Abstract
Background
The high rate of stoma placement during emergency laparotomy for secondary peritonitis is a paradigm in need of change in the current fast-track surgical setting. Despite growing evidence for the feasibility of primary bowel reconstruction in a peritonitic environment, little data substantiate a surgeons’ choice between a stoma and an anastomosis. The aim of this retrospective analysis is to identify pre- and intraoperative parameters that predict the leakage risk for enteric sutures placed during source control surgery (SCS) for secondary peritonitis.
Methods
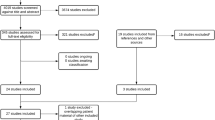
Between January 2014 and December 2020, 497 patients underwent SCS for secondary peritonitis, of whom 187 received a primary reconstruction of the lower gastro-intestinal tract without a diverting stoma. In 47 (25.1%) patients postoperative leakage of the enteric sutures was directly confirmed during revision surgery or by computed tomography. Quantifiable predictors of intestinal suture outcome were detected by multivariate analysis.
Results
Length of intensive care, in-hospital mortality and failure of release to the initial home environment were significantly higher in patients with enteric suture leakage following SCS compared to patients with intact anastomoses (p < 0.0001, p = 0.0026 and p =0.0009, respectively). Reduced serum choline esterase (sCHE) levels and a high extent of peritonitis were identified as independent risk factors for insufficiency of enteric sutures placed during emergency laparotomy.
Conclusions
A preoperative sCHE < 4.5 kU/L and generalized fecal peritonitis associate with a significantly higher incidence of enteric suture insufficiency after primary reconstruction of the lower gastro-intestinal tract in a peritonitic abdomen. These parameters may guide surgeons when choosing the optimal surgical procedure in the emergency setting.
Similar content being viewed by others
Background
Emergency laparotomy for secondary peritonitis is still associated with high mortality rates, albeit a substantial decrease was registered over the last decades as a result of improved perioperative care. By implementing evidence-based guidelines, as propagated by the Surving Sepsis Campaign (SSC), more patients with abdominal sepsis survive an otherwise fatal affliction [1,2,3,4]. The adverse effect of this development is an increase in morbidity following prolonged stays on intensive care units (ICUs), leading to debilitating chronical illness, poor clinical outcomes and poor quality of life [2, 5]. There remains an evident need to further optimize emergency care delivery.
Adherence to the SSC recommendations benefits septic patients through the implementation of screening tools such as the SIRS (Systemic Inflammatory Response Syndrome) or MEWS (Modified Early Warning Score) scores for expediting diagnosis and through commitment to early treatment goals summarized in time-framed bundles [1, 3, 4, 6]. Whilst scores for early sepsis recognition, prompt treatment initiation and post-operative intensive care protocols have thoroughly been investigated, there is little evidence-based guidance for the decision-making process during source control surgery (SCS) [6,7,8,9]. Key surgical decisions that highly impact patient outcome, such as anastomosis vs. stoma placement in a peritonitic abdomen are mostly based on the surgeon’s experience and appreciation of the patients’ severity of illness.
The consideration of primary anastomosis during SCS for secondary peritonitis is fairly recent, as for many years the choice, including that of experienced surgeons, was to avoid bowel reconstruction and place stomata instead. An enterostomy negatively affects its carriers both on a physical and psychosocial level [10, 11]. While bound to a life-time risk of stoma-related complications, less than 50% of enterostomy-carriers undergo subsequent restoration of bowel continuity, a procedure with inherent morbidity [10, 12, 13]. The tendency for enterostomy creation persists even in countries with well-developed public health-care systems. According to large-scale audits and observational multicentric studies, just about one quarter of patients undergoing emergency left-sided colonic resection receive a primary anastomosis [14, 15]. This occurs despite growing evidence that in many cases primary bowel reconstruction can be safely performed, even in patients with perforated diverticulitis and purulent or fecal peritonitis [16,17,18]. Addressing the same issue for small bowel perforation with peritonitis, a meta-analysis concluded that there is no sufficient data to issue evidence-based recommendations of whether and when an anastomosis can safely be placed [8]. Even the recent Enhanced Recovery after Surgery (ERAS®) Society and the World Society of Emergency Surgery (WSES) guidelines for emergency laparotomy refrain from issuing detailed recommendations on the surgical approach due to lack of data or need to extrapolate from data derived from elective surgery, leaving the decision of primary anastomosis placement at the discretion of the operating surgeon [2, 7].
