARS-CoV-2 Spike protein and the ACE2 receptor. It is necessary to conduct functional studies to validate the effect of this variant on the expression of the ACE2 receptor and the accessibility of the receptor for SARS-COV-2 infection [32].
In this study, mortality rate of COVID-19 was significantly higher among patients with the T allele of ACE2 rs1978124. According to the data, the T allele frequency was 0.68. This amount in the other regions was identified in Asian (0.20), South Asian (0.78), East Asian (0.14), other Asian (0.30), African (0.261), African American (0.261), European (0.625), and Latin American (0.744) (https://www.ncbi.nlm.nih.gov/snp/rs1978124).
This study showed that the TC genotype of ACE2 rs1978124 in the Omicron BA.5 and Alpha variants was in association with COVID-19 mortality, whereas the TT genotype in the Delta variant was in association with COVID-19 mortality. As well, TC genotype was associated with a lower COVID-19 mortality rate in females and TT genotype with a higher COVID-19 mortality rate in males after adjusting for gender. SNPs rs2074192 and rs1978124 have protective effects on females based on genotype frequencies. Notably, the ACE2 gene is on the X chromosome, making heterozygosity in males impossible.
Due to this, SNPs with their single copy may cause the worst outcomes in males [33]. In a study involving females, heterozygosity for the ACE2 rs1978124 was associated with disease severity and it counts as a protective factor in females [25]. It also found that the ACE2 rs1978124 T allele was independently correlated with higher mortality among people with acute coronary syndrome [34].
In this study, COVID-19 mortality was significantly higher in patients with the ACE2 rs2285666 C allele, which is consistent with previous studies [20, 21, 35]. The frequency of the C allele was 0.52. This amount in the other regions was identified in Asian (0.446), South Asian (0.494), East Asian (0.438), other Asian (0.480), African (0.768), African American (0.765), European (0.796), and Latin American (0.624) (https://www.ncbi.nlm.nih.gov/snp/rs2285666).
COVID-19 mortality was associated with the ACE2 rs2285666 CC genotype in the Alpha and Delta variants of this study. Additionally, the ACE2 rs2285666 CT genotype was associated with COVID-19 mortality in Delta variant patients, but not with Omicron BA.5. Several reports indicate that the CC genotype at the ACE2 rs2285666 increases the risk of contracting SARS-CoV-2. It was not possible to determine how this SNP affected COVID-19 severity or the COVID-19 mortality rates [36, 37]. In contrast to similar studies, this study examined a larger number of samples and included a different variant of SARS-CoV-2 than comparable studies. It should be noted that the racial factor should not be ignored because the results of the studies conducted in Iran were similar to our study [21, 35]. Also, in an Italian cohort indicated that there is no consistent correlation of ACE2 variants with COVID-19 severity. It has speculated that rare susceptibility or resistant genotypes could be located in the non-coding regions of ACE2 gene, known to play an important role in regulation of the gene activity [38].
The results of this study revealed that the ACE1 rs1799752 DD and ID genotypes in the Delta variant were associated with COVID-19 mortality; however, the relationship was not found in the Alpha or Omicron BA.5 variants. The ACE1 rs1799752 D-alleles are thought to affect how the SARS-CoV-2 entry receptor is expressed in the alveoli, and consequently how well it can infiltrate and cause disease [39].
Evidence suggests a negative correlation between the prevalence of the ACE1 rs1799752 D allele and COVID-19 incidence. Furthermore, the frequency of the D allele was strongly associated with COVID-19-related mortality [40]. A review of ACE1 rs1799752 (I/D) polymorphisms indicates that individuals with the DD genotype of COVID-19 may suffer severe lung damage [41].
Because ACE1 rs1799752 (I/D) and ACE2 rs1978124 are located in non-coding regions, they are unlikely to be functional polymorphisms. According to earlier research, the ACE1 rs1799752 (I/D) polymorphism alters the balance of ACE1/ACE2, affecting serum and tissue levels of ACE1 protein. Approximately 50% of ACE function is attributed to the ACE1 rs1799752 (I/D) polymorphism. Inflammation can be exacerbated by increased ACE activity, which increases angiotensin II levels [42].
This study offers new insight into the effect of polymorphisms in the ACE1/ACE2 genes on COVID-19 mortality rates caused by different SARS-CoV-2 variants. There is still much to learn about the different behavior of different genotypes of these genes towards different SARS-CoV-2 variants, which deserves greater research and attention.
