Abstract
Objective
To investigate the diagnostic performance of MRI in detecting clinically significant prostate cancer (csPCa) and prostate cancer (PCa) in patients with prostate-specific antigen (PSA) levels of 4–10 ng/mL.
Methods
A computerized search of PubMed, Embase, Cochrane Library, Medline, and Web of Science was conducted from inception until October 31, 2023. We included articles on the use of MRI to detect csPCa or PCa at 4–10 ng/mL PSA. The primary and secondary outcomes were MRI performance in csPCa and PCa detection, respectively; the estimates of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were pooled in a bivariate random-effects model.
Results
Among the 19 studies (3879 patients), there were 10 (2205 patients) and 13 studies (2965 patients) that reported MRI for detecting csPCa or PCa, respectively. The pooled sensitivity and specificity for csPCa detection were 0.84 (95% confidence interval [CI], 0.79–0.88) and 0.76 (95%CI, 0.65–0.84), respectively, for PCa detection were 0.82 (95%CI, 0.75–0.87) and 0.74 (95%CI, 0.65–0.82), respectively. The pooled NPV for csPCa detection was 0.91 (0.87–0.93). Biparametric magnetic resonance imaging also showed a significantly higher sensitivity and specificity relative to multiparametric magnetic resonance imaging (both p < 0.01).
Conclusion
Prostate MRI enables the detection of csPCa and PCa with satisfactory performance in the PSA gray zone. The excellent NPV for csPCa detection indicates the possibility of biopsy decision-making in patients in the PSA gray zone, but substantial heterogeneity among the included studies should be taken into account.
Clinical relevance statement
Prostate MRI can be considered a reliable and satisfactory tool for detecting csPCa and PCa in patients with PSA in the “gray zone”, allowing for reducing unnecessary biopsy and optimizing the overall examination process.
Key Points
-
Prostate-specific antigen (PSA) is a common screening tool for prostate cancer but risks overdiagnosis.
-
MRI demonstrated excellent negative predictive value for prostate cancer in the PSA gray zone.
-
MRI can influence decision-making for these patients, and biparametric MRI should be further evaluated.
Graphical Abstract

Similar content being viewed by others
Introduction
Prostate cancer (PCa) is one of the most frequently diagnosed cancers in men worldwide, and its prevalence continues to increase annually [1]. Thus, it is imperative to improve the accuracy of diagnosis for PCa, particularly for clinically significant PCa (csPCa) that requires curative treatment and active monitoring, so as to reduce the mortality due to malignancy [2]. As a serum marker, prostate-specific antigen (PSA) is a common clinical screening index. However, numerous trials have confirmed that this approach has the risk of over-diagnosis [3], since PSA is organ-specific but not cancer-specific. Clinically, patients with PSA levels > 10 ng/mL are highly suspected of having PCa, such that they necessitate a biopsy. In contrast, it is still debatable as to whether biopsies should be carried out in patients with PSA values in the range of 4–10 ng/mL [4], referred to as the “gray zone.” Notably, conducting biopsies in men with PSA in the “gray zone” may lead to over-diagnosis and over-treatment, as well as other negative effects, such as bleeding, genitourinary infections, and urinary retention [5].
With its morphological and various functional imaging modalities, multiparametric magnetic resonance imaging (mpMRI) of the prostate has been applied for the detection, localization, and staging of PCa, and for patient treatment planning [6]. Numerous studies have shown that using MRI prior to biopsy can diminish the detection of indolent prostate cancer while improving the accuracy of diagnosis for csPCa, thus leading to a reduction in unnecessary prostate biopsies [7, 8].
A meta-analysis published by Sathianathen et al indicated that the pooled negative predictive values (NPVs) of MRI for csPCa diagnosis with different combinations of negative mpMRI and csPCa definitions were satisfactory, ranging from 86.8 to 97.1%, suggesting that there was a reliable value for negative MRI in excluding non-csPCa patients [9]. However, this study did not analyze the efficacy of MRI in the context of the PSA gray zone, which is a challenging issue encountered in clinical practice. The diagnostic performance of prostate MRI has been widely studied recently in individuals with PSA levels of 4–10 ng/mL, albeit with high variability found among various centers.
