Abstract
Background
Medication non-adherence is a significant problem in patients with Chronic Obstructive Pulmonary Disease (COPD). Efforts to address this issue are receiving increased attention. Simplifying treatment by prescribing single-inhaler triple therapy (SITT) as an alternative to multi-inhaler triple therapy (MITT) or with smart inhalers are often considered potential solutions. However, the actual impact of these innovations on adherence and clinical outcomes is unclear.
Methods
To address this knowledge gap we first conducted a literature review focusing on two research questions: 1) the difference in adherence between SITT and MITT users in COPD, and 2) the effect of smart inhalers on adherence in COPD. Separate searches were conducted in PubMed and two authors independently assessed the articles. In addition, we present a protocol for a study to acquire knowledge for the gaps identified.
Results
To address the first research question, 8 trials were selected for further review. All trials were observational, i.e. randomized controlled trials were lacking. Seven of these trials showed higher adherence and/or persistence in patients on SITT compared with patients on MITT. In addition, four studies showed a positive effect of SITT on various clinical outcomes. For the second research question, 11 trials were selected for review. While most of the studies showed a positive effect of smart inhalers on adherence, there was considerable variation in the results regarding their effect on other clinical outcomes.
The TRICOLON (TRIple therapy COnvenience by the use of one or multipLe Inhalers and digital support in ChrONic Obstructive Pulmonary Disease) trial aims to improve understanding regarding the effectiveness of SITT and smart inhalers in enhancing adherence. This open-label, randomized, multi-center study will enroll COPD patients requiring triple therapy at ten participating hospitals. In total, 300 patients will be randomized into three groups: 1) MITT; 2) SITT; 3) SITT with digital support through a smart inhaler and an e-health platform. The follow-up period will be one year, during which three methods of measuring adherence will be used: smart inhaler data, self-reported data using the Test of Adherence to Inhalers (TAI) questionnaire, and drug analysis in scalp hair samples. Finally, differences in clinical outcomes between the study groups will be compared.
Discussion
Our review suggests promising results concerning the effect of SITT, as opposed to MITT, and smart inhalers on adherence. However, the quality of evidence is limited due to the absence of randomized controlled trials and/or the short duration of follow-up in many studies. Moreover, its impact on clinical outcomes shows considerable variation. The TRICOLON trial aims to provide solid data on these frequently mentioned solutions to non-adherence in COPD. Collecting data in a well-designed randomized controlled trial is challenging, but the design of this trial addresses both the usefulness of SITT and smart inhalers while ensuring minimal interference in participants' daily lives.
Trial registration
NCT05495698 (Clinicaltrials.gov), registered at 08–08-2022. Protocol version: version 5, date 27–02-2023.
Similar content being viewed by others
Introduction
Background
Chronic obstructive pulmonary disease (COPD) is characterized by chronic respiratory symptoms due to abnormalities in the airways and/or alveoli, resulting in persistent and often progressive airflow obstruction. Inhalation medication is the primary medical treatment, with three types of inhalation medication available as maintenance therapy: 1) long-acting β2-agonist (LABA), 2) long-acting muscarinic antagonist (LAMA), and 3) inhaled corticosteroids (ICS). Triple therapy is defined as treatment with LABA, LAMA and ICS [1]. Large randomized controlled trials have shown that triple therapy provides clinical benefits compared to dual therapy in patients with moderate-to-severe COPD and a history of exacerbations, particularly when eosinophilia is present [2,3,4,5,6]. Furthermore, two trials suggest that triple therapy reduces mortality in this specific population [7, 8]. Triple therapy can be administered through multiple devices, known as multi-inhaler-triple therapy (MITT), or combined in one inhaler, known as single-inhaler-triple therapy (SITT). Assessment of adherence to inhalation therapy is a crucial element in managing COPD patients according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [1]. Previous studies have shown that medication adherence is poor in patients with COPD. A systematic review showed that non-adherence rates ranged from 22 to 93%, depending on the study population and method of measurement [9]. Non-adherence is associated with poor clinical and economic outcomes [10, 11]. Simplifying treatment with smart-inhalers and prescribing single-inhaler triple therapy (SITT) as an alternative to multi-inhaler triple therapy (MITT) can be considered as potential solutions. Nowadays, the GOLD report (version 2024) acknowledges that a single inhaler may be more convenient compared to multi-inhaler therapy. [1]. The actual impact of these innovations on adherence is unclear. Therefore, we conducted a literature review to examine the current evidence on these two potential solutions. Should the evidence prove to be insufficient, we wanted to present a protocol for a study to fill this gap.