The surgical strategy needs of course to be tailored to the patients’ pre-existing conditions and pathophysiological response to the peritoneal contamination, ranging from compensated inflammation to septic shock, as well as to the intraoperative finding. While for elective surgery risk factors for anastomotic leakage have been identified [19, 20], and scoring systems have been developed [21], these data remain scarce in the emergency setting. Among the preoperative tumor-unrelated parameters, the systematic review by McDermott et al. found male sex, American Society of Anesthesiologists (ASA) fitness grade, renal disease, obesity, hypoalbuminemia as a marker of a poor nutritional status, and an indication for emergency surgery to significantly increase the risk of colorectal anastomotic leaks [20]. Two of the largest observational cohort studies analyzing bowel resection with or without primary reconstruction during emergency laparotomy identified fecal contamination as an independent predictor for suture leakage [14, 22]. Both patient cohorts were heterogenous with only 10–30% having peritonitis as an indication for emergency surgery. The authors acknowledged that the lack of data depicting preoperative nutritional deficits limited their risk assessment, as malnutrition has repeatedly been identified as an independent predictor of anastomotic leakage and sepsis [22,23,24]. Low serum albumin, a high C-reactive protein (CRP)-albumin ratio and low serum choline esterase (sCHE) as markers of malnutrition have been linked to a disturbed postoperative wound healing, including that of gastrointestinal (GI) sutures and to a poor prognosis in septic patients, highlighting the need of taking these factors into consideration when placing sutures in a septic surrounding [23,24,1).
Secondary peritonitis requiring SCS was caused in similar proportions in both patient subgroups by gastrointestinal perforation (75.7% vs. 62.5%) or disruption of electively placed gastrointestinal sutures (24.3% vs. 37.5%). There was no significant difference in the location (small vs. large bowel) of the sutures placed during SCS. The length of source control procedures and intraoperative blood loss did not significantly differ in patients with intact vs. insufficient sutures (Table 2).
Postoperative outcomes of patients with lower GI sutures placed during SCS for secondary peritonitis
While SOFA scores immediately upon postoperative ICU admittance were similarly elevated in both patient subgroups, the subgroup of patients with intact enteric sutures had a significantly lower SOFA score on the second postoperative day and therefore a significant improvement in organ functionality.
Both incisional as well as intra-abdominal space infection were significantly higher in the subgroup of patients with insufficient enteric sutures. These patients also had a significantly prolonged stay on the ICU of a median of 8 days, almost three times longer than the intensive care period required by patients with intact sutures. The in-hospital mortality of 38.3% was also significantly higher in the subgroup of patients with suture leakage, of whom only 25.5% were released in their initial home environment (Table 3).
Univariate and multivariate analysis of preoperative and intraoperative factors associated with leakage of lower GI sutures placed during SCS for secondary peritonitis
The following variables showed a statistically significant association with suture leakage in the univariate analysis (Table 4): preoperative CRP levels (p =0.0232), preoperative sCHE activity (p =0.0019) and the peritonitis extent score (p =0.0045). We chose not to include the MPI in our analysis as at least three of the parameters needed to calculate the MPI (age, sex, malignancy) showed no significant association with our primary outcome measure. Other parameters known to influence the outcome of colorectal sutures placed during elective surgery, such as BMI, chronic steroid intake and ASA-score [19, 20] were not significantly associated with the outcome (intact vs. insufficient) of sutures placed on the lower GI tract during SCS for secondary peritonitis. In the multivariate analysis sCHE activity and the peritonitis extent score remained independent predictors for suture outcome (p =0.0472 and p =0.0234, respectively).
Correlation of sCHE activity with suture outcome and patient survival after SCS for secondary peritonitis
We analyzed the correlation of low preoperative sCHE activity and the development of suture leakage. As a cut-off value we took the lower end of the reference interval of 4.5 kU/L. Patients with a sCHE < 4.5 kU/L (n = 96) developed a significantly higher rate of suture insufficiency (p =0.02) and had a significantly higher mortality (p =0.001) than patients with sCHE activity within the normal range (Fig. 3).