Therefore, we conducted a comprehensive analysis of existing literature and performed a meta-analysis to investigate the performance of prostate MRI in patients with PSA levels of 4–10 ng/mL and explored the potential benefits of MRI in the management of patients in the PSA gray zone.
Materials and methods
This meta-analysis and systematic review (CRD: 42023473553) were reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [10].
Search strategy and selection criteria
Two authors systematically searched PubMed, Embase, Cochrane Library, Medline, and Web of Science for studies published from inception to October 31, 2023, with language restricted to English. The search strategy is detailed in Supplemental Materials (S-1). The titles and abstracts of all studies obtained through the search strategies were independently screened by two reviewers. The reviewers then read the full text of the articles to determine whether they appropriately satisfied the inclusion criteria.
Inclusion and exclusion criteria
Studies were considered eligible if they met the following criteria, applying the participants, intervention, control, outcomes, and study (PICOS) format.
-
1.
P: men with elevated PSA levels in the range of 4–10 ng/mL.
-
2.
I: patients who underwent MRI for assessing csPCa or PCa.
-
3.
C: pathological results from radical prostatectomy or biopsy taken as the reference standard.
-
4.
O: outcome indicators reflecting the true positive (TP), false positive (FP), false negative (FN), and true negative (TN), or the sensitivity and specificity of MRI diagnostic performance.
-
5.
S: original articles.
The exclusion criteria included the following:
-
1.
Articles that were unrelated to the field of interest of this study.
-
2.
A PSA level not in the range of 4–10 ng/mL.
-
3.
Data insufficient to construct a 2 × 2 table.
-
4.
Non-original articles such as editorials, case reports, narrative reviews, meta-analyses, or conference abstracts.
-
5.
Languages other than English or unavailable full text.
Data extraction and quality assessment
The following three types of information were extracted from the included articles: (1) demographic and clinical characteristics—i.e., number of patients, number of malignancies, age, and PSA level; (2) study characteristics such as publication year, study period, country, study design, blinding, Prostate Imaging Reporting and Data System (PI-RADS) version with its cutoff value, reference standard, and analysis (patient or zone); and (3) technical characteristics of MRI, such as magnet strength, vendor, MRI sequences, number of readers, readers’ experience, and coil. The quality of the diagnostic accuracy studies was assessed by implementing the Quality Assessment of Diagnostic Accuracy Studies-2 tool (QUADAS-2) [11].
The process described above was completed by two independent reviewers (L.L.X. and E.J.G., with 6 and 2 years of experience, respectively), and disagreements were resolved through discussion or by consulting a senior reviewer (S.H.).
Data synthesis and analysis
The heterogeneity of the results of the included studies was quantified using I2 statistic [12]. Cochran’s Q test with p < 0.1 indicated significant heterogeneity. The summary estimates of sensitivity and specificity, the combined positive predictive value (PPV) and negative predictive value (NPV), and their corresponding 95% confidence intervals (CIs) were computed using the bivariate random-effects model [13]. A hierarchical summary receiver operating characteristics (HSROC) [14] curve with a 95% confidence region and prediction region was presented graphically to illustrate our results and to show the amount of variation between the studies. The presence of publication bias was tested by applying the Deeks’ funnel plot, and statistical significance was determined by the Deeks’ asymmetry test [15].
The following categories were used in the subgroup analysis to investigate the sources of heterogeneity in the detection of csPCa.
-
1.
PI-RADS version (PI-RADS v2.1 vs. PI-RADS v2).
-
2.
Sequence (mpMRI vs. biparametric magnetic resonance imaging [bpMRI]).
-
3.
Standard reference (TRUS-guided systematic biopsy [TRUS-SB] combined with cognitive MRI fusion-guided targeted biopsy [CMF-TB] vs. TRUS-SB).