Methods for measuring adherence
Adherence is defined as the process by which patients take their medication as prescribed, while persistence refers to the duration from initiation to discontinuation of the treatment. Adherence and persistence are complex constructs, as previously described by Vrijens et al. [12, 13]. Various methods can be used to assess medication adherence. Healthcare professionals commonly inquire directly about their patients' adherence. While this approach is straightforward, research has demonstrated its unreliability in comparison to more objective measurement methods. Unstructured self-reports often lead to an overestimation of adherence [14]. Patients can structurally self-report their adherence using questionnaires, such as the Test of Adherence to Inhalers (TAI). The TAI is developed specifically to measure adherence to inhalation medication in patients with COPD or asthma [15]. Furthermore, pharmacy data are often used to determine patient’s access to medication over time by calculating the Proportion of Days Covered (PDC). This method may be less reliable due to missing or inaccessible data (e.g. when multiple pharmacies are used) and the uncertainty about whether the patient actually used the medication [16, 17]. Smart inhalers offer a more objective method for measuring adherence. These electronic sensors (e-devices) are attached to or integrated into inhalers. Devices range from simple dose counters to advanced devices that provide reminders, feedback, and/or analyse inhalation technique [18]. Smart inhalers are often integrated with other e-health interventions, such as telemonitoring, personalised feedback with apps, counselling, and training [19,20,21]. Finally, hair analysis can provide a bioanalytical assessment of average long-term drug exposure in the human body. This method could potentially provide an objective measure of adherence over the last few months. However, external factors can impact measurement, and only small part of medication that has been present in the systemic blood circulation is built into hair [22].
Methods
First, we present a review of the literature on two strategies to improve adherence. Second, we describe the study protocol of the TRICOLON trial (TRIple therapy COnvenience by the use of one or multipLe Inhalers and digital support in ChrONic Obstructive Pulmonary Disease).
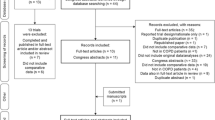
Search strategy literature review
Separate searches were conducted in PubMed based on two research questions: 1) What is the difference in adherence between SITT and MITT users in COPD?, and 2) What is the effect of smart inhalers on adherence in COPD? The selection of articles from the second PubMed search was supplemented by four papers known to the authors or found by snowballing. Two authors independently assessed these articles to determine whether they should be included in this review (LC and JiV). In cases of disagreement, the opinion of a third author was sought (HK). Only original English-language studies were included. Details of the PubMed search and selection process can be found in the Appendix, Suppl.1.
Assessment of the evidence
The primary outcome was the adherence and/or persistence to triple therapy. Secondary outcomes were clinical outcomes, such as exacerbations, COPD Assessment Test (CAT) score, and FEV1. Each study underwent an evaluation across multiple criteria to assess the evidence supporting the research question. The strength of the study design was rated with stars: one star for retrospective studies, two stars for prospective observational studies or intervention studies without randomization (e.g. before-and-after designs), and three stars for randomised controlled trials. A green smiley indicates statistically significant superior results in the intervention group (either SITT or smart-inhaler group, depending on the research question) compared to the control group; a yellow neutral smiley signifies no difference between the groups, while a red sad smiley denotes statistically significant inferior results in the intervention group compared to the control group. Additionally, a thumbs-up signifies that other clinical outcomes were measured in that study, whereas a thumbs-down indicates the absence of measurements for other clinical outcomes, Tables 1 and 2.
Results
Literature review
Adherence to single versus multi inhaler triple therapy
The first search yielded eighteen articles, Suppl. Figure 1. After the selection process, eight articles were included for further evaluation, Table 1. None had a randomized controlled design. Four studies compared SITT with MITT in a prospective setting [23, 27, 28, 30] and four in a retrospective analysis [24,25,26, 29]. The retrospective studies used either anonymized data from electronic health records of patients in primary or secondary care [24, 26], or databases of health insurance claims [25, 29]. Seven of these studies showed that adherence and/or persistence to SITT was significantly higher compared to MITT in COPD patients [23,24,25, 27,28,29,30]. Deslee et al. presented contrasting findings, showing that while persistence was higher in the SITT group (median 181 versus 135 days), adherence levels were similar in SITT and MITT (85.7% versus 86.1%) [26]. The seven trials that showed a positive effect of SITT on adherence were heterogeneous in terms of study design, and methods of measurement, type of inhaler, and molecules. Although most studies directly compared SITT with MITT, two of the prospective studies assessed adherence to SITT after switching from either dual therapy or MITT [27, 28]. Brusselle et al. reported separate results for former MITT users: 71.9% at baseline, 74.7% three months after switching to SITT, and 83.8% at six months [28]. In contrast, Gessner et al. did not report separate results for the different treatments at baseline. Therefore, this difference between SITT and the control group should be interpreted with caution [27].
