Abstract
Background
COVID-19 infection continues all over the world, causing serious physical and psychological impacts to patients. Patients with COVID-19 infection suffer from various negative emotional experiences such as anxiety, depression, mania, and alienation, which seriously affect their normal life and is detrimental to the prognosis. Our study is aimed to investigate the effect of psychological capital on alienation among patients with COVID-19 and the mediating role of social support in this relationship.
Methods
The data were collected in China by the convenient sampling. A sample of 259 COVID-19 patients completed the psychological capital, social support and social alienation scale and the structural equation model was adopted to verify the research hypotheses.
Results
Psychological capital was significantly and negatively related to the COVID-19 patients’ social alienation (p < .01). And social support partially mediated the correlation between psychological capital and patients’ social alienation (p < .01).
Conclusion
Psychological capital is critical to predicting COVID-19 patients’ social alienation. Social support plays an intermediary role and explains how psychological capital alleviates the sense of social alienation among patients with COVID-19 infection.
Similar content being viewed by others
Background
Introduction
Currently, COVID-19 is still widespread around the world [4, 15] and the pandemic is still difficult to prevent and constrain in China as there are sporadic and clustered COVID-19 outbreaks taking place [1, 7]. Up to now, no effective drug for preventing COVID-19 is available [41]. The COVID-19 epidemic is a public health emergency that not only endangers patients’ physical health but also has an emotional impact on individuals and may result in related psychological problems [11, 22]. Patients with COVID-19 infection may experience common psychological symptoms, such as anxiety, insomnia, tension, as well as excessive attention to the body and disease recovery [39, 49]. The COVID-19 epidemic has created a situation where many factors that contribute to poor mental health are made worse. A study on the Lancet estimated an addition of 53.2 million cases of major depression and 76.2 million cases of anxiety disorder globally due to the COVID-19 pandemic [17]. These psychological problems are derived from the uncertainty about the prognosis of COVID-19 and the social discrimination against contagious novel coronavirus [36, 52]. These problems will result in a sense of alienation in patients. Social alienation has a negative impact on patients’ physical and mental health, and is detrimental to both the healing of sickness and the societal integration [8].
Social alienation is the automatic alienation that occurs between people and their families, other people, and society. This feeling of helplessness and loneliness leads to negative behaviors like avoidance and rejection [6, 33]. With COVID-19, the patients are labeled as something others fear of and become a symbol of awe and alienation for others, which has an adverse effect on patients’ physical and mental health and makes it difficult for them to reintegrate into society [38]. At present, there are few studies on social alienation of patients with COVID-19 infection, most of which focus on the negative emotion caused by COVID-19 [29, 45, 50]. Therefore, the purpose of our study is to carry out research to investigate the sense of alienation in patients with COVID-19 infection, in order to ascertain the severity of their social alienation and explore its underlying mechanisms, so as to provide references for alleviating the social alienation of COVID-19 patients and help them to maintain their mental health and to better integrate into society.
Psychological capital refers to the state of being psychologically positive as exhibited in individuals during their growth [3]. Good psychological capital can buffer the impact of negative emotions [9]. At present, psychological capital is a topic that has been extensively studied [25, 46, 58, 31]. Accordingly, we believe that psychological capital, social support and social alienation are interrelated, where social support may play an intermediary role between psychological capital and social alienation. Hence, the present study is designed to investigate the effect of psychological capital on patients’ feelings of social alienation and the mediating role of social support among patients with COVID-19. As such, we attempted to explore the impact of social alienation on COVID-19 patients and provide insights for reducing their social alienation.
Literature review and hypotheses
Psychological capital and social alienation
Psychological capital is a psychological element and a psychological resource that could promote personal growth and development [51]. Psychological capital mainly includes four key dimensions: (a) Self-efficacy, a personal assessment of one’s ability to succeed. (b) Hope, which alludes to positive intentions or goals. (c) Tenacity, or a person’s unyielding spirit and perseverance. (d) Optimism, which is the state of being filled with confidence and optimism for the future [40].