Occurrence of suture leakage and survival of patients in dependence of serum choline esterase activity (sCHE), < 4.5 kU/L vs. ≥ 4.5 kU/L. Shown is the cumulative incidence of suture leakage (a) and the survival (b) after source control surgery (SCS) for secondary peritonitis with suture placement on the lower gastrointestinal tract, in dependence of preoperative sCHE activity
Correlation of CRP/sCHE ratio with patient survival after SCS for secondary peritonitis, in dependence of suture outcome
No multicollinearity issue was detected in the multiple logistic regression model, since the calculated variance inflation factors (VIF) for each independent variable were below 1.5. Nevertheless, there was a negative correlation detected between preoperative CRP and sCHE activity with a Spearman correlation coefficient of − 0.4046. The CRP/sCHE ratio was able to discriminate between death and survival following SCS for secondary peritonitis in both patient subgroups with intact (p =0.0025) and insufficient (p =0.0421) enteric sutures respectively (Fig. 4).
Correlation of peritonitis extent with suture outcome and patient survival after SCS for secondary peritonitis
Patients with a peritonitis extent score of ≥ 18, implying a generalized fecal peritonitis, had a significantly higher incidence (p =0.0014) of enteric suture leakage compared to patients with a less severe degree of peritonitis. There was no significant difference but a noticeable trend (p =0.0788) in patient survival when taking the extent of peritoneal contamination into account (Fig. 5).
Occurrence of suture leakage and survival of patients in dependence of peritonitis extent. Shown is the cumulative incidence of suture leakage (a) and the survival (b) after source control surgery for secondary peritonitis with suture placement in the lower gastrointestinal tract, in dependence of the intraoperatively detected peritonitis extent, quantified through the peritonitis extent score (Fig. 2b in Material and Methods)
Discussion
This study aimed to identify quantifiable preoperative and intraoperative parameters associated with a high risk of leakage for sutures placed on the lower GI tract during SCS for secondary peritonitis. These parameters could serve as an everyday tool for surgeons to decide between a primary intestinal reconstruction vs. enterostomy placement. In our patient group, 25.1% of the sutures placed under these adverse emergency conditions developed a leakage in the early postoperative course, far surpassing the insufficiency rates of lower GI sutures placed under elective conditions [20]. In fact, emergency surgery is a well-known independent risk factor for anastomotic leakage after colorectal surgery [20]. After elective colorectal cancer surgery, the reported incidence of anastomotic leakage ranges between 1 and 19%, with higher leakage rates after left colonic and rectal resections compared to right colonic resections [20]. In our patient collective 25% of the small to large bowel sutures and 27% of large to large bowel sutures developed a leakage as opposed to the reported insufficiency rates of 1–4% and 2–19%, respectively, under elective conditions [20, 31]. Most data concerning incidence and predisposing factors for lower GI suture leakage derive from elective colorectal surgery, leaving a marked paucity of information on the issue of primary suture placement during emergency laparotomy, with the exception of perforated diverticular disease. For perforated diverticulitis with purulent or fecal generalized peritonitis a series of randomized controlled trials (RCTs) triggered a shift in the indoctrinated non-restorative Hartmann approach by presenting primary anastomosis as a feasible alternative [17, 32,33,34]. In most of the mentioned RCTs, primary bowel reconstruction in the acute setting was accompanied by the placement of a diverting enterostomy by study design [32,33,34]. Only the LADIES trial allowed surgeons to decide whether or not to place a diverting enterostomy when performing primary reconstruction [17]. In our study, placement of a diverting stoma was defined as an exclusion criterium because of the high incidence of non-clinical (asymptomatic) leakage of distal sutures reported in the literature [35].
In an attempt to facilitate the choice of the appropriate surgical procedure in patients with generalized peritonitis due to perforated diverticulitis, a recent position paper defined septic shock, overall fitness to surgery and peritonitis severity as important factors to consider in the decision-making process [18]. While the notion of septic shock is clearly defined by the SEPSIS-3 consensus definitions, no explicit easy-to-use, “surgeon-friendly” scoring system for pre- or intraoperative assessment could be recommended based on current evidence. Immunocompetence, ASA-Score and MPI were suggested as adjutants in choosing restorative or non-restorative resections in hemodynamically stable patients [18].
As current guidelines and position papers ultimately leave the choice of the emergency operative procedure in the surgeons’ hands, the results of Karliczek et al. showing surgeons’ assessment to be a poor predictor for anastomotic leakage further consolidates the need of identifying objective criteria for selecting patients for primary bowel reconstruction under peritonitic conditions [36].
