Abstract
Background
SARS-CoV-2 caused a pandemic and global threat for human health. Presence of liver injury was commonly reported in patients with coronavirus disease 2019 (COVID-19). However, reports on severe liver dysfunction (SLD) in critically ill with COVID-19 are lacking. We evaluated the occurrence, clinical characteristics and outcome of SLD in critically ill patients with COVID-19.
Methods
Clinical course and laboratory was analyzed from all patients with confirmed COVID-19 admitted to ICU of the university hospital. SLD was defined as: bilirubin ≥ 2 mg/dl or elevation of aminotransferase levels (> 20-fold ULN).
Results
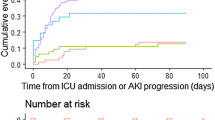
72 critically ill patients were identified, 22 (31%) patients developed SLD. Presenting characteristics including age, gender, comorbidities as well as clinical presentation regarding COVID-19 overlapped substantially in both groups. Patients with SLD had more severe respiratory failure (paO2/FiO2: 82 (58–114) vs. 117 (83–155); p < 0.05). Thus, required more frequently mechanical ventilation (95% vs. 64%; p < 0.01), rescue therapies (ECMO) (27% vs. 12%; p = 0.106), vasopressor (95% vs. 72%; p < 0.05) and renal replacement therapy (86% vs. 30%; p < 0.001). Severity of illness was significantly higher (SAPS II: 48 (39–52) vs. 40 (32–45); p < 0.01). Patients with SLD and without presented viremic during ICU stay in 68% and 34%, respectively (p = 0.002). Occurrence of SLD was independently associated with presence of viremia [OR 6.359; 95% CI 1.336–30.253; p < 0.05] and severity of illness (SAPS II) [OR 1.078; 95% CI 1.004–1.157; p < 0.05]. Mortality was high in patients with SLD compared to other patients (68% vs. 16%, p < 0.001). After adjustment for confounders, SLD was independently associated with mortality [HR3.347; 95% CI 1.401–7.999; p < 0.01].
Conclusion
One-third of critically ill patients with COVID-19 suffer from SLD, which is associated with high mortality. Occurrence of viremia and severity of illness seem to contribute to occurrence of SLD and underline the multifactorial cause.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) caused by novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is responsible for a global threat for human health. Since its initial detection in Wuhan (China) in December 2019 COVID-19 spread and accounts for the ongoing pandemic with more than 30 million infections and 900.000 deaths [1, 2]. The disease is mainly characterized by mild flu-like symptoms or can be complicated by respiratory deterioration, potentially leading to acute respiratory distress syndrome (ARDS) and/or other organ failure [3,4,5]. A severe course of COVID-19 with need of intensive care unit (ICU) admission can be observed in up to 20% of hospitalized patients [6, 7]. Patients admitted to ICU suffer from high mortality [7, 8]. Several large studies reported clinical features and revealed that older age and underlying comorbidities increase the risk of unfavorable outcome [5, 6, 9,10,47]. Further, SAPS II [OR 1.078; 95% CI 1.004–1.157] was independently associated with occurrence of SLD which confirms previous studies [47].