Several limitations accompanied this study. The frequency of these polymorphisms among healthy people without a previous history of COVID-19 infection could not be compared to that among patients due to the lack of healthy individuals with no history of COVID-19 infection. The absence of measuring serum ACE levels was another limitation of this study. Moreover, since this study was conducted among an ethnic group in Iran, more studies should be conducted with different ethnic groups to confirm these findings.
In conclusion, the finding of this study showed that the ACE2 rs2074192 TT genotype in all three variants, the ACE2 rs2074192 TC genotype in the Alpha and Omicron BA.5 variants and TT genotype in the Delta variant, the ACE2 rs2285666 CC genotype in the Alpha and Delta variants and ACE2 rs2285666 CT genotype in patients infected with the Delta variant was associated with the COVID-19 mortality. Also, the ACE1 rs1799752 DD and ID genotypes in the Delta variant were associated with the COVID-19 mortality, while this relationship was not found in the Alpha and Omicron BA.5 variants. In order to confirm the results of this study, more research should be conducted in other places.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Zhang J, Dong X, Liu G, Gao Y. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2023;64:90–107.
Fauci AS, Lane HC, Redfield RR. Covid-19—navigating the uncharted. N Engl J Med. 2020;382:1268–9.
Raheem Juhi Al-Kaabi N, Khameneh SC, Montazeri M, Mardasi M, Amroabadi JM, Sakhaee F, Fateh A. On the relationship between tripartite motif-containing 22 single-nucleotide polymorphisms and COVID-19 infection severity. Hum Genom. 2022;16:1–8.
Rahimi P, Tarharoudi R, Rahimpour A, Mosayebi Amroabadi J, Ahmadi I, Anvari E, Siadat SD, Aghasadeghi M, Fateh A. The association between interferon lambda 3 and 4 gene single-nucleotide polymorphisms and the recovery of COVID-19 patients. Virol J. 2021;18:1–7.
Gholami M, Sakhaee F, Sotoodehnejadnematalahi F, Zamani MS, Ahmadi I, Anvari E, Fateh A. Increased risk of COVID-19 mortality rate in IFITM3 rs6598045 G allele carriers infected by SARS-CoV-2 delta variant. Hum Genom. 2022;16:1–9.
Mirzaei Gheinari F, Sakhaee F, Gholami M, Sotoodehnejadnematalahi F, Zamani MS, Ahmadi I, Anvari E, Fateh A. ABO rs657152 and blood groups are as predictor factors of COVID-19 mortality in the Iranian population. Dis Markers. 2022;2022:1–8.
Al-Gharrawi ANR, Anvari E, Fateh A. Association of ApaI rs7975232 and BsmI rs1544410 in clinical outcomes of COVID-19 patients according to different SARS-CoV-2 variants. Sci Rep. 2023;13:3612.
Beheshti Shirazi SS, Sakhaee F, Sotoodehnejadnematalahi F, Zamani MS, Ahmadi I, Anvari E, Fateh A. rs12329760 polymorphism in transmembrane serine protease 2 gene and risk of coronavirus disease 2019 mortality. BioMed Res Int. 2022;2022:7841969.
Ahmadi I, Afifipour A, Sakhaee F, Zamani MS, Gheinari FM, Anvari E, Fateh A. Impact of interferon-induced transmembrane protein 3 gene rs12252 polymorphism on COVID-19 mortality. Cytokine. 2022;157:155957.
Albu-Mohammed WHM, Anvari E, Fateh A. Evaluating the role of BglI rs739837 and TaqI rs731236 polymorphisms in vitamin D receptor with SARS-CoV-2 variants mortality rate. Genes. 2022;13:2346.
Abbood SJA, Anvari E, Fateh A. Association between interleukin-10 gene polymorphisms (rs1800871, rs1800872, and rs1800896) and severity of infection in different SARS-CoV-2 variants. Hum Genom. 2023;17:19.
Shawi HRS, Anvari E, Fateh A. Role of FokI rs. 2228570 and Tru9I rs. 757343 polymorphisms in the mortality of patients infected with different variants of SARS-CoV-2. Arch Med Res. 2023;54:310–8.
Gemmati D, Bramanti B, Serino ML, Secchiero P, Zauli G, Tisato V. COVID-19 and individual genetic susceptibility/receptivity: role of ACE1/ACE2 genes, immunity, inflammation and coagulation. Might the double X-chromosome in females be protective against SARS-CoV-2 compared to the single X-chromosome in males? Int J Mol Sci. 2020;21:3474.
Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94:e00127-00120.
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui DS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20.
Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–4.
Sommerstein R, Kochen MM, Messerli FH, Gräni C. Coronavirus disease 2019 (COVID-19): do angiotensin-converting enzyme inhibitors/angiotensin receptor blockers have a biphasic effect? J Am Heart Assoc. 2020;9:e016509.
Darbani B. The expression and polymorphism of entry machinery for COVID-19 in human: juxtaposing population groups, gender, and different tissues. Int J Environ Res Public Health. 2020;17:3433.
Hou Y, Zhao J, Martin W, Kallianpur A, Chung MK, Jehi L, Sharifi N, Erzurum S, Eng C, Cheng F. New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis. BMC Med. 2020;18:1–8.
Möhlendick B, Schönfelder K, Breuckmann K, Elsner C, Babel N, Balfanz P, Dahl E, Dreher M, Fistera D, Herbstreit F. ACE2 polymorphism and susceptibility for SARS-CoV-2 infection and severity of COVID-19. Pharmacogenet Genom. 2021;31:165–71.
Khalilzadeh F, Sakhaee F, Sotoodehnejadnematalahi F, Zamani MS, Ahmadi I, Anvari E, Fateh A. Angiotensin-converting enzyme 2 rs2285666 polymorphism and clinical parameters as the determinants of COVID-19 severity in Iranian population. Int J Immunogenet. 2022;49:325–32.
Tikellis C, Thomas M. Angiotensin-converting enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease. Int J Pept. 2010;2012:1–8.
Adamzik M, Frey U, Sixt S, Knemeyer L, Beiderlinden M, Peters J, Siffert W. ACE I/D but not AGT (-6) A/G polymorphism is a risk factor for mortality in ARDS. Eur Respir J. 2007;29:482–8.
Patel SK, Velkoska E, Freeman M, Wai B, Lancefield TF, Burrell LM. From gene to protein—experimental and clinical studies of ACE2 in blood pressure control and arterial hypertension. Front Physiol. 2014;5:227.
Sabater Molina M, Nicolás Rocamora E, Bendicho AI, Vázquez EG, Zorio E, Rodriguez FD, Gil Ortuño C, Rodríguez AI, Sánchez-López AJ, Jara Rubio R. Polymorphisms in ACE, ACE2, AGTR1 genes and severity of COVID-19 disease. PLoS ONE. 2022;17:e0263140.
Fan Z, Wu G, Yue M, Ye J, Chen Y, Xu B, Shu Z, Zhu J, Lu N, Tan X. Hypertension and hypertensive left ventricular hypertrophy are associated with ACE2 genetic polymorphism. Life Sci. 2019;225:39–45.
Faridzadeh A, Mahmoudi M, Ghaffarpour S, Zamani MS, Hoseinzadeh A, Naghizadeh MM, Ghazanfari T. The role of ACE1 I/D and ACE2 polymorphism in the outcome of Iranian COVID-19 patients: a case-control study. Front Genet. 2022;13:955965.
Cafiero C, Rosapepe F, Palmirotta R, Re A, Ottaiano MP, Benincasa G, Perone R, Varriale E, D’amato G, Cacciamani A. Angiotensin system polymorphisms’ in SARS-CoV-2 positive patients: assessment between symptomatic and asymptomatic patients: a pilot study. Pharmacogenom Personal Med. 2021;14:621–9.
Hamet P, Pausova Z, Attaoua R, Hishmih C, Haloui M, Shin J, Paus T, Abrahamowicz M, Gaudet D, Santucci L. SARS–CoV-2 receptor ACE2 gene is associated with hypertension and severity of COVID 19: interaction with sex, obesity, and smoking. Am J Hypertens. 2021;34:367–76.
Liu C, Li Y, Guan T, Lai Y, Shen Y, Zeyaweiding A, Zhao H, Li F, Maimaiti T. ACE2 polymorphisms associated with cardiovascular risk in Uygurs with type 2 diabetes mellitus. Cardiovasc Diabetol. 2018;17:1–11.
Chen Y, Zhang P, Zhou X, Liu D, Zhong J, Zhang C, ** L, Yu H. Relationship between genetic variants of ACE 2 gene and circulating levels of ACE 2 and its metabolites. J Clin Pharm Ther. 2018;43:189–95.