By the a priori exclusion of non-restorative resections, hemodynamic instable patients for which damage control surgery is the only obvious and valid option are not included in the present study. The preoperative ASA score did not discriminate between patients develo** suture leakage and those who did not in our patient cohort. Neither did the intake of immunosuppressives or the chronic use of corticosteroids. The extent of peritonitis was, however, an independent predictor of suture outcome in the multivariate analysis. We chose to evaluate a simplified form of the MPI, developed to solely assess the extent and quality of the intraoperatively determined peritonitis for a number of reasons. First, the MPI was originally developed in 1987 for predicting postoperative morbidity in a cohort that also included peritonitis due to upper GI perforation but excluded postoperative peritonitis and mesenteric infarction [37]. Neither inclusion and exclusion criteria nor primary outcome matched the purpose of our study. Second, the MPI includes various parameters such as age, sex, preexisting malignancy that did not influence our primary outcome parameter in the univariate analysis. Third, it is easier for the operating surgeon to simply discriminate between purulent or fecal peritonitis and between localized or generalized peritonitis than to calculate a more intricate score. Our data show that patients with generalized fecal peritonitis developed a significantly higher rate of suture leakage (p =0.0014) than patients with less extensive peritonitis, while also showing a trend (p =0.0788) in the mortality rate.
The pathophysiological events triggered within the peritoneal cavity by the spillage of intestinal content seem to critically impact the complex and incompletely understood healing process of the sutured intestinal wall. Altered peripheral blood perfusion, bowel distention and intestinal wall edema are just few of the macroscopic changes imposing a greater degree of difficulty for the surgeon attempting primary bowel repair. The alterations on a microscopic and molecular level are just as intricate, as inflammatory status, microbiome and genetics all seem to affect intestinal suture healing [38]. In a histologic analysis of colonic tissue samples Stumpf et al. identified a preexisting impairment in collagen metabolism as a possible risk factor for the healing of enteric sutures [39]. Polymorphisms in lipid signaling and metabolic pathways are also thought to predispose to altered intestinal suture healing, underlining the importance of the preoperative patient status [38].
In our study, sCHE activity was the only relevant preoperative parameter identified as having a significant predictive value for suture outcome in the multivariate analysis. We deliberately chose to analyze sCHE activity instead of albumin in order to avoid data distortion by parenteral albumin infusions in patients that were hospitalized previous to emergency surgery. In support of sCHE as a predictor for anastomotic healing Antolovic et al. identified low preoperative sCHE levels as an independent risk factor for bile leakage in 519 patients who underwent hepaticojejunostomy [40]. In an emergency setting, our study is one of the few approaching the issue of preoperative predictors for a successful primary bowel reconstruction. Various studies have validated sCHE as a marker of nutritional status, correlating low sCHE levels to sarcopenia and to a high nutritional risk in critically ill patients treated on ICUs [26, 41, 42]. Beside the critically ill, oncologic patients are another group for which malnutrition importantly influenced postoperative morbidity and mortality [43, 44]. In patients with colorectal cancer, low sCHE levels were associated with poor 5-year overall and disease-specific survival rates [43], whereas nutritional support led to an increase in sCHE levels and in body weight [45]. In an analysis of 453 prospectively recruited treatment-naïve cancer patients, without manifest hepatic involvement, Pavo et al. reported that decreased sCHE is associated with an increased all-cause mortality [46]. Interestingly, an inverse correlation of sCHE with CRP was observed (r = − 0.21, p < 0.001) as in our study (r = − 0.40, p < 0.001). In another series of patients with non-malignant disease, sCHE was shown to negatively correlate with further parameters of inflammation, namely interleukin (IL)-6 and tumor necrosis factor alpha (TNF)-α [47].