Considering the infectious nature of the disease, COVID-19 patients need to be isolated in treatment after diagnosis [20]. Patients who are physically isolated develop a psychological distance to the outside world [14]. The society discriminates against the patients tested positive as carriers and communicators of the virus and this discrimination still exists even after their recovery, because patients have a possibility of reinfection. All of these make the patients feel socially excluded and less connected with others, and exhibit autistic emotions [23]. Social alienation mainly consists of four dominant dimensions: (a) Self-alienation, which is a denial of oneself. (b) Social isolation, the feeling of loneliness when interacting with others. (c) Powerlessness, the feeling brought on by a lack of accomplishment. (d) Meaningless, a sense of loss due to a lack of a goal or direction in life [60].
Research shows that good psychological capital can help individuals find solutions to problems [47]. Hope and optimism, in particular, can help individuals to eliminate the entrenched discrimination and respond to this discrimination with a positive attitude [26]. Here, we argue that psychological capital can alleviate social alienation. People who have supportive psychological capital can overcome their social isolation. Resilience can improve a person’s capacity to handle stress and withstand unfavorable feelings like powerlessness and helplessness in the face of challenges [16]. Therefore, based on these arguments, our first hypothesis is:
Hypothesis 1
Psychological capital is directly related to patients’ social alienation and can alleviate social alienation.
Social support as a mediator
Social support refers to the objective support from the outside to the individual and the subjective support perceived by the individual [43, 27]. And social support was identified as one of the protective factors against emotional loneliness during the COVID-19 pandemic [28]. The mental condition of COVID-19 patients with is closely linked to social support they received, and good social support can relieve their negative emotions such as tension and anxiety [21]. However, the studies currently do not have sufficient evidence in the impact of social support on patients’ social alienation. Thus, it is of great importance to investigate the relationship between social support and social alienation in COVID-19 patients.
Presently, there are limited investigations on the relations among psychological capital, social support and social alienation in patients with COVID-19. Therefore, it is crucial to investigate how social alienation affects COVID-19 patients in order to support their active social integration, preserve their mental health, and accelerate disease healing. We thus anticipate that social support functions as a mediator between psychological capital and social alienation. Individuals with strong psychological capital can seek greater social support, and good social support can in turn alleviate their social alienation. Taken together, we propose that:
Hypothesis 2
Social support mediates the relationship between psychological capital and social alienation.
Methods
Participants and data collection
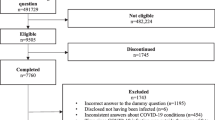
Participants were collected by convenient sampling, and 284 COVID-19-infected patients from a shelter hospital were selected as study subjects. With the help of the head nurses, we distributed electronic questionnaires to patients in the shelter hospital from April to May 2022 in Shanghai. All the patients diagnosed with COVID-19 meet the inclusion criteria with those who refused to participate or were absent during the survey excluded. Participants’ informed consent was acquired before the survey was conducted. The time required to complete the phone-sent questionnaire was under control in just over 30 min. The questionnaire’s cover page reaffirmed the study’s objectives and importance. The survey was completed in an anonymous manner with a promise to protect the privacy and to use the data for research purpose only. Patients were informed that they could withdraw from the study at any time for any reason. Thirteen patients dropped out of the study midway through, seven questionnaires were determined to be incomplete, and five surveys were deemed invalid because of their excessive uniformity. After the questionnaires were collected, 259 of them were determined to be valid with an effective recovery rate of 91.97%.