-
4.
Study design (prospective vs. retrospective).
The performance of MRI in detecting PCa was the secondary objective, with the sensitivities and specificities pooled. We then performed subgroup analysis and meta-regression based on whether or not the PI-RADS assessment was applied.
Statistical analysis was performed using Stata 14.0 (StataCorp LLC, College Station, TX, USA) with p < 0.05 considered the statistically significant difference. RevMan 5.3 (Cochrane Library) was implemented for processing the assessment of quality.
Results
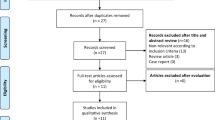
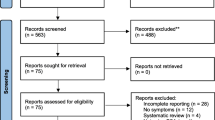
Literature search
The detailed study selection process is presented in Fig. 1. A total of 19 studies with 3879 participants that met the inclusion criteria were chosen for the final analysis [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,22, 28, 22,23, 28, 29, 31, 32, 34], six studies used 1.5-T scanners [20, 24,25,26,27, 30], one study used both [16]; one article did not provide relevant explanations [33]. The relevant elements are described in detail in the Supplemental Materials (S-4).
Quality assessment
In general, the quality of the studies was moderate, with 15 studies satisfying four out of seven items in the QUADAS-2 tool. The detailed quality assessment of the enrolled studies is depicted in Fig. S1, a detailed description is presented in the Supplemental Materials (S-5), and the specific evaluation results of each study are presented in Table S2.
Diagnostic performance of MRI for detection of csPCa
The pooled sensitivity of MRI for csPCa detection was 0.84 (95%CI, 0.79–0.88) and the pooled specificity was 0.76 (95%CI, 0.65–0.84) (Fig. 2a, b). The summary PPV and NPV were 0.62 (95%CI, 0.51–0.71) and 0.91 (95%CI, 0.87–0.93), respectively (Fig. 2c, d). The area under the HSROC curve was 0.88 (95%CI, 0.85–0.90) (Fig. 3). The Deeks’ funnel plot showed no evidence of publication bias, with a p value of 0.95 for the asymmetry test (Fig. 4). Heterogeneity was observed as indicated by the Cochran’s Q test (p < 0.01), with the I2 statistic denoting substantial heterogeneity in relation to the sensitivity (I2 = 90%) and specificity (I2 = 71%). The HSROC curve revealed significant differences between the 95% confidence and prediction zones, further highlighting the variability within the studies.
Subgroup analysis and meta-regression
The results of the subgroup analysis and meta-regression are presented in Table 4. The pooled sensitivities and specificities were significantly different between bpMRI and mpMRI (0.87 vs. 0.83, p < 0.01; 0.87 vs. 0.69, p < 0.01). The pooled sensitivity for PI-RADS v2.1 was significantly higher than that for PI-RADS v2.0 (0.88 vs. 0.81, p = 0.02). As for the standard reference, TRUS-SB in combination with CMF-TB revealed significantly high sensitivity compared with TRUS-SB alone (0.88 vs. 0.77, p = 0.02). The pooled sensitivity of prospective studies was lower than that of retrospective studies (0.83 vs. 0.85, p = 0.01).
Diagnostic performance of MRI for detection of PCa
The pooled sensitivity and specificity of the 13 studies [18, 19, 23,24,25,26,27,28,29,30, 32,33,34] for PCa detection were 0.82 (95%CI, 0.75–0.87) and 0.74 (95%CI, 0.65–0.82), respectively, with the area under the HSROC curve of 0.85 (95%CI, 0.82–0.88) (Figs. S2 and S3). Detailed information on secondary outcomes is depicted in the Supplemental Materials (S-6). We further conducted subgroup analysis on the diagnostic performance of MRI in the diagnosis of prostate cancer according to whether PI-RADS was used. The results are provided in Table S1.