The observed association with inflammatory parameters is not surprising since the body of evidence linking sCHE to the inflammatory response to injury is continuously growing. SCHE is part of the non-neuronal cholinergic system (NNCS), a complex regulatory network including most immune cells and regulating their function in the setting of local and systemic inflammation [48, 49]. By targeting this system through intraperitoneal injection of CHE inhibitors in an experimental abdominal sepsis model, Hofer et al. showed that locally administered CHE inhibitors led to a reduced production of pro-inflammatory cytokines and improved survival, most probably by increasing acetylcholine levels that control cytokine production [50]. This apparently beneficial effect of a lowered or inhibited CHE activity intuitively stands in contradiction with the clinical observation that a low sCHE activity measured at the clinical onset of sepsis is an independent predictor of worse outcome and higher mortality [51]. However, the anti-inflammatory effect of increased acetylcholine levels is expected to impair host defense against infections, which most probably offsets its benefit [52,53,54]. Several other studies on collectives of critically ill patients requiring ICU care identified low sCHE activity as a relevant predictor of increased mortality [ Low preoperative sCHE activity and a high extent of the intraoperatively determined peritonitis are two easily quantifiable parameters that significantly correlate with a poor outcome of enteric sutures placed during SCS for secondary peritonitis. An objective surgical decision tailored to the patients’ individual pathophysiological pattern helps the surgeons, as they are no longer dependent on subjective considerations alone, while also benefiting the patients through the choice of the appropriate procedure.Conclusion
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- CT:
-
Computer tomography
- ERAS®:
-
Enhanced Recovery after Surgery
- GI:
-
Gastro-intestinal
- Hb:
-
Hemoglobin
- ICUs:
-
Intensive care units
- IL:
-
Interleukin
- IQR:
-
Interquartile range
- MAP:
-
Mean arterial pressure
- MEWS:
-
Modified Early Warning Score
- MPI:
-
Mannheim peritonitis index
- NNCS:
-
Non-neuronal cholinergic system
- OR:
-
Odds ratio
- PCO2 :
-
Partial pressure of carbon dioxide
- PO2 :
-
Partial pressure of oxygen
- POD:
-
Postoperative day
- RCTs:
-
Randomized controlled trials
- sCHE:
-
Serum choline esterase
- SCS:
-
Source control surgery
- SIRS:
-
Systemic Inflammatory Response Syndrome
- SOFA:
-
Sequential organ failure assessment
- SSC:
-
Surving Sepsis Campaign
- SSI:
-
Surgical site infection
- TNF:
-
Tumor necrosis factor
- VIF:
-
Variance inflation factors
- WSES:
-
World Society of Emergency Surgery
References
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36(2):222–31. https://doi.org/10.1007/s00134-009-1738-3.
Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16(1):49. https://doi.org/10.1186/s13017-021-00387-8.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247. https://doi.org/10.1007/s00134-021-06506-y.
van Zanten AR, Brinkman S, Arbous MS, Abu-Hanna A, Levy MM, de Keizer NF, Netherlands Patient Safety Agency Sepsis Expert Group. Guideline bundles adherence and mortality in severe sepsis and septic shock. Crit Care Med. 2014;42(8):1890–8. https://doi.org/10.1097/CCM.0000000000000297.
Cox MC, Brakenridge SC, Stortz JA, Hawkins RB, Darden DB, Ghita GL, et al. Abdominal sepsis patients have a high incidence of chronic critical illness with dismal long-term outcomes. Am J Surg. 2020;220(6):1467–74. https://doi.org/10.1016/j.amjsurg.2020.07.016.
Venkatesh B, Schlapbach L, Mason D, Wilks K, Seaton R, Lister P, et al. Impact of 1-hour and 3-hour sepsis time bundles on patient outcomes and antimicrobial use: a before and after cohort study. Lancet Reg Health West Pac. 2021;2(18): 100305. https://doi.org/10.1016/j.lanwpc.2021.100305.
Scott MJ, Aggarwal G, Aitken RJ, Anderson ID, Balfour A, Foss NB, et al. Consensus guidelines for perioperative care for emergency laparotomy enhanced recovery after surgery (ERAS®) society recommendations part 2-emergency laparotomy: intra- and postoperative care. World J Surg. 2023;47(8):1850–80. https://doi.org/10.1007/s00268-023-07020-6.
Skovsen AP, Burcharth J, Gögenur I, Tolstrup MB. Small bowel anastomosis in peritonitis compared to enterostomy formation: a systematic review. Eur J Trauma Emerg Surg. 2023;49(5):2047–55. https://doi.org/10.1007/s00068-022-02192-7.
Schmidt S, Ismail T, Puhan MA, Soll C, Breitenstein S. Meta-analysis of surgical strategies in perforated left colonic diverticulitis with generalized peritonitis. Langenbecks Arch Surg. 2018;403(4):425–33. https://doi.org/10.1007/s00423-018-1686-x.
Murken DR, Bleier JIS. Ostomy-related complications. Clin Colon Rectal Surg. 2019;32(3):176–82. https://doi.org/10.1055/s-0038-1676995.
Stavropoulou A, Vlamakis D, Kaba E, Kalemikerakis I, Polikandrioti M, Fasoi G, Vasilopoulos G, Kelesi M. “Living with a stoma”: exploring the lived experience of patients with permanent colostomy. Int J Environ Res Public Health. 2021;18(16):8512. https://doi.org/10.3390/ijerph18168512.