Clinical outcomes in single vs multi inhaler triple therapy
Five trials investigated the effect of SITT compared to MITT on clinical outcomes. Four of these trials showed a beneficial effect of SITT on clinical outcomes, Table 1. SITT users had a lower risk of exacerbations compared to MITT users in two studies [23, 28]; three studies showed lower CAT-scores and higher FEV1 in SITT users [27, 28, 30]; and one study showed a reduced all-cause mortality risk in SITT users [HR: 0.475 (0.237–0.952), p = 0.036] [23]. In contrast to these studies with positive effects of SITT, Bogart et al. showed different results in two different groups of patients. In patients enrolled in Medicare Advantage with Part D (MAPD) insurance, a significant reduction in exacerbations and healthcare utilisation was seen in the SITT group. However, these differences were not statistically significant in the commercially insured patients [29].
The effect of smart inhalers on adherence
The second part of our literature review investigated the effect of smart inhalers on adherence in patients with COPD and resulted in 78 articles, from which 11 studies were selected, Table 2. These studies were heterogenetic in terms of number of patients, study design, and type of intervention and/or smart inhaler. Additionally, length of follow-up ranged from 1 to 12 months, with the vast majority (90.9%) having a follow-up period of ≤ 6 months. Seven studies prospectively compared COPD patients who used a smart-inhalers with a control group; four of those had a randomized controlled open-label design. Six of these seven studies showed a statistically better adherence in the intervention group [19, 31, 32, 37, 38, 40]; one prospective study showed no difference in adherence between smart inhaler users and controls [33]. Four other observational studies showed variable average adherence rates in smart-inhaler users from 44–77%; however, it should be noted that these trials did not include a control group without smart-inhaler [34,35,36, 39].
The effect of smart inhalers on clinical outcomes
Nine studies also investigated the effect of smart inhalers on clinical outcomes [19, 31,32,33, 35,36,37,38,39]. These studies showed mixed results, Table 2. A significant better inhalation technique was seen in two studies [31, 33]. The impact of smart inhalers on other clinical outcomes, including exacerbations, disease burden, quality of life assessments, rescue medication usage, hospitalizations, and healthcare utilization, varied across different studies [19, 32, 33, 35,36,37,38,39].
Conclusion of literature review
This review suggests promising results concerning the effect of SITT, as opposed to MITT, and smart inhalers on adherence. However, the quality of evidence is limited due to the absence of randomized controlled trials and/or the short duration of follow-up in many studies. Moreover, there is considerable variation in the findings of these studies regarding diverse clinical outcomes. Consequently, there is a clear need for comprehensive randomised controlled trials to evaluate the benefits of SITT versus MITT in COPD, as well as the individual and combined effects of smart inhalers, both on adherence and clinical outcomes.
Study protocol for an RCT: the TRICOLON study
The TRICOLON study was initiated to provide evidence on two previously mentioned potential solutions for the non-adherence issue in COPD patients. The primary objective is to investigate whether the adherence to SITT is superior to the adherence to MITT over 12 months of treatment and to investigate whether the adherence of SITT users with a smart inhaler and digital support is superior to the adherence of MITT and SITT users without the smart inhaler and digital support. As a secondary objective, three methods of measuring adherence will be compared: smart inhaler data, self-reported data using the Test of Adherence to Inhalers (TAI) questionnaire [15], and drug analysis of formoterol in scalp hair samples [41]. Finally, differences in clinical outcomes between the study groups will be examined.
Study design
The TRICOLON study is an investigator-initiated, prospective, open-label, randomised, real-world, multicentre study. The study will be conducted at ten hospitals in the Netherlands, Supplement 2. Patients will be recruited from the pulmonary wards or outpatient clinics of the participating hospitals. Informed consent will be obtained by a member of the research team. Participants are randomly assigned in a 1:1:1 ratio to one of three groups: 1) multi-inhaler triple therapy (Bevespi® and Qvar®), 2) single-inhaler triple therapy (Trimbow®), 3) single-inhaler triple therapy (Trimbow®) with digital support, Fig. 1. The follow-up period will be one year, during which we aim to minimise disruption to their usual care, thus creating a (close to) real-world situation. The study outline is presented in Fig. 2. Ethical approval for this study was granted by the United Medical Research Ethics Committees (NL79938.100.22). The trial is registered on clinicaltrials.gov (NCT05495698).
Study participants
A total of 300 patients will be enrolled. Patients with a diagnosis of COPD and an indication for triple therapy according to their physician following the GOLD report are eligible to participate. Patients are excluded if asthma is the dominant diagnosis (asthma in the past or as a comorbidity is allowed), if patients use nebulizers or if they already use an e-health application for their COPD. The inclusion and exclusion criteria are displayed in Table 3.