In general, liver injury and failure is a frequently observed in critically ill patients [23]. Traditionally, HLI and CLD were regarded as late features in critical illness [24]. However, recent findings showed that they are found early in life-threatening illness on the ICU [23,24,25]. In our cohort, SLD developed within one week after admission, with a median of 6 (4–11.3) days. The occurrence of HLI or CLD is associated with increased morbidity and mortality [21,22,23]. In the medical ICU about 20% develop CLD and 10% suffer from HLI [21, 22, 25]. In our cohort, we observed a higher rate of SLD, mainly as a consequence of the severity of COVID-19 with pronounced respiratory failure accompanied by sepsis and cardiac failure. Of interest, about 23% of patients with SLD had reduced ejection fraction measured by echocardiography. Further, Septic shock preceded SLD in 56% of patients. Presumably, the cause of SLD was septic shock combined with ARDS in more than 70% of our patients. However, data on patients with severe respiratory failure and/or ARDS are lacking. Mortality rates in patients with SLD were significantly higher in patients suffering from SLD. However, even after splitting injury patterns in HLI or CLD alone and a mixed injury pattern observed mortality rates were generally comparable between groups. Of interest, at time of death 12 of 15 patients met criteria of SLD. Highest mortality rate was observed in patients presenting with HLI injury pattern. Recent data showed that HLI accompanied by CLD increases complications and mortality [22]. After adjusting for covariables SLD was the most indicative factor [HR 3.347 95% CI 1.401–7.999] for mortality in our cohort of critically ill patients with COVID-19. A recent study showed that viral load can serve as predictor for mortality in patients with COVID-19 [48]. Interestingly, presence of viremia [OR 6.359 95% CI 1.336–30.253] was the most important factor associated with occurrence of SLD in our cohort, but was not associated with mortality. However, we observed significantly higher viral load as well as presence of viremia (defined as detection of viral RNA > 1000 copies/ml) in patients with SLD. This finding is novel and direct causation of liver injury by viral effects could be one explanation. Viremia was not associated with mortality in our cohort; this could be explained by the rather small number of patients included. Nevertheless, occurrence of viremia in critically ill patients (especially in patients with SLD) could serve as an early risk marker and should prompt close surveillance of liver function. Different clinical patterns and complications, like hypo-/hyperglycemia, hyperammonemia, respiratory failure or acute kidney injury in patients with SLD are associated with increased mortality [21,22,23,24, 46, 47]. Due to occurrence of SLD within a dynamic process in patients with multi-organ failure patients are generally not eligible for liver transplantation. However, even though no specific treatment of SLD is available, prevention of complications is of central importance. All in all, our data clearly demonstrate that occurrence of SLD is a multifactorial event. Severity of illness as well as complications during ICU, and direct viral effects play an important role in development of SLD.
Although, the number comorbidities in our cohort were high, no patient suffered from pre-existing liver disease. Pre-existing liver diseases were reported in up to 11% of patients with COVID-19 [1, 5, 8, 10] and were associated with fast deterioration of liver function and elevated mortality [20]. Thirty-two per-cent of patients presented with a BMI > 30 kg/m2. Although, we did not observe differences in occurrence of SLD in our cohort patients with non-alcoholic fatty liver disease or non-alcoholic steatohepatitis are probably at risk for SLD. However, whether COVID-19 aggravates occurrence of SLD or not must be addressed in larger analyses of critically ill patients with COVID-19 and pre-existing liver disease.
This study has strengths and limitations. First, the sample size of our study is rather small. However, this is the first and most comprehensive study describing the occurrence of SLD in critically ill patients with COVID-19. Second, for SLD we used a combination of well-established definitions of HLI and CLD. Both entities can be caused by different underlying mechanism, therefore our definition has to be interpreted with caution when comparing or data to other studies. Third, for detection of pre-existing liver disease, we carefully reviewed patient charts and due to routine clinical care patients were screened for presence of liver disease. However, due to the retrospective character of the study, we cannot entirely exclude the presence of pre-exiting liver disease. Fourth, we show results of a center experienced in management of ARDS and liver failure, and results and conclusions may not be generally transferable to other settings with less experience. Fifth, direct viral effects of SARS-CoV-2 could not be further validated in this clinical study and should be addressed in future studies. Sixth, residual confounding from unmeasured covariables is a matter of concern and cannot be entirely excluded. Future larger studies should be conducted to confirm these results.
Conclusion
In conclusion, our study could demonstrate that occurrence of SLD is a frequent observation in critically ill patients with COVID-19 and is associated with high mortality rates. Severity of illness as well as viremia seems to contribute to the occurrence of SLD and underline the multifactorial cause. Our findings highlight the significant contribution and impact on outcome of SLD in critically ill patients with COVID-19.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CCI:
-
Charlson Comorbidity Index
- CLD:
-
Cholestatic liver dysfunction
- COVID-19:
-
Coronavirus disease 2019
- ECMO:
-
Extracorporeal membrane oxygenation
- HFNC:
-
High-flow nasal cannula
- HLI:
-
Hypoxic liver injury
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- MAP:
-
Mean arterial pressure
- MV:
-
Mechanical ventilation
- NIV:
-
Non-invasive ventilation
- RRT:
-
Renal replacement therapy
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus-2
- SAPS II:
-
Simplified Acute Physiologic Assessment Score
- SOFA:
-
Sequential Organ Failure Assessment
References
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
WHO. WHO - World Map - COVID-19 [https://covid19.who.int/. Accessed online: January, 15th 2020] 2020 [Available from: https://covid19.who.int/. Accessed 15Jan 2021.
Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;15:458.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;57:894.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506.
Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42.
Karagiannidis C, Mostert C, Hentschker C, Voshaar T, Malzahn J, Schillinger G, et al. Case characteristics, resource use, and outcomes of 10,021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:42.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–9.
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan. China Intensive Care Med. 2020;46(5):846–8.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region. Italy JAMA. 2020;323(16):1574–81.
Wu C, Chen X, Cai Y, **a J, Zhou X, Xu S, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan. JAMA internal medicine: China; 2020.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020;7:96.
Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–30.
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–2.
Wang Y, Liu S, Liu H, Li W, Lin F, Jiang L, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020;73:807.
Zhang Y, Zheng L, Liu L, Zhao M, **ao J, Zhao Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city China. Liver Int. 2020;40(9):2095–103.
Cai Q, Huang D, Yu H, Zhu Z, **a Z, Su Y, et al. COVID-19: Abnormal liver function tests. J Hepatol. 2020;73(3):566–74.
Fan Z, Chen L, Li J, Cheng X, Yang J, Tian C, et al. Clinical Features of COVID-19-Related Liver Functional Abnormality. Clin Gastroenterol Hepatol. 2020;18(7):1561–6.
Iavarone M, D’Ambrosio R, Soria A, Triolo M, Pugliese N, Del Poggio P, et al. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J Hepatol. 2020. https://doi.org/10.1016/j.jhep.2020.06.001.
Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, et al. Impact of hypoxic hepatitis on mortality in the intensive care unit. Intensive Care Med. 2011;37(8):1302–10.
Jager B, Drolz A, Michl B, Schellongowski P, Bojic A, Nikfardjam M, et al. Jaundice increases the rate of complications and one-year mortality in patients with hypoxic hepatitis. Hepatology. 2012;56(6):2297–304.
Horvatits T, Drolz A, Trauner M, Fuhrmann V. Liver Injury and Failure in Critical Illness. Hepatology. 2019;70(6):2204–15.
Horvatits T, Trauner M, Fuhrmann V. Hypoxic liver injury and cholestasis in critically ill patients. Curr Opin Crit Care. 2013;19(2):128–32.
Kramer L, Jordan B, Druml W, Bauer P, Metnitz PG. Incidence and prognosis of early hepatic dysfunction in critically ill patients–a prospective multicenter study. Crit Care Med. 2007;35(4):1099–104.
Fuhrmann V, Jäger B, Zubkova A, Drolz A. Hypoxic hepatitis - epidemiology, pathophysiology and clinical management. Wien Klin Wochenschr. 2010;122(5–6):129–39.
Pfefferle S, Reucher S, Norz D, Lutgehetmann M. Evaluation of a quantitative RT-PCR assay for the detection of the emerging coronavirus SARS-CoV-2 using a high throughput system. Euro Surv. 2020;25:9.
Nörz D, Frontzek A, Eigner U, Oestereich L, Fischer N, Aepfelbacher M, et al. Pushing beyond specifications: Evaluation of linearity and clinical performance of a fully automated SARS-CoV-2 RT-PCR assay for reliable quantification in blood and other materials outside recommendations. J Clin Virol. 2020;132:104650.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854–87.
Kluge S, Janssens U, Welte T, Weber-Carstens S, Marx G, Karagiannidis C. German recommendations for critically ill patients with COVID-19. Medizinische Klinik, Intensivmedizin und Notfallmedizin. 2020;54:1–4.
Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and Liver. J Hepatol. 2020;73(5):1231–40.
Xu L, Liu J, Lu M, Yang D, Zheng X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020;40(5):998–1004.
Arabi YM, Al-Omari A, Mandourah Y, Al-Hameed F, Sindi AA, Alraddadi B, et al. Critically Ill Patients With the Middle East Respiratory Syndrome: A Multicenter Retrospective Cohort Study. Crit Care Med. 2017;45(10):1683–95.
Cao W. Clinical features and laboratory inspection of novel coronavirus pneumonia (COVID-19) in **angyang, Hubei. MedRxiv. 2020;85:6.
Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091.
