Abstract
Purpose
To evaluate viral loads in children with human adenovirus (HAdV) pneumonia at different stages of disease and compare the viral load between upper and lower respiratory tract samples.
Methods
We prospectively enrolled children who required invasive ventilation for HAdV pneumonia. Nasopharyngeal aspirate (NPA) and tracheal aspirate (TA) samples were collected throughout the entire period of invasive ventilation. Viral detection and quantification were performed using quantitative real-time polymerase chain reaction.
Results
Ninety-four children were enrolled. The median age of the children was 12.0 months (IQR: 11.0–24.0), and > ninety percent of patients were aged between 6 and 59 months. Seven hundred and nine paired NPA-TA samples were collected. The median viral loads of the NPA and TA samples were 7.31 log10 and 7.50 log10 copies/mL, respectively. Viral loads generally decreased steadily over time. The median viral load after 1, 2, 3, and > 3 weeks of the disease course was 8.65, 7.70, 6.69, and 5.09 log10 copies/mL, respectively, in NPA samples and 8.67, 7.79, 7.08, and 5.53 log10 copies/mL, respectively, in TA samples. Viral load showed a significant negative correlation with time since symptom onset in both NPA samples (Spearman r = − 0.607, P = 0.000) and TA samples (Spearman r = − 0.544, P = 0.000). The predicted duration of HAdV shedding was 60.17 days in the NPA group and 65.81 days in the TA group. Viral loads in NPA and TA from the same subjects correlated well with each other (R2 = 0.694). HAdV loads in NPA and TA were most comparable during the early phase of infection (95% limits of agreement, − 1.36 to 1.30 log10 copies/mL, R2 = 0.746). Variation increased during the late phase of infection (i.e., in follow-up samples), with viral loads remaining significantly higher in TA than NPA.
Conclusions
In children with HAdV pneumonia, viral loads in both NPA and TA steadily decreased during the course of the disease, and the predicted duration of viral shedding was more than 2 months. The HAdV DNA load of NPA is highly correlated with that of TA, especially in the initial phase of infection.
Similar content being viewed by others
Background
Human adenoviruses (HAdVs) are important pathogens in paediatric pneumonia [1, 2]. Although the prevalence of adenovirus-associated pneumonia (10–20%) is lower than that of respiratory syncytial virus, this type of infection can induce severe and fatal necrotizing pneumonia (especially HAdV-3 and 7) [3,4,5,6,Laboratory experiments Magnetic beads (Multi-Type Sample DNA/RNA Extraction-Purification Kit; Sansure Biotech Inc., Changsha, China) were used to extract DNA from 200 μL of NPA and TA samples following the protocol of the manufacturer. The extracted DNA was eluted in 50 μL of elution buffer and the eluted solution was stored at − 80 °C until required. The hexon gene of HAdV was amplified by quantitative real-time PCR (SLAN 96S Real-Time PCR System, Shanghai Hongshi Medical Technology Co. Ltd., Shanghai, China) using a Respiratory Adenovirus DNA Diagnostic Kit (Sansure Biotech Inc., Changsha, China) according to the manufacturer’s instructions. The PCR reaction comprised 43 μL of a buffer, 2 μL of Taq enzyme (5 U), 0.2 μL each of four primers (50 M), 0.2 μL each of two probes (50 M), and 5 μL of DNA. The kit also contained plasmid DNA of a defined HAdV copy number as a standard. The target-sequence copy number was inversely proportional to the cycle threshold. For positive samples, adjusted Ct values were calculated by correcting the Ct values for the initial sample dilution, and the corrected Ct values were converted to copies/mL using standard curves. An HAdV DNA load of < 1 × 102 copies/mL was considered negative. Glyceraldehyde 3-phosphate dehydrogenase was used as the internal control. Intrasample variation was assessed by dividing material from 10 NPA samples and 10 TA samples into three aliquots, followed by DNA isolation and real-time PCR separately for each aliquot. The precision test showed excellent within -NPA and -TA reproducibility; the coefficient of variation of the detection result Ct value was ≤ 5%. According to Lu and Erdman, the hypervariable region (1–6) of loop 1 of the hexon protein was sequenced for HAdV ty** [23]. Statistical tests were performed using R software (version 3.6.2; R Development Core Team, Vienna, Austria). A P value of < 0.05 was considered indicative of significance. The quantitative PCR data were log10 transformed. Median values are reported with interquartile range (IQR). Statistical comparisons between the NPA and TA groups were evaluated by two-tailed paired Mann–Whitney U tests. Correlations were assessed by two-tailed Spearman test. Scatter plots and Bland–Altman plots with 95% limits of agreement were constructed.Statistical analysis
Results
Patients and general information
A total of 105 patients were enrolled. Eleven patients were excluded, including four with an HAdV DNA load < 1 × 102 copies/mL in TA samples for 4 consecutive days after invasive ventilation (6.34 × 102, 2.59 × 102, 1.31 × 102, and 2.05 × 102 copies/mL, respectively, in initial NPA testing); one with < 3 days of invasive ventilation (deceased); two whose guardians refused continued sampling; and four with an unknown HAdV type. Thus, 94 patients were enrolled in the study (Fig. 1) and provided 736 simultaneously obtained paired NPA-TA samples. Twenty-seven pairs of NPA-TA samples were excluded. Thus, 709 pairs of positive samples were included in the study.