Horesh N, Lessing Y, Rudnicki Y, Kent I, Kammar H, Ben-Yaacov A, et al. Considerations for Hartmann’s reversal and Hartmann’s reversal outcomes—a multicenter study. Int J Colorectal Dis. 2017;32(11):1577–82. https://doi.org/10.1007/s00384-017-2897-2.
Resio BJ, Jean R, Chiu AS, Pei KY. Association of timing of colostomy reversal with outcomes following Hartmann procedure for diverticulitis. JAMA Surg. 2019;154(3):218–24. https://doi.org/10.1001/jamasurg.2018.4359.
Aicher BO, Hernandez MC, Betancourt-Ramirez A, Grossman MD, Heise H, Schroeppel TJ, et al. Colorectal resection in emergency general surgery: an EAST multicenter trial. J Trauma Acute Care Surg. 2020;89(6):1023–31. https://doi.org/10.1097/TA.0000000000002894.
Burmas M, Aitken RJ, Broughton KJ. Outcomes following emergency laparotomy in Australian public hospitals. ANZ J Surg. 2018;88(10):998–1002. https://doi.org/10.1111/ans.14847.
Boyce SA, Bartolo DC, Paterson HM, Edinburgh Coloproctology Unit. Subspecialist emergency management of diverticulitis is associated with reduced mortality and fewer stomas. Colorectal Dis. 2013;15(4):442–7. https://doi.org/10.1111/codi.12022.
Lambrichts DPV, Vennix S, Musters GD, Mulder IM, Swank HA, Hoofwijk AGM, et al. Hartmann’s procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol. 2019;4(8):599–610. https://doi.org/10.1016/S2468-1253(19)30174-8.
Nascimbeni R, Amato A, Cirocchi R, Serventi A, Laghi A, Bellini M, et al. Management of perforated diverticulitis with generalized peritonitis. A multidisciplinary review and position paper. Tech Coloproctol. 2021;25(2):153–65. https://doi.org/10.1007/s10151-020-02346-y.
Boccola MA, Buettner PG, Rozen WM, Siu SK, Stevenson AR, Stitz R, et al. Risk factors and outcomes for anastomotic leakage in colorectal surgery: a single-institution analysis of 1576 patients. World J Surg. 2011;35(1):186–95. https://doi.org/10.1007/s00268-010-0831-7.
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102(5):462–79. https://doi.org/10.1002/bjs.9697.
Dekker JW, Liefers GJ, de Mol van Otterloo JC, Putter H, Tollenaar RA. Predicting the risk of anastomotic leakage in left-sided colorectal surgery using a colon leakage score. J Surg Res. 2011;166(1):e27-34. https://doi.org/10.1016/j.jss.2010.11.004.
Bruns BR, Morris DS, Zielinski M, Mowery NT, Miller PR, Arnold K, et al. Stapled versus hand-sewn: a prospective emergency surgery study. An American Association for the Surgery of Trauma multi-institutional study. J Trauma Acute Care Surg. 2017;82(3):435–43. https://doi.org/10.1097/TA.0000000000001354.
Suding P, Jensen E, Abramson MA, Itani K, Wilson SE. Definitive risk factors for anastomotic leaks in elective open colorectal resection. Arch Surg. 2008;143(9):907–11. https://doi.org/10.1001/archsurg.143.9.907.
Lai CC, You JF, Yeh CY, Chen JS, Tang R, Wang JY, et al. Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis. 2011;26(4):473–81. https://doi.org/10.1007/s00384-010-1113-4.
Paliogiannis P, Deidda S, Maslyankov S, Paycheva T, Farag A, Mashhour A, Misiakos E, Papakonstantinou D, Mik M, Losinska J, Scognamillo F, Sanna F, Feo CF, Porcu A, **das A, Zinellu A, Restivo A, Zorcolo L. C reactive protein to albumin ratio (CAR) as predictor of anastomotic leakage in colorectal surgery. Surg Oncol. 2021;38: 101621. https://doi.org/10.1016/j.suronc.2021.101621.
Santarpia L, Grandone I, Contaldo F, Pasanisi F. Butyrylcholinesterase as a prognostic marker: a review of the literature. J Cachexia Sarcopenia Muscle. 2013;4(1):31–9. https://doi.org/10.1007/s13539-012-0083-5.
Peng ZL, Huang LW, Yin J, Zhang KN, **ao K, Qing GZ. Association between early serum cholinesterase activity and 30-day mortality in sepsis-3 patients: a retrospective cohort study. PLoS ONE. 2018;13(8): e0203128. https://doi.org/10.1371/journal.pone.0203128.