Measures
Psychological capital
Psychological capital was measured using the Psychological Capital Questionnaire (PCQ) [13]. PCQ is a higher-order construct consisting of 4 subscales, each comprised of 6 items (with a total of 24 items). The subscales include self-efficacy, hope, tenacity, and optimism. Example items include ‘I believe there are many different ways to solve the problem’ and ‘I believe I can analyze long-term problems and find solutions’. A 6-point Likert scale was adopted, ranging from 6 (totally agree) to 1 (totally disagree) with higher scores indicating higher psychological capital. The scale is widely used in Chinese population research and has good applicability [10, 54]. In our research, the scale also shows good reliability and validity; its Cronbach’s alpha coefficient was 0.87 and varied between 0.81 and 0.90 for each of the scale’s 4 dimensions.
Social support
Social support was measured using the Social Support Rate Scale (SSRS) [30]. SSRS is a higher-order construct consisting of 3 subscales, with a total of 10 questions items. The subscales fall into objective support (3 items), subjective support (4 items) and utilization of support (3 items). Example items include ’How many close friends do you have?’ and ‘Who comforted and cared for you when you were in trouble?’; Higher scores indicate higher social support. The scale is widely applied in Chinese populations, showing a good applicability [44, 58, With the assistance of head nurses in the shelter hospital, 259 out of 284 patients completed the survey with a response rate of 91.97%, among whom 144 were male (55.60%) and 115 were female (44.40%). The subjects had an average age of 41.87 years (SD = 12.62); 97 subjects were from urban areas (37.45%) and 162 were from rural areas (62.55%); 184 patients had high-school degrees or less (71.04%), 73 had bachelor's degrees (28.19%), and 2 had master's degrees (0.77%); 10 were unmarried (3.86%), 236 were married (91.12%), and 13 were divorced or widowed (5.02%). Table 1 shows the scores of the 3 scales and subscales. The psychological capital score of 259 patients with COVID-19 was (104.01 ± 14.89) with the social support score of (37.20 ± 7.88), and the social alienation score of (35.39 ± 4.64). The scores of other dimensions were presented in Table 1. Table 2 displays the Pearson correlation coefficients among variables in the survey. The results showed that psychological capital and its 4 dimensions have significantly positive correlations with social support (r = 0.58, p < 0.01; r = 0.54, p < 0.01; r = 0.58, p < 0.01; r = 0.50, p < 0.01; r = 0.36, p < 0.01) and have significantly negative correlations with social alienation (r = − 0.36, p < 0.01; r = − 0.34, p < 0.01; r = − 0.39, p < 0.01; r = − 0.38, p < 0.01; r = − 0.36, p < 0.01). Social alienation and its 4 dimensions had a negative correlation with social support (r = − 0.30, p < 0.01; r = − 0.31, p < 0.01; r = − 0.33, p < 0.01; r = − 0.34, p < 0.01). To verify hypothesis 1, we firstly tested the direct effect model, with the results indicating a good fit in the direct effect model: χ2 = 41.91, df = 19, χ2/df = 2.21, CFI = 0.95, TLI = 0.93, RMSEA = 0.05, 90%CI: 0.04–0.09, SRMR = 0.05 (p < 0.01) (as shown in Fig. 1). Psychological capital was negatively correlated with social alienation (β = − 0.46, p < 0.01). Then we performed 2000 bootstrap** resamples to justify the 95% CI of the total direct effect of psychological capital on social alienation, which showed 95% CI for the total direct effect (− 0.65, − 0.27). And psychological capital could justify the 31% variance of social alienation. Next, we tested a mediating effect model to verify hypothesis 2 that whether social support mediates psychological capital and social alienation. We repeated this process 2000 times to obtain an empirical approximation of the sampling distribution, and to obtain estimates and confidence intervals for this indirect effect. The confirmatory factor analysis revealed that the three-factor model had an adequate fit to the data: χ2 = 131.32, df = 37, χ2/ df = 3.55, CFI = 0.91, TLI = 0.92, RMSEA = 0.05, 90%CI: 0.03–0.07, SRMR = 0.07 (p < 0.01) (as shown in Fig. 2). Psychological capital was positively related to social support (β = 0.59, p < 0.01), while negatively related with social alienation (β = − 0.13, p < 0.01). And social support also showed a negative correlation with social alienation (β = − 0.37, p < 0.01). We performed 2000 bootstrap** resamples to justify the 95% CI of the indirect effect of psychological capital on social alienation via social