Flow-chart of patient enrolment. a: One patient had undergone invasive ventilation for less than 3 days (patient deceased); four patients were unsuccessfully typed; and two children's guardians refused to provide paired TA specimens. Four patients had positive NPA samples, but four consecutive negative TA samples. b: Among specimens from 94 patients, phylogenetic analysis classified 78 as HAdV-7, 12 as HAdV-3, 2 as HAdV-2, 1 as HAdV-4, and 1 as HAdV-14. c: Reasons for samples included patients being unsuitable for sampling due to a critical condition, insufficient mucus in the nasopharynx or trachea, and sample not collected. d: Twenty-seven pairs of NPA-TA samples were excluded, including eight that were both negative and nineteen that consisted of a positive and negative sample (positive sample viral load range: 2.64–8.67 log10 copies/mL; median = 5.07 log10 copies/mL). In 12 of the latter 19 sample pairs, the TA sample was positive, and the NPA sample was negative. The paired samples collected before and after each of the 27 excluded paired samples were positive for HAdV DNA, indicating that the negative results were due to experimental error. Abbreviations: N, number of patients; n, number of samples; NPA, nasopharyngeal aspirate; TA, tracheal aspirate
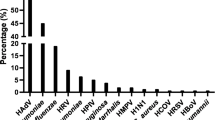
Of the 94 children studied, the ratio of boys to girls was 2.13:1. Male preponderance was most prominent with regard to infection with HAdV. The median age of the children was 12.0 months (IQR: 11.0–24.0), and > 90% of patients were aged between 6 and 59 months. The common genotypes in 94 cases were HAdV-7 (78/94, 82.98%) and HAdV-3 (12/94, 12.77%). Among 94 HAdV-infected patients, 72 were infected with HAdV alone and 22 (23.40%) had coinfections. Four patients were positive for both HAdV and parainfluenza 3, and one patient was positive for HAdV and influenza A. Three children were infected with HAdV, parainfluenza 3, and Mycoplasma pneumoniae. Fourteen children were infected with HAdV and M. pneumoniae. The median interval from onset to hospitalization was 6 days (IQR, 4.00–8.25). All patients had fever and cough (rectal temperature ≥ 38 °C or axillary temperature ≥ 37.5 °C). The median peak temperature was 39.8 °C, and the median duration of fever was 18 days. Together with fever and cough, wheezing (32.98%) was a common respiratory symptom. Gastrointestinal symptoms included diarrhoea (8 [8.51%]) and vomiting (10 [10.64%]). The median duration of mechanical ventilation and length of stay in the PICU were 10 and 17.0 days, respectively. We used a Kaplan–Meier plot to assess the cohort size over time as patients were extubated (Fig. 2). All patients received glucocorticoids and gamma-globulin therapy, and none received antiviral treatment. All five children who died were infected with HAdV-7, and one patient had underlying diseases (Table 1).