Brown LR, McLean RC, Perren D, O’Loughlin P, McCallum IJ. Evaluating the effects of surgical subspecialisation on patient outcomes following emergency laparotomy: a retrospective cohort study. Int J Surg. 2019;62:67–73. https://doi.org/10.1016/j.ijsu.2019.01.010.
Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27. https://doi.org/10.1186/s13017-020-00306-3.
Krecko LK, Hoyos Gomez T, Scarborough JE, Jung HS. Postoperative outcomes after index vs interval cholecystectomy for perforated cholecystitis. J Am Coll Surg. 2021;232(4):344–9. https://doi.org/10.1016/j.jamcollsurg.2020.11.034.
Platell C, Barwood N, Dorfmann G, Makin G. The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis. 2007;9(1):71–9. https://doi.org/10.1111/j.1463-1318.2006.01002.x.
Binda GA, Karas JR, Serventi A, Sokmen S, Amato A, Hydo L, et al. Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis. 2012;14(11):1403–10. https://doi.org/10.1111/j.1463-1318.2012.03117.x.
Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C, et al. A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg. 2012;256(5):819–26. https://doi.org/10.1097/SLA.0b013e31827324ba.
Bridoux V, Regimbeau JM, Ouaissi M, Mathonnet M, Mauvais F, Houivet E, et al. Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg. 2017;225(6):798–805. https://doi.org/10.1016/j.jamcollsurg.2017.09.004.
Fukudome I, Maeda H, Okamoto K, Yamaguchi S, Fujisawa K, Shiga M, et al. Early stoma closure after low anterior resection is not recommended due to postoperative complications and asymptomatic anastomotic leakage. Sci Rep. 2023;13(1):6472. https://doi.org/10.1038/s41598-023-33697-9.
Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam GM. Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Colorectal Dis. 2009;24(5):569–76. https://doi.org/10.1007/s00384-009-0658-6.
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. Der Mannheimer Peritonitis-Index. Ein Instrument zur intraoperativen Prognose der Peritonitis [The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis]. Chirurg. 1987;58(2):84–92.
Lee JA, Chico TJA, Renshaw SA. The triune of intestinal microbiome, genetics and inflammatory status and its impact on the healing of lower gastrointestinal anastomoses. FEBS J. 2018;285(7):1212–25. https://doi.org/10.1111/febs.14346.
Stumpf M, Cao W, Klinge U, Klosterhalfen B, Kasperk R, Schumpelick V. Collagen distribution and expression of matrix metalloproteinases 1 and 13 in patients with anastomotic leakage after large-bowel surgery. Langenbecks Arch Surg. 2002;386(7):502–6. https://doi.org/10.1007/s00423-001-0255-9.
Antolovic D, Koch M, Galindo L, Wolff S, Music E, Kienle P, et al. Hepaticojejunostomy—analysis of risk factors for postoperative bile leaks and surgical complications. J Gastrointest Surg. 2007;11(5):555–61. https://doi.org/10.1007/s11605-007-0166-3.
Liu J, Shao T, Chen H, Ma C, Lu X, Yang X, et al. Serum cholinesterase as a new nutritional indicator for predicting weaning failure in patients. Front Med (Lausanne). 2023;12(10):1175089. https://doi.org/10.3389/fmed.2023.1175089.
Cacciatore F, Della-Morte D, Basile C, Curcio F, Liguori I, Roselli M, et al. Butyryl-cholinesterase is related to muscle mass and strength. A new biomarker to identify elderly subjects at risk of sarcopenia. Biomark Med. 2015;9(7):669–78. https://doi.org/10.2217/bmm.15.28.
Yamamoto M, Saito H, Uejima C, Tanio A, Tada Y, Matsunaga T, et al. Combination of serum albumin and cholinesterase levels as prognostic indicator in patients with colorectal cancer. Anticancer Res. 2019;39(2):1085–90. https://doi.org/10.21873/anticanres.13217.
Bi Y, Zhang J, Zeng D, Chen L, Ye W, Yang Q, et al. Cholinesterase is associated with prognosis and response to chemotherapy in advanced gastric cancer. Pathol Oncol Res. 2021;25(27): 580800. https://doi.org/10.3389/pore.2021.580800.
Bozzetti F. Effects of artificial nutrition on the nutritional status of cancer patients. J Parenter Enteral Nutr. 1989;13(4):406–20. https://doi.org/10.1177/0148607189013004406.