support. The results showed that the 95% CI of the mediating effect was (− 0.27, − 0.17), with the total effect of − 0.46 and the indirect effect of − 0.22. The indirect effect accounted for 47.82% of the total effect of psychological capital on social alienation (Table 3). Through the investigation of 259 COVID-19 patients, we found that their psychological capital can directly predict social alienation. Psychological capital is a positive psychological state which can buffer the negative effects of negative emotions [42]. The negative correlation between psychological capital and social alienation was verified by the correlation analysis in patients with COVID-19 infection (p < 0.01). Following an infection, the patient is very contagious, and the effects of this COVID-19 remained unclear at this moment [19, 61]. Additionally, being isolated in such an unfamiliar environment as the shelter hospital, it is easy for the patients to develop negative psychological conditions such as closure, refusal to communicate with others, fear and so on [12]. If with positive psychological capital, when facing difficulties, these patients would show positive responses such as hope, optimism, resilience, and self-efficacy. These positive reactions will encourage them to accept the reality of infection, actively receive treatment against the disease, and avoid the alienation feelings [48]. Specifically, when the patient is optimistic about his or her treatment and prognosis rather than abandons himself, it helps to create a sense of self-worth and avoid being isolated from the external environment. Research shows that mindfulness meditation might be a viable low-cost intervention to mitigate the psychological impact of the COVID-19 crisis [31, 32], and that of Yarcheski & Mahon [55] suggesting that the higher the level of perceived social support, the higher the level of psychological capital. Calati et al. [5] proposed that social support can negatively predict people's sense of alienation, which means that the more the social support, the less lonely people tend to feel. Social support can alleviate the negative emotional experience of patients with COVID-19; specifically, the more external support they receive from friends, coworkers, and family members, the less social alienation they feel [56]. Lack of adequate psychological capital among patients will result in a loss in interpersonal and adaptive abilities after the disease. Subsequently, it will make people feel isolated from others and reluctant to seek social help; and ultimately increase their sense of social alienation. On the contrary, a patient who has a strong psychological capital can adjust to changes well, actively fight against the disease, and seek help from the outside. This improved social capital enables people to obtain social support, foster a sense of belonging, and feel less isolated, thus leading to the lowered sense of social alienation. Therefore, medical personnel should be completely aware of the critical role that social support plays in reducing social alienation in COVID-19 patients, as the patients are vulnerable to unfair treatment such as social discrimination, exclusion, isolation and alienation [62, 63]. Medical personnel should provide support especially psychological assistance to patients. They could allay the patients' worries by reassuring them and sharing successful cases of patients recovering from COVID-19. Psychological capital is critical to predicting COVID-19 patients' social alienation. Social support plays an intermediary role and explains how psychological capital alleviates the sense of social alienation among patients with COVID-19 infection.Results
Demographic characteristics of patients with COVID-19 infection and variables score
Correlation analysis of psychological capital, social support and social alienation
Verification of research hypotheses
Discussion
The direct effect of psychological capital on social alienation
Conclusions
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to the protection of the privacy of consulting experts but are available from the corresponding author (906963251@qq.com) on reasonable request.
References
Araf Y, Akter F, Tang YD, Fatemi R, Parvez MSA, Zheng C, Hossain MG. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022;94(5):1825–32. https://doi.org/10.1002/jmv.27588.
Bae SR, Hong HJ, Chang JJ, Shin SH. The association between Korean clinical nurses’ workplace bullying, positive psychological capital, and social support on burnout. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182111583.