Discussion
In this meta-analysis, we investigated the diagnostic efficacy of MRI in the detection of both csPCa and PCa among patients with PSA levels between 4 and 10 ng/mL. Generally, MRI demonstrated a favorable diagnostic performance for csPCa detection, with the area under the HSROC curve, sensitivity, and specificity of 0.88 (0.85–0.90), 0.84 (0.79–0.88), and 0.76 (0.65–0.84), respectively. The pooled NPV of prostate MRI for csPCa detection was satisfactory with the value of 0.91 (0.87–0.93). Regarding PCa detection, the pooled sensitivity and specificity were 0.82 (0.75–0.87) and 0.74 (0.65–0.82), respectively.
The pooled NPV for csPCa detection obtained in our study was excellent, indicating that there is sufficient certainty to exclude non-csPCa patients when the MRI result is negative [9], which would lead to a reduction in unnecessary biopsies. A previous study shown that in patients with a PSA < 10 ng/mL, the median NPV of MRI for overall PCa was 86.3% (IQR, 73.3%–93.6%), with a median cancer prevalence of 35.4% (IQR, 27.6–42.5%) [35]; this was similar to our research results. Similarly, the results of the study published by Xu et al showed that at a median PSA value of 4.65 (0.22–86.00) ng/mL and a csPCa prevalence of 42%, the NPV of mpMRI for csPCa detection was 87.8%, whereas the NPV of bpMRI for csPCa detection was 85.0% [36]. Although the NPV varied in the studies included in our analysis (ranging from 76–95%—potentially the result of the heterogeneous prevalence among them, which ranged between 18 and 67%), this indicator was generally satisfactory and supported the benefits of MRI in reducing unnecessary biopsies.
Compared with the excellent pooled NPV in our study, the pooled PPV of 0.66 (0.54–0.76) was less than ideal. Because prostate MRI is a screening tool and clinical priority is defined as not missing any significant cancer, we paid more attention to the NPV of MRI screening. However, the PPV also reflects vital clinical significance as it describes whether positive mpMRI consistently supports the presence of csPCa. Regarding the relatively low PPV for patients with a positive prostate MRI, additional clinical information may need to be considered before proceeding to a biopsy. A review by Schoots et al argued that multivariable risk prediction tools—including clinical, biochemical parameters and MRI suspicion scores—possess the potential to significantly reduce the number of biopsies and the detection of clinically insignificant prostate cancer; these tools will then assist doctors and patients in making appropriate biopsy decisions [37]. Among these modalities, PSA density (PSAD) is an important parameter in guiding biopsy decisions. In a systematic review by Wang et al, a quantitative risk assessment was performed that combined different PSAD cut-offs and MRI results to predict the occurrence of csPCa [38]. PSAD demonstrated complementary performance and predictive value, especially among patients with negative MRI and PI-RADS 3 or Likert 3 lesions. However, the diagnostic performance of bp-MRI combined with PSAD did not demonstrate statistically significant improvement in all evaluation schemes, according to the research by Cuocolo et al [39]. In light of these findings, the role of PSAD remains to be further investigated. We envision that incorporating prostate MRI, clinical factors, and possible biomarkers into the biopsy decision-making process will enhance the diagnostic accuracy and increase the confidence to avoid unnecessary biopsies in patients with PSA gray zone.