Henrion J, Minette P, Colin L, Schapira M, Delannoy A, Heller FR. Hypoxic hepatitis caused by acute exacerbation of chronic respiratory failure: a case-controlled, hemodynamic study of 17 consecutive cases. Hepatology. 1999;29(2):427–33.
Saner FH, Olde Damink SW, Pavlakovic G, van den Broek MA, Sotiropoulos GC, Radtke A, et al. Positive end-expiratory pressure induces liver congestion in living donor liver transplant patients: myth or fact. Transplantation. 2008;85(12):1863–6.
Krenn CG, Krafft P, Schaefer B, Pokorny H, Schneider B, Pinsky MR, et al. Effects of positive end-expiratory pressure on hemodynamics and indocyanine green kinetics in patients after orthotopic liver transplantation. Crit Care Med. 2000;28(6):1760–5.
Roedl K, Spiel AO, Nurnberger A, Horvatits T, Drolz A, Hubner P, et al. Hypoxic liver injury after in- and out-of-hospital cardiac arrest: Risk factors and neurological outcome. Resuscitation. 2019;137:175–82.
Jung C, Fuernau G, Eitel I, Desch S, Schuler G, Kelm M, et al. Incidence, laboratory detection and prognostic relevance of hypoxic hepatitis in cardiogenic shock. Clin Res Cardiol. 2017;106(5):341–9.
Drolz A, Horvatits T, Roedl K, Rutter K, Staufer K, Haider DG, et al. Outcome and features of acute kidney injury complicating hypoxic hepatitis at the medical intensive care unit. Ann Intensive Care. 2016;6(1):61.
Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, et al. Hypoxic hepatitis: underlying conditions and risk factors for mortality in critically ill patients. Intensive Care Med. 2009;35(8):1397–405.
Pujadas E, Chaudhry F, McBride R, Richter F, Zhao S, Wajnberg A, et al. SARS-CoV-2 viral load predicts COVID-19 mortality. The Lancet Respiratory Medicine. 2020;1:1. https://doi.org/10.1016/s2213-2600(20)30354-4.
Acknowledgements
We sincerely thank the study nurses of the Department of Intensive Care Medicine involved in data acquisition and management—Grit Ringeis, Melanie Kerinn, Lisa Krebs, and Andrea Conrad
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported exclusively by institutional funds of the Department of Intensive Care Medicine.
Author information
Authors and Affiliations
Contributions
KR, VF and SK conceived and designed the study. KR and DJ, DW, AD, OB, MK, GdH, CB, DF, BS and ML were involved in data acquisition and laboratory analysis. KR, DJ, DW, AD, AN and VF analyzed and interpreted the data. KR and VF drafted the manuscript. DW, ML, AN, VF and SK critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of the Hamburg Chamber of Physicians was informed about the study (No.: WF-142/20). The study was approved by the local clinical institutional review board and complied with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing Interests
KR, DJ, AD, OB, GDH BS, CB and VF do not report any conflicts of interest. SK received research support by Ambu, E.T.View Ltd, Fisher & Paykel, Pfizer and Xenios, lecture honoraria from ArjoHuntleigh, Astellas, Astra, Basilea, Bard, Baxter, Biotest, CSL Behring, CytoSorbents, Fresenius, Gilead, MSD, Orion, Pfizer, Philips, Sedana, Sorin, Xenios and Zoll, and consultant honorarium from AMOMED, Astellas, Baxter, Bayer, Fresenius, Gilead, MSD, Pfizer and Xenios. AN received research funds, lecture honoraria and travel reimbursement within the last 5 years from CytoSorbents Europe, Biotest AG and ThermoFisher Scientific. DF reports lecture honoraria within the last 5 years from Xenios AG. DW received lecture and consultant honorarium from Gilead, MSD, Pfizer, Shionogi and reports no other potential conflict of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Biomarkers stratified according no liver dysfunction and severe liver dysfunction. Table S2. Viral characteristics in patients with and without severe liver dysfunction. Table S3a. Cox regression model for factors associated with ICU mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roedl, K., Jarczak, D., Drolz, A. et al. Severe liver dysfunction complicating course of COVID-19 in the critically ill: multifactorial cause or direct viral effect?. Ann. Intensive Care 11, 44 (2021). https://doi.org/10.1186/s13613-021-00835-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-021-00835-3