Abstract
Background
The triglyceride-glucose (TyG) index and triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio, two simple surrogate indicators of insulin resistance, have been demonstrated to predict cardiovascular disease (CVD). However, very few studies have investigated their associations with CVD in European populations.
Methods
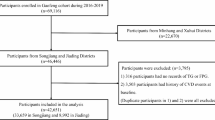
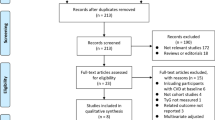
A total of 403,335 participants from the UK Biobank with data for TyG index and TG/HDL-C ratio and free from CVD at baseline were included. Cox models were applied to evaluate the association between TyG index and TG/HDL-C ratio and incident CVD. Mediation analyses were performed to evaluate the contribution of prevalent diabetes, hypertension, and dyslipidemia to observed associations.
Results
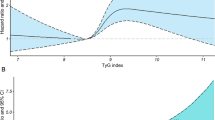
During a median follow-up of 8.1 years, 19,754 (4.9%) individuals developed CVD, including 16,404 (4.1%) cases of CHD and 3976 (1.0%) cases of stroke. The multivariable-adjusted hazard ratios of total CVD in higher quartiles versus the lowest quartiles were 1.05, 1.05, and 1.19, respectively, for TyG index, and 1.07, 1.13, and 1.29, respectively, for TG/HDL-C ratio. There were significant trends toward an increasing risk of CVD across the quartiles of TyG index and TG/HDL-C ratio. In mediation analyses, dyslipidemia, type 2 diabetes, and hypertension explained 45.8%, 27.0%, and 15.0% of TyG index’s association with CVD, respectively, and 40.0%, 11.8%, and 13.3% of TG/HDL-C ratio’s association with CVD, respectively.
Conclusions
Elevated baseline TyG index and TG/HDL-C ratio were associated with a higher risk of CVD after adjustment for the well-established CVD risk factors. These associations were largely mediated by greater prevalence of dyslipidemia, type 2 diabetes, and hypertension.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD), including ischemic heart disease and stroke, constitute the leading cause of premature death worldwide [1]. In 2017, CVD caused an estimated 17.8 million deaths and was responsible for 330 million years of life lost globally [1]. This highlights the importance of identifying risk factors that could predict the risk of CVD and thereby facilitate its prevention at an early stage.
Insulin resistance, a pathophysiological condition characterized by the decreased insulin sensitivity of peripheral tissues, plays a key role in the development of metabolic syndrome and atherosclerosis [2, 3]. The euglycemic-hyperinsulinemic clamp is served as the gold standard to identify insulin resistance, but the technique is laborious, costly, and therefore impractical in the clinical setting [4]. The triglyceride-glucose (TyG) index and triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio have been proposed as simple and credible surrogate indicators of insulin resistance because they show strong correlations with the euglycemic-hyperinsulinemic clamp and they are suitable for clinical practice and large epidemiological studies [5, 6]. Several cross-sectional and retrospective studies have reported significant associations of the TyG index and TG/HDL-C ratio with incident CVD [14]. Furthermore, another 8-year prospective study of 796 participants showed that an elevated TG/HDL-C ratio predicted the incident risk of CVD events [21]. Consistent with prior studies, our study of a larger sample size confirmed that higher TyG index and TG/HDL-C ratio were significantly associated with increased risks of total CVD and CHD in the UK Biobank population. Neither the TyG index nor TG/HDL-C ratio was associated with stroke in our population after full covariate adjustment, in contrast with some earlier studies [39].
In conclusion, our analysis of data from the UK Biobank showed that elevated baseline TyG index and TG/HDL-C ratio, two surrogate markers of insulin resistance, were associated with a higher risk of CVD after adjustment for the well-established CVD risk factors. These associations were largely mediated by the greater prevalence of dyslipidemia, diabetes, and hypertension.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the public UK Biobank Resource (www.ukbiobank.ac.uk/).
References
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88.
Faerch K, Vaag A, Holst JJ, Hansen T, Jørgensen T, Borch-Johnsen K. Natural history of insulin sensitivity and insulin secretion in the progression from normal glucose tolerance to impaired fasting glycemia and impaired glucose tolerance: the Inter99 study. Diabetes Care. 2009;32(3):439–44.
Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14(5):575–85.
Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23(1):57–63.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, Jacques-Camarena O, Rodríguez-Morán M. The product of triglycerides and glucose, a simple measure of insulin sensitivity comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51.
Giannini C, Santoro N, Caprio S, Kim G, Lartaud D, Shaw M, Pierpont B, Weiss R. The triglyceride-to-HDL cholesterol ratio: association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care. 2011;34(8):1869–74.
Shi W, **ng L, **g L, Tian Y, Yan H, Sun Q, Dai D, Shi L, Liu S. Value of triglyceride-glucose index for the estimation of ischemic stroke risk: insights from a general population. Nutr Metab Cardiovasc Dis. 2020;30(2):245–53.