Considerable heterogeneity was observed among the included studies regarding the PI-RADS versions, standard reference, and study design. Compared with three studies that entailed bpMRI, eight studies with mpMRI produced relatively low pooled sensitivity and specificity. In consensus with our results, in the study by Han et al [21], the area under the curve value for bpMRI in csPCa detection (0.86) was significantly higher than that for mpMRI (0.82). In addition, several published meta-analyses in which the diagnostic effectiveness of bpMRI and mpMRI were compared, suggested that bpMRI exhibited performance comparable to that of mpMRI when diagnosing csPCa in men with any PSA level [36, 40]. As a standard acquisition protocol of mpMRI, DCE images are of limited value in prostate cancer detection according to the PI-RADS recommendations. A study reported by Messina et al [41] suggested that upgrading peripheral lesions with DWI Score 3 to PI-RADS 4 due to a positive DCE negatively impacted the accuracy of MRI and decrease the true csPCa detection rate of PI-RADS 4 lesions. Nevertheless, DCE remains valuable in cases when DWI and/or T2WI do not reach an adequate level of quality. The ESUR/ESUI expert panel has emphasized the importance of regularly monitoring and reporting MRI quality in clinical practice [42]. The PI-QUAL scoring system is a useful tool for standardized quality assessment and reporting, with a potential impact on patient care [43]. Ponsiglione et al found that the detection efficiency of extracapsular extension was significantly improved in high-quality mpMRI scans, with diagnostic accuracy improving from 0.564 in low-quality scans to 0.849 in high-quality scans (PI-QUAL ≥ 4) [44]. A study by Brembilla et al showed that in scans of suboptimal quality, the proportion of biopsies for PI-RADS 3 MRI rose by 18% while the detection rate of csPCa declined by 35%, confirming the potential impact of MRI scan quality on the performance of mpMRI relative to biopsy results [45].
The inherent disadvantages of setting bpMRI as a default approach should also be noted, including low reproducibility in community hospitals, lack of widely accepted imaging quality standards, and the impossibility of performing loco-regional staging [46]. However, early detection of csPCa by MRI is a priority. Given the analysis above, we postulate that bpMRI could serve as a potential substitute for mpMRI to optimize the clinical workup in men with PSA levels of 4–10 ng/mL, allowing us to avoid the extra expense and scan time as well as the side effects of contrast media. Moreover, there is an urgent need for the standardization of prostate bpMRI acquisition and reporting, and more robust validations of this imaging methodology should be carried out [47].
An additional significant factor that affected heterogeneity in the sensitivity was standard reference. Eight studies using TRUS-SB combined with CMF-TB as a standard reference produced significantly higher sensitivity than the other three studies that did not incorporate CMF-TB. A comparative study conducted by Elkhoury et al [48] revealed that the clinically significant prostate cancer detection rate (CDR) by systematic biopsy was 15.7%, while the CDR using cognitive fusion biopsy was 33.3% on a per-core basis. The reason behind our outcome may have been the greater CDR of CMF-TB. CMF-TB involves an operator who is cognitively aware of the obtained MRI interpretation and uses anatomic landmarks to target suspicious lesions on real-time transrectal ultrasound (TRUS) [49]. There has thus been an improvement in the diagnostic performance of prostate MRI commensurate with the increasing rate of cancer detection.
Li et al in a relevant review systematically evaluated the effectiveness of MRI and magnetic resonance spectroscopy (MRS) in detecting PCa and csPCa in patients with PSA levels in the gray zone before biopsy, as well as their applications in guiding prostate biopsy [50]. As one of the sequences of mpMRI, MRS imaging (MRSI) enables noninvasive assessment of certain metabolites in the prostate gland; however, it is not recommended in the latest version of PI-RADS. Thus, we did not include articles about MRS. In addition, our study is an adjunct to clinical practice, not only summarizing the diagnostic efficacies of prostate MRI for csPCa in patients in the PSA gray zone, but also further assessing the impact of prostate MRI on the decision-making of patients with PSA gray zone.
Our study has several limitations. First, the design of the majority of studies regarding csPCa detection was retrospective, which may have generated some bias in the patient selection domain. Second, there was significant heterogeneity among the studies, thus affecting the general applicability of our summary estimates. We conducted subgroup analyses and meta-regression to explore the potential factors underlying the heterogeneity, but a portion of heterogeneity remained unexplained. Finally, even though our study showed that MRI screening for csPCa detection in men with PSA levels of 4–10 ng/mL exhibited satisfactory diagnostic performance with good NPV and moderate PPV, the prevalence is an influencing factor that should be taken into consideration when conducting clinical decision strategies.
Conclusion
In this study, it was found that MRI could be considered a reliable and satisfactory tool to instruct clinical decisions for patients with PSA in the “gray zone,” particularly for csPCa detection. Furthermore, the high NPV of prostate MRI for csPCa detection indicates that negative MRI can reliably rule out the non-csPCa, sparing patients unnecessary biopsy.