Bi X, ** J. Psychological capital, college adaptation, and internet addiction: an analysis based on moderated mediation model. Front Psychiat. 2021;12:712964. https://doi.org/10.3389/fpsyt.2021.712964.
Biswas S, Mandal AK. Optimization strategies of human mobility during the COVID-19 pandemic: a review. Math Biosci Eng. 2021;18(6):7965–78. https://doi.org/10.3934/mbe.2021395.
Calati R, Ferrari C, Brittner M, Oasi O, Olié E, Carvalho AF, Courtet P. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord. 2019;245:653–67. https://doi.org/10.1016/j.jad.2018.11.022.
Chen DR, Lu HH. Social alienation of adolescents with obesity in classrooms: a multilevel approach. J Adolesc. 2022;94(1):81–91. https://doi.org/10.1002/jad.12001.
Chen F, Zhu S, Dai Z, Hao L, Luan C, Guo Q, Zhang Y. Effects of COVID-19 and mRNA vaccines on human fertility. Hum Reprod. 2021;37(1):5–13. https://doi.org/10.1093/humrep/deab238.
Chen WC, Chen SJ, Zhong BL. Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in Wuhan, China, During the COVID-19 Pandemic. J Geriatr Psychiatry Neurol. 2022;35(2):215–22. https://doi.org/10.1177/08919887221078564.
Chevalier S, Calmé I, Coillot H, Le Rudulier K, Fouquereau E. How can students’ entrepreneurial intention be increased? the role of psychological capital, perceived learning from an entrepreneurship education program, emotions and their relationships. Eur J Psychol. 2022;18(1):84–97. https://doi.org/10.5964/ejop.2889.
Cui CY, Wang Y, Zhang Y, Chen S, Jiang N, Wang L. The development and validation of the psychological capital questionnaire for patients with Cancer the psychological capital questionnaire. BMC Cancer. 2021;21(1):1194. https://doi.org/10.1186/s12885-021-08960-9.
Currò CT, Ciacciarelli A, Vitale C, Vinci ES, Toscano A, Vita G, Autunno M. Chronic migraine in the first COVID-19 lockdown: the impact of sleep, remote working, and other life/psychological changes. Neurol Sci. 2021;42(11):4403–18. https://doi.org/10.1007/s10072-021-05521-7.
Ding S, Dong L, Chen L, Gao F. Fear of progression in patients with mild or common type COVID-19. Int J Nurs Pract. 2022. https://doi.org/10.1111/ijn.13085.
Dirzyte A, Perminas A, Biliuniene E. Psychometric properties of satisfaction with life scale (SWLS) and psychological capital questionnaire (PCQ-24) in the Lithuanian population. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18052608.
Economou M. Social distance in COVID-19: drawing the line between protective behavior and stigma manifestation. Psychiatriki. 2021;32(3):183–6. https://doi.org/10.22365/jpsych.2021.025.
Fiolet T, Kherabi Y, MacDonald CJ, Ghosn J, Peiffer-Smadja N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review. Clin Microbiol Infect. 2022;28(2):202–21. https://doi.org/10.1016/j.cmi.2021.10.005.
Furman G, Bluvstein I, Itzhaki M. Emotion work and resilience of nurses and physicians towards Palestinian authority patients. Int Nurs Rev. 2021;68(4):493–503. https://doi.org/10.1111/inr.12672.
Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. (2021). Lancet, 398(10312), 1700–1712. https://doi.org/10.1016/s0140-6736(21)02143-7
Gu J, Yang C, Zhang K, Zhang Q. Mediating role of psychological capital in the relationship between social support and treatment burden among older patients with chronic obstructive pulmonary disease. Geriatr Nurs. 2021;42(5):1172–7. https://doi.org/10.1016/j.gerinurse.2021.07.006.
Guo T, Liu X, Xu C, Wang J, Yang L, Shi H, Dai M. Fangcang Shelter Hospital in Wuhan: a radiographic report on a cohort of 98 COVID-19 patients. Int J Med Sci. 2020;17(14):2125–32. https://doi.org/10.7150/ijms.48074.