Guo W, Zhu W, Wu J, Li X, Lu J, Qin P, Zhu C, Xu N, Zhang Q. Triglyceride glucose index is associated with arterial stiffness and 10-year cardiovascular disease risk in a chinese population. Front Cardiovascular Med. 2021;8:585776.
Su WY, Chen SC, Huang YT, Huang JC, Wu PY, Hsu WH, Lee MY. Comparison of the effects of fasting glucose, hemoglobin A(1c), and triglyceride-glucose index on cardiovascular events in type 2 diabetes mellitus. Nutrients. 2019. https://doi.org/10.3390/nu11112838.
Li S, Guo B, Chen H, Shi Z, Li Y, Tian Q, Shi S. The role of the triglyceride (triacylglycerol) glucose index in the development of cardiovascular events: a retrospective cohort analysis. Sci Rep. 2019;9(1):7320.
Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med. 2020;18(1):361.
Bertoluci MC, Quadros AS, Sarmento-Leite R, Schaan BD. Insulin resistance and triglyceride/HDLc index are associated with coronary artery disease. Diabetol Metab Syndr. 2010;2:11.
Barzegar N, Tohidi M, Hasheminia M, Azizi F, Hadaegh F. The impact of triglyceride-glucose index on incident cardiovascular events during 16 years of follow-up: tehran lipid and glucose study. Cardiovasc Diabetol. 2020;19(1):155.
Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, Wang A. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20(1):19.
Park B, Lee YJ, Lee HS, Jung DH. The triglyceride-glucose index predicts ischemic heart disease risk in Koreans: a prospective study using national health insurance service data. Cardiovasc Diabetol. 2020;19(1):210.
Lee EY, Yang HK, Lee J, Kang B, Yang Y, Lee SH, Ko SH, Ahn YB, Cha BY, Yoon KH, et al. Triglyceride glucose index, a marker of insulin resistance, is associated with coronary artery stenosis in asymptomatic subjects with type 2 diabetes. Lipids Health Dis. 2016;15(1):155.
Zhao Y, Sun H, Zhang W, ** Y, Shi X, Yang Y, Lu J, Zhang M, Sun L, Hu D. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: the rural Chinese cohort study. Diabetes Metab. 2021;47(4):101246.
Turak O, Afşar B, Ozcan F, Öksüz F, Mendi MA, Yayla Ç, Covic A, Bertelsen N, Kanbay M. The role of plasma triglyceride/high-density lipoprotein cholesterol ratio to predict new cardiovascular events in essential hypertensive patients. J Clin Hypertens (Greenwich). 2016;18(8):772–7.
Sánchez-Íñigo L, Navarro-González D, Fernández-Montero A, Pastrana-Delgado J, Martínez JA. The TyG index may predict the development of cardiovascular events. Eur J Clin Invest. 2016;46(2):189–97.
Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, Dulbecco CA, Reaven GM. Comparison of two surrogate estimates of insulin resistance to predict cardiovascular disease in apparently healthy individuals. Nutr Metab Cardiovasc Dis. 2017;27(4):366–73.
Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, Leiva Sisnieguez CE, March CE, Balbín E, Stavile RN, Reaven GM. Identifying cardiovascular disease risk and outcome: use of the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio versus metabolic syndrome criteria. J Intern Med. 2013;273(6):595–601.
Rader DJ. Effect of insulin resistance, dyslipidemia, and intra-abdominal adiposity on the development of cardiovascular disease and diabetes mellitus. Am J Med. 2007;120(3 Suppl 1):S12-18.
Reaven GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities–the role of insulin resistance and the sympathoadrenal system. N Engl J Med. 1996;334(6):374–81.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Tyrrell J, Jones SE, Beaumont R, Astley CM, Lovell R, Yaghootkar H, Tuke M, Ruth KS, Freathy RM, Hirschhorn JN, et al. Height, body mass index, and socioeconomic status: mendelian randomisation study in UK Biobank. BMJ Clin Res ed. 2016;352:i582.
Elliott P, Peakman TC. The UK Biobank sample handling and storage protocol for the collection, processing and archiving of human blood and urine. Int J Epidemiol. 2008;37(2):234–44.
Fritz J, Bjørge T, Nagel G, Manjer J, Engeland A, Häggström C, Concin H, Teleka S, Tretli S, Gylling B, et al. The triglyceride-glucose index as a measure of insulin resistance and risk of obesity-related cancers. Int J Epidemiol. 2020;49(1):193–204.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100.
Drouin-Chartier JP, Zheng Y, Li Y, Malik V, Pan A, Bhupathiraju SN, Tobias DK, Manson JE, Willett WC, Hu FB. Changes in consumption of sugary beverages and artificially sweetened beverages and subsequent risk of type 2 diabetes: results from three large prospective us cohorts of women and men. Diabetes care. 2019;42(12):2181–9.