Data availability
Information on study subjects was based on the previously published articles which were included in this study.
Abbreviations
- bpMRI:
-
Biparametric magnetic resonance imaging
- CI:
-
Confidence interval
- CMF-TB:
-
Cognitive MRI fusion-guided targeted biopsy
- csPCa:
-
Clinically significant prostate cancer
- HSROC:
-
Hierarchical summary receiver operating characteristics
- mpMRI:
-
Multiparametric magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- NPV:
-
Negative predictive value
- PCa:
-
Prostate cancer
- PI-RADS:
-
Prostate Imaging Reporting and Data System
- PPV:
-
Positive predictive value
- PSA:
-
Prostate-specific antigen
- PSAD:
-
Prostate-specific antigen density
- QUADAS–2:
-
Quality Assessment of Diagnostic Accuracy Studies–2
- TRUS-SB:
-
Transrectal ultrasound-guided systematic biopsy
References
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clin 73:17–48
Prostate Cancer Guideline, European Association of Urology (2023). https://uroweb.org/guideline/prostate-cancer/. Accessed 25 Nov 2023
Ilic D, Djulbegovic M, Jung JH et al (2018) Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ 362:k3519
Stamey TA, Johnstone IM, McNeal JE, Lu AY, Yemoto CM (2002) Preoperative serum prostate specific antigen levels between 2 and 22 ng./ml. correlate poorly with post-radical prostatectomy cancer morphology: prostate specific antigen cure rates appear constant between 2 and 9 ng./ml. J Urol 167:103–111
Gershman B, Van Houten HK, Herrin J et al (2017) Impact of prostate-specific antigen (PSA) screening trials and revised PSA screening guidelines on rates of prostate biopsy and postbiopsy complications. Eur Urol 71:55–65
Stabile A, Giganti F, Rosenkrantz AB et al (2020) Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nat Rev Urol 17:41–61
Radtke JP, Wiesenfarth M, Kesch C et al (2017) Combined clinical parameters and multiparametric magnetic resonance imaging for advanced risk modeling of prostate cancer-patient-tailored risk stratification can reduce unnecessary biopsies. Eur Urol 72:888–896
Chiu PK, Lam TY, Ng CF et al (2023) The combined role of MRI prostate and prostate health index in improving detection of significant prostate cancer in a screening population of Chinese men. Asian J Androl 25:674–679
Sathianathen NJ, Omer A, Harriss E et al (2020) Negative predictive value of multiparametric magnetic resonance imaging in the detection of clinically significant prostate cancer in the prostate imaging reporting and data system era: a systematic review and meta-analysis. Eur Urol 78:402–414
McInnes MDF, Moher D, Thombs BD et al (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Rutter CM, Gatsonis CA (2001) A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 20:2865–2884
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Sun Z, Wu P, Cui Y et al (2023) Deep-learning models for detection and localization of visible clinically significant prostate cancer on multi-parametric MRI. J Magn Reson Imaging 58:1067–1081
Wei CG, Chen T, Zhang YY et al (2020) Biparametric prostate MRI and clinical indicators predict clinically significant prostate cancer in men with “gray zone” PSA levels. Eur J Radiol 127:108977
Xu N, Wu YP, Chen DN et al (2018) Can prostate imaging reporting and data system version 2 reduce unnecessary prostate biopsies in men with PSA levels of 4-10 ng/ml? J Cancer Res Clin Oncol 144:987–995
Liu C, Liu SL, Wang ZX et al (2018) Using the prostate imaging reporting and data system version 2 (PI-RIDS v2) to detect prostate cancer can prevent unnecessary biopsies and invasive treatment. Asian J Androl 20:459–464