There were 19 cases of coinfection in the children in the HAdV-7-infected group and 3 cases in the other HAdV-type-infected group. The age distribution and clinical symptoms were generally similar among the groups (Table 1). Compared with children infected with other HAdV types, those with HAdV-7 had longer duration of fever and mechanical ventilation and longer stays in the PICU and hospital. All of the deaths occurred in type-7 infections. After excluding the influence of coinfection, patients infected by HAdV-7 alone had a longer interval from onset to intubation, longer duration of fever, and longer length of stay in the PICU and hospitals than patients infected by the other HAdV-type alone. However, there was no difference in the duration of mechanical ventilation between the two groups.
Correlation of viral load between TA and NPA samples
We studied 709 pairs of respiratory samples collected from 94 individuals at different stages of infection. The viral loads ranged from 2.37 to 11.08 log10 copies/mL; the median values for the NPA and TA samples were 7.31 log10 and 7.50 log10 copies/mL, respectively. The median viral loads after 1, 2, 3 and > 3 weeks of the disease course was 8.65, 7.70, 6.69, and 5.09 log10 copies/mL, respectively, in NPA samples and 8.67, 7.79, 7.08, and 5.53 log10 copies/mL, respectively, in TA samples. Viral load was significantly higher in TA than NPA samples (Wilcoxon, Z = − 2.281, P = 0.023).
We monitored the kinetics of HAdV viral loads in upper and lower respiratory specimens from 94 patients. We analysed 709 NPA (Fig. 3A) and 709 TA (Fig. 3B) samples; there were > 3 sequential paired samples for each patient. There was a significant negative correlation between viral load and time since onset in both NPA samples (Spearman r = − 0.607, P = 0.000) and TA samples (Spearman r = − 0.544, P = 0.000). The viral load reduction rate and predicted duration of shedding were − 0.157 log10 copies/mL per day (95% confidence interval [CI]: − 0.143 to − 0.171; R2 = 0.397) and 60.17 days (y = 9.447 − 0.157x), respectively, for NPA and − 0.144 log10 copies/mL per day (95% CI: − 0.13 to − 0.158; R2 = 0.368) and 65.81 days (y = 9.476 − 0.144x), respectively, for TA. Pre-extubation viral loads (i.e., the last paired samples for each patient) were also similar in the same patients. The median viral loads of NPA and TA were 5.55 log10 copies/mL (IQR: 5.01–5.95) and 5.74 log10 copies/mL (IQR: 5.06–6.37), respectively. Furthermore, all patients remained virus-positive in the invasive ventilation stages of infection. Severe cases had prolonged viral shedding in respiratory secretions, i.e., viral DNA was still detected in five patients > 30 days after the onset of symptoms.
We further plotted viral loads (median [IQR]) for NPA and TA samples collected from 94 patients at different disease stages. There was no significant difference in viral loads between NPA and TA samples at days 6–13 after onset, but variation increased during the late phase of infection (days 14, 16, 18, 21, 23, and 24), with loads remaining significantly higher in TA than NPA samples (Fig. 4). The viral loads were significantly correlated between NPA and TA samples (R2 = 0.694, P = 0.000) (Fig. 5). Cooccurring viral loads from NPA and TA samples of the same subjects also correlated well with each other. Viral loads of TA and NPA samples from the 321 pairs available from days 6–13 correlated significantly (R2 = 0.746, P = 0.000) (Fig. 4). The 95% limits of agreement for paired samples from days 6–13 were − 1.36 and 1.30 log10 copies/mL (Fig. 6).