Pavo N, Raderer M, Goliasch G, Wurm R, Strunk G, Cho A, et al. Subclinical involvement of the liver is associated with prognosis in treatment naïve cancer patients. Oncotarget. 2017;8(46):81250–60. https://doi.org/10.18632/oncotarget.17131.
Hubbard RE, O’Mahony MS, Calver BL, Woodhouse KW. Plasma esterases and inflammation in ageing and frailty. Eur J Clin Pharmacol. 2008;64(9):895–900. https://doi.org/10.1007/s00228-008-0499-1.
Wessler I, Kirkpatrick CJ. Acetylcholine beyond neurons: the non-neuronal cholinergic system in humans. Br J Pharmacol. 2008;154(8):1558–71. https://doi.org/10.1038/bjp.2008.185.
Kawashima K, Fujii T, Moriwaki Y, Misawa H, Horiguchi K. Non-neuronal cholinergic system in regulation of immune function with a focus on α7 nAChRs. Int Immunopharmacol. 2015;29(1):127–34. https://doi.org/10.1016/j.intimp.2015.04.015.
Hofer S, Eisenbach C, Lukic IK, Schneider L, Bode K, Brueckmann M, et al. Pharmacologic cholinesterase inhibition improves survival in experimental sepsis. Crit Care Med. 2008;36(2):404–8. https://doi.org/10.1097/01.CCM.0B013E31816208B3.
Zivkovic AR, Decker SO, Zirnstein AC, Sigl A, Schmidt K, Weigand MA, et al. A sustained reduction in serum cholinesterase enzyme activity predicts patient outcome following sepsis. Mediators Inflamm. 2018;29(2018):1942193. https://doi.org/10.1155/2018/1942193.
van Westerloo DJ, Giebelen IA, Florquin S, Daalhuisen J, Bruno MJ, de Vos AF, et al. The cholinergic anti-inflammatory pathway regulates the host response during septic peritonitis. J Infect Dis. 2005;191(12):2138–48. https://doi.org/10.1086/430323.
Kessler W, Traeger T, Westerholt A, Neher F, Mikulcak M, Müller A, et al. The vagal nerve as a link between the nervous and immune system in the instance of polymicrobial sepsis. Langenbecks Arch Surg. 2006;391(2):83–7. https://doi.org/10.1007/s00423-006-0031-y.
Engel O, Akyüz L, da Costa Goncalves AC, Winek K, Dames C, Thielke M, et al. Cholinergic pathway suppresses pulmonary innate immunity facilitating pneumonia after stroke. Stroke. 2015;46(11):3232–40. https://doi.org/10.1161/STROKEAHA.115.008989.
Yue C, Zhang C, Ying C, Jiang H. Reduced serum cholinesterase is an independent risk factor for all-cause mortality in the pediatric intensive care unit. Front Nutr. 2022;24(9): 809449. https://doi.org/10.3389/fnut.2022.809449.
Bahloul M, Kharrat S, Makni S, Baccouche N, Ammar R, Eleuch A, et al. Prognostic value of serum cholinesterase activity in severe SARS-CoV-2-infected patients requiring intensive care unit admission. Am J Trop Med Hyg. 2022;107(3):534–9. https://doi.org/10.4269/ajtmh.21-0934.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding. A.-L.A. and M.R. was supported by the Justus-Liebig University Giessen Clinician Scientist Program in Biomedical Research (JLU-CAREER) funded by the German Research Foundation (DFG No. GU405/14-1).
Author information
Authors and Affiliations
Contributions
A-LA, AH and SP conceived the project and developed the methodology. RE, LM and AKP are responsible for data acquisition. A-LA, MR and SP performed the statistical analysis and interpreted the data. A-LA and SP wrote the manuscript. AH, TS, MS, VG aided in interpreting the results and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This exploratory, retrospective single-center cohort study was performed in accordance with the latest version of the Declaration of Helsinki and was approved by the local ethics committee of the Medical Faculty of the University of Giessen (approval No. 20/22). Due to the retrospective nature of the study, the need for a written informed consent was waived by the ethics committee. The data are collected, the manuscript is written and submitted in accordance with the COPE and STROBE guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amati, A.L., Ebert, R., Maier, L. et al. Reduced preoperative serum choline esterase levels and fecal peritoneal contamination as potential predictors for the leakage of intestinal sutures after source control in secondary peritonitis. World J Emerg Surg 19, 21 (2024). https://doi.org/10.1186/s13017-024-00550-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-024-00550-x