Hayden ME, Rozycki D, Tanabe KO, Pattie M, Casteen L, Davis S, Holstege CP. COVID-19 isolation and quarantine experience for residential students at a large four-year public university. Am J Public Health. 2021;111(10):1772–5. https://doi.org/10.2105/ajph.2021.306424.
Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, Ma P. Epidemiology of mental health problems in COVID-19: a review. Research. 2020;9:636.
Hu B, Ruan Y, Liu K, Wei X, Wu Y, Feng H, Wang T. A mid-to-long term comprehensive evaluation of psychological distress and erectile function in COVID-19 recovered patients. J Sex Med. 2021;18(11):1863–71. https://doi.org/10.1016/j.jsxm.2021.08.010.
Huynh G, Nguyen HV, Vo LY, Le NT, Nguyen HTN. Assessment of insomnia and associated factors among patients who have recovered from COVID-19 in Vietnam. Patient Prefer Adherence. 2022;16:1637–47. https://doi.org/10.2147/ppa.S371563.
Jarden RJ, Jarden A, Weiland TJ, Taylor G, Bujalka H, Brockenshire N, Gerdtz MF. New graduate nurse wellbeing, work wellbeing and mental health: a quantitative systematic review. Int J Nurs Stud. 2021;121:103997. https://doi.org/10.1016/j.ijnurstu.2021.103997.
Jurek K, Niewiadomska I. Relationship between psychological capital and quality of life among seniors working after retirement: the mediating role of hope of success. PLoS One. 2021;16(11):e0259273. https://doi.org/10.1371/journal.pone.0259273.
Krafft AM, Martin-Krumm C, Fenouillet F. Adaptation, further elaboration, and validation of a scale to measure hope as perceived by people: discriminant value and predictive utility vis-à-vis dispositional hope. Assessment. 2019;26(8):1594–609. https://doi.org/10.1177/1073191117700724.
Labrague LJ. Psychological resilience, co** behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. 2021;29(7):1893–905. https://doi.org/10.1111/jonm.13336.
Labrague LJ, De Los Santos JAA, Falguera CC. Social and emotional loneliness among college students during the COVID-19 pandemic: the predictive role of co** behaviors, social support, and personal resilience. Perspect Psychiatr Care. 2021;57(4):1578–84. https://doi.org/10.1111/ppc.12721.
Li J, Su Q, Li X, Peng Y, Liu Y. COVID-19 negatively impacts on psychological and somatic status in frontline nurses. J Affect Disord. 2021;294:279–85. https://doi.org/10.1016/j.jad.2021.07.031.
Lin FH, Yih DN, Shih FM, Chu CM. Effect of social support and health education on depression scale scores of chronic stroke patients. Medicine (Baltimore). 2019;98(44):e17667. https://doi.org/10.1097/md.0000000000017667.
Liu JJ, Dalton AN, Lee J. The “Self” under COVID-19: Social role disruptions, self-authenticity and present-focused co**. PLoS One. 2021;16(9):e0256939. https://doi.org/10.1371/journal.pone.0256939.
Liu Y, Aungsuroch Y, Gunawan J, Zeng D. Job stress, psychological capital, perceived social support, and occupational burnout among hospital nurses. J Nurs Scholarsh. 2021;53(4):511–8. https://doi.org/10.1111/jnu.12642.
Lobato RM, García-Coll J, Moyano M. Disconnected out of passion: relationship between social alienation and obsessive passion. J Interpers Violence. 2022. https://doi.org/10.1177/08862605221094631.
Lv G, Zhao X, Xu X, Hou F, Li P. Gender-based differences in the relationships among social support, positive psychological capital, and sleep quality in patients implanted with pacemakers: a moderated mediation model. J Cardiovasc Nurs. 2022;37(1):79–85. https://doi.org/10.1097/jcn.0000000000000745.