Viral loads (median [IQR]) in NPA and TA samples collected from 94 patients at days 3–30 after disease onset. The data after day 30 of onset were not due to small numbers of paired samples. Continuous data for > 10 paired samples were analysed by 2-tailed paired Mann–Whitney U tests. All P values indicate significant differences. Abbreviations: n, number of pairs of samples; NPA, nasopharyngeal aspirate; TA, tracheal aspirate
Correlation of viral loads between NPA samples and TA samples. Solid line represents linear correlation. A Viral loads of 709 pairs of NPA-TA samples over the course of the disease (R2 = 0.694, P = 0.000). B Viral loads of 321 pairs of NPA-TA samples 6–13 days after disease onset (R2 = 0.746, P = 0.000). Abbreviations: n, number of pairs of samples; NPA, nasopharyngeal aspirate; TA, tracheal aspirate
Discussion
We found that fever and cough were common clinical presentations in 94 mechanically ventilated children (median age = 12 months) with HAdV pneumonia. HAdV-7 was the main infection genotype, and all of the deaths were in HAdV-7-infected patients. We observed that HAdV-7 infection has a worse outcome than other HAdV types of infection, as others have reported [5, 19]. An aetiological study of Australian children with lower respiratory tract infection used PCR to show that HAdV positivity in nasopharyngeal swabs was associated with lower respiratory tract infection [20]. NPA samples can be acquired less invasively and used to monitor viral shedding trends. The present study showed that for children with HAdV pneumonia, the viral loads in NPA and TA samples were significantly correlated, especially at days 6–13 of the disease course. We recommend that patients be sampled, including collecting NPA, as early as possible during the course of infection to obtain the most reliable measure of HAdV.
We found that the variation in viral loads increased during the late phase of infection, with loads being significantly higher in TA than NPA samples. Previous studies have shown that virus replication and inflammatory responses differ among various parts of the airways and lungs [35, 36]. Therefore, the difference in viral loads between TA and NPA samples during the late phase of infection may be related to the pathogenesis of adenoviral pneumonia.
We also found that the pre-extubation viral loads (i.e., the last paired samples for each patient) were similar among all patients. To improve prognosis and disease management, the association between viral loads and ventilator weaning should be assessed in a randomized controlled trial with a process evaluation (such as by an ethics committee).
Our study had several limitations. First, it was a single-centre cohort study, and we did not enrol patients with early-stage or mild HAdV pneumonia or those who did not require invasive ventilation or were asymptomatically healthy; this was due to ethical considerations. Thus, there is some uncertainty as to whether our results can be extended to mild HAdV pneumonia. Additionally, viral loads are influenced by many factors. Although the samples in this study were collected by experienced nurses and sent for testing by specialized laboratory staff, confounding human factors may still have affected the sampling process. Viral shedding was also affected by factors such as genotype and therapy (data not shown). Furthermore, viral cultures from the collected samples were not seeded. PCR has high sensitivity, is easy to perform, and is widely used to detect viral loads. In our patients, continuous monitoring of HAdV load was not consistent with transient shedding during latent infection or transient shedding of residual virus. Finally, although multiple respiratory tract samples were collected from each patient for virus testing, we did not determine the precise timing of the “turning point” (i.e., from positive to negative virus detection).
Conclusions
In conclusion, viral loads in both NPA and TA steadily decreased with the course of the disease, and the duration of HAdV shedding in respiratory specimens was long. The HAdV DNA load of NPA is highly correlated with that of TA, especially in the initial phase of infection.
Availability of data and materials
The datasets of the current study are available from the corresponding author on reasonable request.
Abbreviations
- HAdV:
-
Human adenovirus
- NPA:
-
Nasopharyngeal aspirates
- TA:
-
Tracheal aspirates
- PICU:
-
Pediatric intensive care unit
- IQR:
-
Interquartile ranges
- CI:
-
Confidence interval
References
Li QG, Zheng QJ, Liu YH, Wadell G. Molecular epidemiology of adenovirus types 3 and 7 isolated from children with pneumonia in Bei**g. J Med Virol. 1996;49(3):170–7.
Ruuskanen O, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011;377(9773):1264–75.
Carballal G, Videla C, Misirlian A, Requeijo PV, Aguilar MC. Adenovirus type 7 associated with severe and fatal acute lower respiratory infections in Argentine children. BMC Pediatr. 2002;2:6.
García-García ML, Calvo C, Pozo F, Villadangos PA, Pérez-Breña P, Casas I. Spectrum of respiratory viruses in children with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(8):808–13.
Hong JY, Lee HJ, Piedra PA, Choi EH, Park KH, Koh YY, et al. Lower respiratory tract infections due to adenovirus in hospitalized Korean children: epidemiology, clinical features, and prognosis. Clin Infect Dis. 2001;32(10):1423–9.
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835–45.