Baruah SK, Das N, Baruah SJ et al (2019) Combining prostate-specific antigen parameters with prostate imaging reporting and data system score version 2.0 to improve its diagnostic accuracy. World J Oncol 10:218–225
Han C, Liu S, Qin XB, Ma S, Zhu LN, Wang XY (2020) MRI combined with PSA density in detecting clinically significant prostate cancer in patients with PSA serum levels of 4∼10ng/mL: Biparametric versus multiparametric MRI. Diagn Interv Imaging 101:235–244
Niu XK, Li J, Das SK, ** a nomogram based on multiparametric magnetic resonance imaging for forecasting high-grade prostate cancer to reduce unnecessary biopsies within the prostate-specific antigen gray zone. BMC Med Imaging 17:11
Qi Y, Zhang S, Wei J et al (2020) Multiparametric MRI-based radiomics for prostate cancer screening with PSA in 4-10 ng/mL to reduce unnecessary biopsies. J Magn Reson Imaging 51:1890–1899
Tamada T, Sone T, Higashi H et al (2011) Prostate cancer detection in patients with total serum prostate-specific antigen levels of 4-10 ng/mL: diagnostic efficacy of diffusion-weighted imaging, dynamic contrast-enhanced MRI, and T2-weighted imaging. AJR Am J Roentgenol 197:664–670
Dwivedi DK, Kumar R, Dwivedi AK et al (2018) Prebiopsy multiparametric MRI-based risk score for predicting prostate cancer in biopsy-naive men with prostate-specific antigen between 4-10 ng/mL. J Magn Reson Imaging 47:1227–1236
Vilanova JC, Comet J, Capdevila A et al (2001) The value of endorectal MR imaging to predict positive biopsies in clinically intermediate-risk prostate cancer patients. Eur Radiol 11:229–235
Kubota Y, Kamei S, Nakano M, Ehara H, Deguchi T, Tanaka O (2008) The potential role of prebiopsy magnetic resonance imaging combined with prostate-specific antigen density in the detection of prostate cancer. Int J Urol 15:322–326. discussion 327
Chen Y, Ruan M, Zhou B et al (2021) Cutoff values of prostate imaging reporting and data system version 2.1 score in men with prostate-specific antigen level 4 to 10 ng/mL: importance of lesion location. Clin Genitourin Cancer 19:288–295
Pepe P, Garufi A, Priolo G, Pennisi M (2015) Can 3-Tesla pelvic phased-array multiparametric MRI avoid unnecessary repeat prostate biopsy in patients with PSA < 10 ng/mL? Clin Genitourin Cancer 13:e27–e30
Sciarra A, Panebianco V, Ciccariello M et al (2010) Value of magnetic resonance spectroscopy imaging and dynamic contrast-enhanced imaging for detecting prostate cancer foci in men with prior negative biopsy. Clin Cancer Res 16:1875–1883
Yang J, Li J, **ao L et al (2023) (68)Ga-PSMA PET/CT-based multivariate model for highly accurate and noninvasive diagnosis of clinically significant prostate cancer in the PSA gray zone. Cancer Imaging 23:81
Zhang CC, Tu X, Lin TH et al (2023) Combining clinical parameters and multiparametric magnetic resonance imaging to stratify biopsy-naïve men for an optimum diagnostic strategy with prostate-specific antigen 4 ng ml−1 to 10 ng ml−1. Asian J Androl 25:492–498
Liu T, Zhang X, Chen R, Deng X, Fu B (2023) Development, comparison, and validation of four intelligent, practical machine learning models for patients with prostate-specific antigen in the gray zone. Front Oncol 13:1157384–1157384
Zhong JG, Shi L, Liu J, Cao F, Ma YQ, Zhang Y (2023) Predicting prostate cancer in men with PSA levels of 4-10 ng/mL: MRI-based radiomics can help junior radiologists improve the diagnostic performance. Sci Rep 13:4846
Moldovan PC, Van den Broeck T, Sylvester R et al (2017) What is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate cancer at biopsy? a systematic review and meta-analysis from the European Association of Urology prostate cancer guidelines panel. Eur Urol 72:250–266