Massar K, Kopplin N, Schelleman-Offermans K. Childhood socioeconomic position, adult educational attainment and health behaviors: the role of psychological capital and health literacy. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18179399.
Mattila E, Peltokoski J, Neva MH, Kaunonen M, Helminen M, Parkkila AK. COVID-19: anxiety among hospital staff and associated factors. Ann Med. 2021;53(1):237–46. https://doi.org/10.1080/07853890.2020.1862905.
Mellin-Olsen J, Staender S. The Helsinki declaration on patient safety in anaesthesiology: the past, present and future. Curr Opin Anaesthesiol. 2014;27(6):630–4. https://doi.org/10.1097/aco.0000000000000131.
Missel M, Bernild C, Westh Christensen S, Dagyaran I, Kikkenborg Berg S. The marked body - a qualitative study on survivors embodied experiences of a COVID-19 illness trajectory. Scand J Caring Sci. 2022;36(1):183–91. https://doi.org/10.1111/scs.12975.
Morin CM, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, Espie CA. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. https://doi.org/10.1016/j.sleep.2021.07.035.
Peng C, Xue K, Tian Y, Zhang X, **g X, Luo H. Organizational emotional capability perspective: research on the impact of psychological capital on enterprise safety performance. Front Psychol. 2022;13:854620. https://doi.org/10.3389/fpsyg.2022.854620.
Rehman SU, Rehman SU, Yoo HH. COVID-19 challenges and its therapeutics. Biomed Pharmacother. 2021;142:112015. https://doi.org/10.1016/j.biopha.2021.112015.
Sabot DL, Hicks RE. Does psychological capital mediate the impact of dysfunctional sleep beliefs on well-being? Heliyon. 2020;6(6):e04314. https://doi.org/10.1016/j.heliyon.2020.e04314.
Saud M, Ashfaq A, Abbas A, Ariadi S, Mahmood QK. Social support through religion and psychological well-being: COVID-19 and co** strategies in Indonesia. J Relig Health. 2021;60(5):3309–25. https://doi.org/10.1007/s10943-021-01327-1.
Shao R, He P, Ling B, Tan L, Xu L, Hou Y, Yang Y. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and co** styles among Chinese medical students. BMC Psychol. 2020;8(1):38. https://doi.org/10.1186/s40359-020-00402-8.
Shayestefar M, Memari AH, Nakhostin-Ansari A, Joghataei MT. COVID-19 and fear, which comes first? Psychiatr Danub. 2021;33(Suppl 13):335–40.
Siu OL, Kong Q, Ng TK. Psychological capital and family satisfaction among employees: do occupational stressors moderate the relationship? Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182212260.
Tang JJ. Psychological capital and entrepreneurship sustainability. Front Psychol. 2020;11:866. https://doi.org/10.3389/fpsyg.2020.00866.
Testoni I, Brondolo E, Ronconi L, Petrini F, Navalesi P, Antonellini M, Capozza D. Burnout following moral injury and dehumanization: a study of distress among Italian medical staff during the first COVID-19 pandemic period. Psychol Trauma. 2022. https://doi.org/10.1037/tra0001346.
Tizenberg BN, Brenner LA, Lowry CA, Okusaga OO, Benavides DR, Hoisington AJ, Postolache TT. Biological and psychological factors determining neuropsychiatric outcomes in COVID-19. Curr Psychiatry Rep. 2021;23(10):68. https://doi.org/10.1007/s11920-021-01275-3.
Twardowska-Staszek E, Rostek I, Biel K, Seredyńska A. Predictors of positive and negative emotions experienced by poles during the second wave of the COVID-19 Pandemic. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182211993.
Wang R, Zhou H, Wang L. The influence of psychological capital and social capital on the entrepreneurial performance of the new generation of entrepreneurs. Front Psychol. 2022;13:832682. https://doi.org/10.3389/fpsyg.2022.832682.