**e L, Zhang B, Zhou J, Huang H, Zeng S, Liu Q, et al. Human adenovirus load in respiratory tract secretions are predictors for disease severity in children with human adenovirus pneumonia. Virol J. 2018;15(1):123.
Franz A, Adams O, Willems R, Bonzel L, Neuhausen N, Schweizer-Krantz S, et al. Correlation of viral load of respiratory pathogens and co-infections with disease severity in children hospitalized for lower respiratory tract infection. J Clin Virol. 2010;48(4):239–45.
Gray GC, McCarthy T, Lebeck MG, Schnurr DP, Russell KL, Kajon AE, et al. Genotype prevalence and risk factors for severe clinical adenovirus infection, United States 2004–2006. Clin Infect Dis. 2007;45(9):1120–31.
Palomino MA, Larranaga C, Villagra E, Camacho J, Avendano LF. Adenovirus and respiratory syncytial virus-adenovirus mixed acute lower respiratory infections in Chilean infants. Pediatr Infect Dis J. 2004;23(4):337–41.
Goikhman Y, Drori Y, Friedman N, Sherbany H, Keller N, Mendelson E, et al. Adenovirus load correlates with respiratory disease severity among hospitalized pediatric patients. Int J Infect Dis. 2020;97:145–50.
Suparno C, Milligan DW, Moss PA, Mautner V. Adenovirus infections in stem cell transplant recipients: recent developments in understanding of pathogenesis, diagnosis and management. Leuk Lymphoma. 2004;45(5):873–85.
Hammitt LL, Feikin DR, Scott JAG, Zeger SL, Murdoch DR, O’Brien KL, et al. Addressing the analytic challenges of cross-sectional pediatric pneumonia etiology data. Clin Infect Dis. 2017;64(suppl_3):S197–204.
Feikin DR, Hammitt LL, Murdoch DR, O’Brien KL, Scott JAG. The enduring challenge of determining pneumonia etiology in children: considerations for future research priorities. Clin Infect Dis. 2017;64(suppl_3):S188–96.
Hammitt LL, Murdoch DR, Scott JA, Driscoll A, Karron RA, Levine OS, et al. Specimen collection for the diagnosis of pediatric pneumonia. Clin Infect Dis. 2012;54(Suppl 2):S132–9.
Kalu SU, Loeffelholz M, Beck E, Patel JA, Revai K, Fan J, et al. Persistence of adenovirus nucleic acids in nasopharyngeal secretions: a diagnostic conundrum. Pediatr Infect Dis J. 2010;29(8):746–50.
Rhedin S, Lindstrand A, Rotzen-Ostlund M, Tolfvenstam T, Ohrmalm L, Rinder MR, et al. Clinical utility of PCR for common viruses in acute respiratory illness. Pediatrics. 2014;133(3):e538–45.
Garnett CT, Talekar G, Mahr JA, Huang W, Zhang Y, Ornelles DA, et al. Latent species C adenoviruses in human tonsil tissues. J Virol. 2009;83(6):2417–28.
Lu AZ, Shi P, Wang LB, Qian LL, Zhang XB. Diagnostic value of nasopharyngeal aspirates in children with lower respiratory tract infections. Chin Med J (Engl). 2017;130(6):647–51.
Smith-Vaughan HC, Binks MJ, Beissbarth J, Chang AB, McCallum GB, Mackay IM, et al. Bacteria and viruses in the nasopharynx immediately prior to onset of acute lower respiratory infections in Indigenous Australian children. Eur J Clin Microbiol Infect Dis. 2018;37(9):1785–94.
Subspecialty Group of Respiratory Diseases, The Society of Pediatrics, Chinese Medical Association; Editorial Board, Chinese Journal of Pediatrics. Guidelines for management of community acquired pneumonia in children (the revised edition of 2013) (I). Zhonghua Er Ke Za Zhi. 2013;51(10):745–52.
Driscoll AJ, Karron RA, Morpeth SC, Bhat N, Levine OS, Baggett HC, et al. Standardization of laboratory methods for the PERCH study. Clin Infect Dis. 2017;64(suppl_3):S245–52.
Lu X, Erdman DD. Molecular ty** of human adenoviruses by PCR and sequencing of a partial region of the hexon gene. Arch Virol. 2006;151(8):1587–602.