Xu L, Zhang G, Shi B et al (2019) Comparison of biparametric and multiparametric MRI in the diagnosis of prostate cancer. Cancer Imaging 19:90
Schoots IG, Padhani AR (2020) Personalizing prostate cancer diagnosis with multivariate risk prediction tools: how should prostate MRI be incorporated? World J Urol 38:531–545
Wang S, Kozarek J, Russell R et al (2023) Diagnostic performance of prostate-specific antigen density for detecting clinically significant prostate cancer in the era of magnetic resonance imaging: a systematic review and meta-analysis. Eur Urol Oncol 7:189–203
Cuocolo R, Stanzione A, Rusconi G et al (2018) PSA-density does not improve bi-parametric prostate MR detection of prostate cancer in a biopsy naïve patient population. Eur J Radiol 104:64–70
Tamada T, Kido A, Yamamoto A et al (2021) Comparison of biparametric and multiparametric MRI for clinically significant prostate cancer detection with PI-RADS version 2.1. J Magn Reson Imaging 53:283–291
Messina E, Pecoraro M, Laschena L et al (2023) Low cancer yield in PI-RADS 3 upgraded to 4 by dynamic contrast-enhanced MRI: is it time to reconsider scoring categorization? Eur Radiol 33:5828–5839
Turkbey B, Rosenkrantz AB, Haider MA et al (2019) Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur Urol 76:340–351
Giganti F, Kirkham A, Kasivisvanathan V et al (2021) Understanding PI-QUAL for prostate MRI quality: a practical primer for radiologists. Insights Imaging 12:59
Ponsiglione A, Stanzione A, Califano G et al (2023) MR image quality in local staging of prostate cancer: Role of PI-QUAL in the detection of extraprostatic extension. Eur J Radiol 166:110973
Brembilla G, Lavalle S, Parry T et al (2023) Impact of prostate imaging quality (PI-QUAL) score on the detection of clinically significant prostate cancer at biopsy. Eur J Radiol 164:110849
Pecoraro M, Messina E, Bicchetti M et al (2021) The future direction of imaging in prostate cancer: MRI with or without contrast injection. Andrology 9:1429–1443
Cuocolo R, Verde F, Ponsiglione A et al (2021) Clinically significant prostate cancer detection with biparametric MRI: a systematic review and meta-analysis. AJR Am J Roentgenol 216:608–621
Elkhoury FF, Felker ER, Kwan L et al (2019) Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: the prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study. JAMA Surg 154:811–818
Sugano D, Kaneko M, Yip W, Lebastchi AH, Cacciamani GE, Abreu AL (2021) Comparative effectiveness of techniques in targeted prostate biopsy. Cancers (Basel) 13:1449
Li X, Li C, Chen M (2023) Patients with “gray zone” PSA levels: application of prostate MRI and MRS in the diagnosis of prostate Cancer. J Magn Reson Imaging 57:992–1010
Funding
This study has received funding from the Bei**g Natural Science Foundation (Grant No. L232133), National High Level Hospital Clinical Research Funding (Grant No. 2022-PUMCH-A-033 and 2022-PUMCH-B-069), and the CAMS Innovation Fund for Medical Sciences (CIFMS) (Grant No. 2022-I2M-C&T-B-019).
Author information
Authors and Affiliations
Contributions
Conceptualization: E.G., H.S., Z.J.; data curation: L.X., E.G., G.Z., D.Z., J.Z., X.Z., X.B., L.C., Q.P.; funding acquisition: H.S., G.Z., Z.J.; methodology: L.X., H.S.; resources: H.S., Z.J.; supervision: H.S., Z.J.; visualization: E.G., L.X.; writing-original draft: all authors; writing-review & editing: all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, E., Xu, L., Zhang, D. et al. Diagnostic performance of MRI in detecting prostate cancer in patients with prostate-specific antigen levels of 4–10 ng/mL: a systematic review and meta-analysis. Insights Imaging 15, 147 (2024). https://doi.org/10.1186/s13244-024-01699-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-024-01699-4