Woday Tadesse A, Mihret ST, Biset G, Kassa AM. Psychological problems and the associated factors related to the COVID-19 pandemic lockdown among college students in Amhara Region, Ethiopia: a cross-sectional study. BMJ Open. 2021;11(9):e045623. https://doi.org/10.1136/bmjopen-2020-045623.
**ao, H., Zhang, Y., Kong, D., Li, S., Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (covid-19) in January and February 2020 in china. Med Sci Monit, 26, e923549. https://doi.org/10.12659/msm.923549
Yan D, Wen F, Li X, Zhang Y. The relationship between psychological capital and innovation behaviour in Chinese nurses. J Nurs Manag. 2020;28(3):471–9. https://doi.org/10.1111/jonm.12926.
Yarcheski A, Mahon NE. Meta-analyses of predictors of hope in adolescents. West J Nurs Res. 2016;38(3):345–68. https://doi.org/10.1177/0193945914559545.
Yu J, Bang KS. Perceived alienation of, and social support for, siblings of children with cancer. J Pediatr Oncol Nurs. 2015;32(6):410–6. https://doi.org/10.1177/1043454214563753.
Yu X, Zhang L, Lin Z, Zhou Z, Hazer-Rau D, Li P, Wu T. Ostracism, psychological capital, perceived social support and depression among economically disadvantaged youths: a moderated mediation model. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182111282.
Zhang F, Liu Y, Wei T. Psychological capital and job satisfaction among Chinese residents: a moderated mediation of organizational identification and income level. Front Psychol. 2021;12:719230. https://doi.org/10.3389/fpsyg.2021.719230.
Zhang JY, Shu T, **ang M, Feng ZC. Learning burnout: evaluating the role of social support in medical students. Front Psychol. 2021;12:625506. https://doi.org/10.3389/fpsyg.2021.625506.
Zhang L, Li W, Liu B, **e W. Self-esteem as mediator and moderator of the relationship between stigma perception and social alienation of Chinese adults with disability. Disabil Health J. 2014;7(1):119–23. https://doi.org/10.1016/j.dhjo.2013.07.004.
Zhou F, Tao M, Shang L, Liu Y, Pan G, ** Y, Yang S. Assessment of sequelae of COVID-19 nearly 1 year after diagnosis. Front Med (Lausanne). 2021;8:717194. https://doi.org/10.3389/fmed.2021.717194.
Zhu JL, Schülke R, Vatansever D, ** D, Yan J, Zhao H, Wang S. Mindfulness practice for protecting mental health during the COVID-19 pandemic. Transl Psychiatry. 2021;11(1):329. https://doi.org/10.1038/s41398-021-01459-8.
Zhu Y, Zhang L, Zhou X, Li C, Yang D. The impact of social distancing during COVID-19: a conditional process model of negative emotions, alienation, affective disorders, and post-traumatic stress disorder. J Affect Disord. 2021;281:131–7. https://doi.org/10.1016/j.jad.2020.12.004.
Acknowledgements
We sincerely thank the head nurses of the shelter hospital for distributing the questionnaire to the participants, and the 259 COVID-19 patients participated in our investigation.
Funding
None.
Author information
Authors and Affiliations
Contributions
Design of the study (CW, CYH, JRY); acquisition of data (HLZ, LL, CT); analysis and reporting of data (NNC, YHZ); drafting the manuscript (QYW, HJL). All the author have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study was conducted under ethical guidelines in the Helsinki Declaration. Research was approved by the ethics committee of ****g Hospital of Air Force Military Medical University, China (Number KY20224143-1). Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, C., He, Cy., Yan, Jr. et al. Psychological capital and alienation among patients with COVID-19 infection: the mediating role of social support. Virol J 20, 114 (2023). https://doi.org/10.1186/s12985-023-02055-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-023-02055-6