Fu Y, Tang Z, Ye Z, Mo S, Tian X, Ni K, et al. Human adenovirus type 7 infection causes a more severe disease than type 3. BMC Infect Dis. 2019;19(1):36.
Liu C, **ao Y, Zhang J, Ren L, Li J, **e Z, et al. Adenovirus infection in children with acute lower respiratory tract infections in Bei**g, China, 2007 to 2012. BMC Infect Dis. 2015;15:408.
Yu Z, Zeng Z, Zhang J, Pan Y, Chen M, Guo Y, et al. Fatal community-acquired pneumonia in children caused by re-emergent human adenovirus 7d associated with higher severity of illness and fatality rate. Sci Rep. 2016;6:37216.
Jiang W, Wu M, Zhou J, Wang Y, Hao C, Ji W, et al. Etiologic spectrum and occurrence of coinfections in children hospitalized with community-acquired pneumonia. BMC Infect Dis. 2017;17(1):787.
Nguyen T, Kyle UG, Jaimon N, Tcharmtchi MH, Coss-Bu JA, Lam F, et al. Coinfection with Staphylococcus aureus increases risk of severe coagulopathy in critically ill children with influenza A (H1N1) virus infection. Crit Care Med. 2012;40(12):3246–50.
Dawood FS, Chaves SS, Pérez A, Reingold A, Meek J, Farley MM, et al. Complications and associated bacterial coinfections among children hospitalized with seasonal or pandemic influenza, United States, 2003–2010. J Infect Dis. 2014;209(5):686–94.
Choi SH, Hong SB, Ko GB, Lee Y, Park HJ, Park SY, et al. Viral infection in patients with severe pneumonia requiring intensive care unit admission. Am J Respir Crit Care Med. 2012;186(4):325–32.
Nolan VG, Arnold SR, Bramley AM, Ampofo K, Williams DJ, Grijalva CG, et al. Etiology and impact of coinfections in children hospitalized with community-acquired pneumonia. J Infect Dis. 2018;218(2):179–88.
Huh K, Kim I, Jung J, Lee JE, Jhun BW, Gu SH, et al. Prolonged shedding of type 55 human adenovirus in immunocompetent adults with adenoviral respiratory infections. Eur J Clin Microbiol Infect Dis. 2019;38(4):793–800.
Ganime AC, Carvalho-Costa FA, Santos M, Costa Filho R, Leite JP, Miagostovich MP. Viability of human adenovirus from hospital fomites. J Med Virol. 2014;86(12):2065–9.
Gu L, Qu J, Sun B, Yu X, Li H, Cao B. Sustained viremia and high viral load in respiratory tract secretions are predictors for death in immunocompetent adults with adenovirus pneumonia. PLoS ONE. 2016;11(8):e0160777.
Yang TI, Li WL, Chang TH, Lu CY, Chen JM, Lee PI, et al. Adenovirus replication and host innate response in primary human airway epithelial cells. J Microbiol Immunol Infect. 2019;52(2):207–14.
Becroft DM. Histopathology of fatal adenovirus infection of the respiratory tract in young children. J Clin Pathol. 1967;20(4):561–9.
Acknowledgements
All authors wish to thank the infants and their parents, who volunteered to participate in this study.
Funding
This work was supported by Hunan Provincial Medicine and Health Research Program (Grant No. B201611) and China Mega-Project for Infectious Disease (Grant No. 2014ZX10004002).
Author information
Authors and Affiliations
Contributions
BZ and SZ were responsible for the study concept and design. XH, TW, LY, and JL collected study samples and acquired the data. LX, SZ, TY, and LZ analyzed and interpreted the data. LX, SZ, ZD, and BZ have drafted the manuscript and critically revised it for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University).
Consent for publication
Not applicable.
Competing interests
No authors have any potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
**e, LY., Zeng, SZ., Yu, T. et al. Viral loads in nasopharyngeal aspirates and tracheal aspirates among children hospitalized with invasive ventilation for human adenovirus pneumonia. Virol J 18, 238 (2021). https://doi.org/10.1186/s12985-021-01711-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-021-01711-z