Bosso M, Thanaraj TA, Abu-Farha M, Alanbaei M, Abubaker J, Al-Mulla F. The two faces of ACE2: the role of ACE2 receptor and its polymorphisms in hypertension and COVID-19. Mol Ther Methods Clin Dev. 2020;18:321–7.
Walls AC, Park Y-J, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(281–292):e286.
Palmer BR, Jarvis MD, Pilbrow AP, Ellis KL, Frampton CM, Skelton L, Yandle TG, Doughty RN, Whalley GA, Ellis CJ. Angiotensin-converting enzyme 2 A1075G polymorphism is associated with survival in an acute coronary syndromes cohort. Am Heart J. 2008;156:752–8.
Alimoradi N, Sharqi M, Firouzabadi D, Sadeghi MM, Moezzi MI, Firouzabadi N. SNPs of ACE1 (rs4343) and ACE2 (rs2285666) genes are linked to SARS-CoV-2 infection but not with the severity of disease. Virol J. 2022;19:48.
Gómez J, Albaiceta GM, García-Clemente M, López-Larrea C, Amado-Rodríguez L, Lopez-Alonso I, Hermida T, Enriquez AI, Herrero P, Melón S. Angiotensin-converting enzymes (ACE, ACE2) gene variants and COVID-19 outcome. Gene. 2020;762:145102.
Karakaş Çelik S, Çakmak Genç G, Pişkin N, Açikgöz B, Altinsoy B, Kurucu İşsiz B, Dursun A. Polymorphisms of ACE (I/D) and ACE2 receptor gene (Rs2106809, Rs2285666) are not related to the clinical course of COVID-19: a case study. J Med Virol. 2021;93:5947–52.
Novelli A, Biancolella M, Borgiani P, Cocciadiferro D, Colona VL, D’Apice MR, Rogliani P, Zaffina S, Leonardis F, Campana A. Analysis of ACE2 genetic variants in 131 Italian SARS-CoV-2-positive patients. Hum Genom. 2020;14:1–6.
Jacobs M, Lahousse L, Van Eeckhoutte HP, Wijnant SR, Delanghe JR, Brusselle GG, Bracke KR. Effect of ACE1 polymorphism rs1799752 on protein levels of ACE2, the SARS-CoV-2 entry receptor, in alveolar lung epithelium. ERJ Open Res. 2021;7:00940–2020.
Delanghe JR, Speeckaert MM, De Buyzere ML. The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clin Chim Acta Int J Clin Chem. 2020;505:192.
Zheng H, Cao JJ. Angiotensin-converting enzyme gene polymorphism and severe lung injury in patients with coronavirus disease 2019. Am J Pathol. 2020;190:2013–7.
Osadnik T, Strzelczyk JK, Fronczek M, Bujak K, Reguła R, Gonera M, Gawlita M, Kurek A, Wasilewski J, Lekston A. Relationship of the rs1799752 polymorphism of the angiotensin-converting enzyme gene and the rs699 polymorphism of the angiotensinogen gene to the process of in-stent restenosis in a population of Polish patients with stable coronary artery disease. Adv Med Sci. 2016;61:276–81.
Acknowledgements
We would like to thank all of the patients who participated in the study.
Author information
Authors and Affiliations
Contributions
FSH, SSM and FS: performed the experiments and manuscript preparation; IA and EA: clinical sample and data acquisition; MSH, ST, and MGJ: analyzed and interpreted data; AF: wrote the paper and supervised the research. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Pasteur Institute of Iran Ethical Committee, Tehran, Iran, authorized the pilot study and it was carried out in accordance with institutional policies. A written informed consent was obtained from all patients who voluntarily participated in the research. All procedures adhered to the values outlined in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Table S1:
ACE2 rs2074192 and sex cross-classification interaction. Table 2: ACE2 rs1978124 and sex cross-classification interaction. Table S3: Bonferroni-corrected test for all SNPs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sheikhian, F., Sadeghi Mofrad, S., Tarashi, S. et al. The impact of ACE2 polymorphisms (rs1978124, rs2285666, and rs2074192) and ACE1 rs1799752 in the mortality rate of COVID-19 in different SARS-CoV-2 variants. Hum Genomics 17, 54 (2023). https://doi.org/10.1186/s40246-023-00501-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40246-023-00501-8