Lee H, Herbert RD, McAuley JH. Mediation analysis. JAMA. 2019;321(7):697–8.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Eeg-Olofsson K, Gudbjörnsdottir S, Eliasson B, Zethelius B, Cederholm J. The triglycerides-to-HDL-cholesterol ratio and cardiovascular disease risk in obese patients with type 2 diabetes: an observational study from the Swedish national diabetes register (NDR). Diabetes Res Clin Pract. 2014;106(1):136–44.
Wu Z, Zhou D, Liu Y, Li Z, Wang J, Han Z, Miao X, Liu X, Li X, Wang W, et al. Association of TyG index and TG/HDL-C ratio with arterial stiffness progression in a non-normotensive population. Cardiovasc Diabetol. 2021;20(1):134.
Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev. 2018;98(4):2133–223.
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the vascular-metabolic CUN cohort. Prev Med. 2016;86:99–105.
Wang Y, Yang W, Jiang X. Association between triglyceride-glucose index and hypertension: a meta-analysis. Front Cardiovascular Med. 2021;8:644035.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R, Allen NE. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol. 2017;186(9):1026–34.
Acknowledgements
We thank UK Biobank participants. This research has been conducted using the UK Biobank Resource (Application No 52632).
Funding
The study is supported by grants from by the National Natural Science Foundation of China (Grant 82173648), the Innovative Talent Support Plan of the Medical and Health Technology Project in Zhejiang province (2021422878), the Zhejiang Provincial Public Service and Application Research Foundation (LGF20H250001 and GC22H264267), Ningbo Health Branding Subject Fund (PPXK2018-01), the Internal Fund of Ningbo Institute of Life and Health Industry, University of Chinese Academy of Sciences (2020YJY0212), Ningbo Clinical Research Center for Digestive System Tumors (2019A21003), Key Laboratory of Diagnosis and Treatment of Digestive System Tumors of Zhejiang Province, Ningbo, China (2019E10020), the Public Welfare Foudation of Ningbo (2021S108), and Ningbo Science and Technology Innovation 2025 Specific Project (2020Z096).
Author information
Authors and Affiliations
Contributions
Conceptualization: BC and LH; Methodology: BC and CZ; Formal analysis and investigation: BC and CZ; Writing—original draft preparation: BC; Writing—review and editing: LH and YZ; Funding acquisition: LH; Resources: RZ, LP, and TZ; Supervision: YZ and LH All authors contributed to subsequent revisions and approved the final version. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
UK Biobank was constructed under ethical approval obtained by the North West Multi-Centre Research Ethics Committee (REC reference: 11/NW/03820) and all participants provided written informed consent prior to participation. The current analyses were carried out under Application Number 52632.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Characteristics of the study population according to the TG/HDL-C ratio quartiles. TG/HDL-C, triglyceride to high-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate. aContinuous variables are expressed as mean (SD). Categorical variables are expressed as frequency (percentage). Table S2. Correlations of the TyG index and TG/HDL-C ratio with participant characteristicsa. TyG, triglyceride-glucose; TG/HDL-C, triglyceride to high-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate. aPoint-biserial correlation for dichotomized variables and Pearson’s correlation for continuous variables. Table S3. Characteristics and cardiovascular outcomes of the study population in England, Scotland, and Wales. TyG, triglyceride-glucose; TG/HDL-C, triglyceride to high-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate. aContinuous variables are expressed as mean (SD). Categorical variables are expressed as frequency (percentage). Table S4. Sensitivity analysis: Multivariable-adjusted hazard ratios of cardiovascular disease associated with the TyG index and TG/HDL-C ratio, additionally adjusted for prevalent dyslipidemia, type 2 diabetes, and hypertension. TyG, triglyceride-glucose; TG/HDL-C, triglyceride to high-density lipoprotein cholesterol; HR, hazard ratio. aHazard ratios were adjusted for the variables included in model 3 in Table 2 in addition to prevalent type 2 diabetes, hypertension, and dyslipidemia. Table S5. Sensitivity analysis: Associations of the TyG index and TG/HDL-C ratio with risk of cardiovascular disease, excluding 6080 incident cases with less than 3 years of follow-up (N = 397,255). TyG, triglyceride-glucose; TG/HDL-C, triglyceride to high-density lipoprotein cholesterol; HR, hazard ratio. Hazard ratios were adjusted for the same variables included in model 3 in Table 2. Appendix S1. ICD-10 codes used to ascertain comorbidities and cardiovascular outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Che, B., Zhong, C., Zhang, R. et al. Triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio as potential cardiovascular disease risk factors: an analysis of UK biobank data. Cardiovasc Diabetol 22, 34 (2023). https://doi.org/10.1186/s12933-023-01762-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01762-2