Interventions
The study groups have uniform doses, identical molecules and doses (beclomethasone 100µg, formoterol 6µg, and glycopyrronium 10µg), and the same device type (pressurised metered dose inhaler). Therefore, the only differentiating factors are the number of devices used and the use of digital support. Digital support comprises the Findair® smart-inhaler, an electronic device that is attached to the inhaler and measures the frequency and time of the actuations, and the Curavista® platform (Gezondheidsmeter PGO), a digital platform that promotes patient self-management by displaying their medication use and providing medication intake reminders [31, 32]. Each patient is provided with smart inhalers that are attached to all their inhalers, including the potential rescue medication. This enables the measurement of actuation frequency and timing. The smart-inhalers are linked to the digital platform for data collection. However, it is important to note that only group 3 has access to an overview of the actuations with feedback in the app and reminders, along with full access to the digital platform. Groups 1 and 2 will not receive any reminders and cannot access the digital platform. Their e-health applications are solely used for data collection purposes, ensuring "silent monitoring" that should not influence their adherence.
We aim for all participants to complete the study using the original study medication. However, given the real-world nature of the study, it is possible that patients require a change in medication due to clinical reasons such as side effects or lack of effectiveness. To prevent the loss of these patients from the study, changes in medication are permitted only when absolutely necessary. Data collection will persist via the electronic devices and with the same settings of the app (silent monitoring or full access). Patients who no longer use a pressurized metered dose inhaler will be excluded, as the electronic devices are specifically tailored for this type of inhaler.
Outcomes
The primary outcome is the average adherence to ICS therapy (measured as the number of actuations registered by the smart-inhaler divided by the total number of doses prescribed, in %) over 12 months of treatment. As a secondary outcome, the average adherence to LABA/LAMA in study group 1 will be compared with adherence to ICS in group 1, and with adherence to LABA/LAMA/ICS in groups 2 and 3. Additional secondary outcomes include the percentage of patients with good adherence, defined as an average ICS adherence of more than 80% and less than 110% actuations measured by the smart inhaler; the Test of Adherence to Inhalers (TAI) scores; and drug levels of formoterol in scalp hair. The hair samples will be collected, stored, and prepared according to the guidelines of the Society of Hair Testing [42]. Additionally, the study will measure changes in Patient Reported Outcome Measures (PROMs), use of rescue medication, number of exacerbations and hospitalizations, healthcare consumption, and spirometry (FEV1). The PROMs are displayed in Supplement 3.
Statistical analysis
The statistical software G*Power version 3.1.9.6 was used to calculate the sample size. The study aims to compare three groups: group 1 vs group 2, group 2 vs group 3, and group 1 vs group 3. The sample size calculation is based on the comparison of the average adherence in group 1 vs group 2 (so MITT vs SITT without e-health). Based on a previous study [19], we expect a 15% difference between the groups, with a standard deviation of 30%. The significance level of the test was set at (alpha) 0.0167 using the Holm-Bonferroni method to adjust for multiple testing, as we are comparing three groups (alpha 0.05/3 = 0.0167), with a power of 80%. We calculated n = 84 for each group using a two-sided T-test, and plan to include 100 patients in each group of the study, considering a potential drop-out rate of 15%. The patients will be randomized using the program Castor EDC. To prevent inequality in the study groups, at randomization patients will be stratified for their treatment before the study (dual therapy, MITT or SITT) and for inclusion during an exacerbation or during stable disease. The data will be analyzed using both the intention-to-treat (primary analysis) and per-protocol methods. The Kruskal–Wallis test or ANOVA, as appropriate, will be used to compare the average adherence between the three study groups. Post-hoc comparisons will be performed using Mann–Whitney U tests or Tukey’s HSD, as appropriate. The average baseline scores of the PROMs and baseline clinical status (FEV1, number of exacerbations, hospitalizations and rescue medication use) will be presented descriptively. These scores and outcomes are all continuous, unpaired data and will be compared between more than two groups. Therefore, we will use the Kruskal–Wallis or ANOVA, as appropriate, to investigate the differences between the three groups. The Net Promoter score is a binary variable, so we will use the Chi-square test. Questionnaire data will be analysed by both the difference in mean scores between groups and the percentage of patients achieving the minimally clinical important difference (MCID) when available. Furthermore, a mixed model repeated measurement analysis will be performed to assess the differences in the previously mentioned outcomes over time. The analysis will be conducted on normally distributed data, with or without transformations. The main parameter of interest is the group * time interaction. Between-group comparisons will be adjusted using the method of Sidak. If the data cannot be normalized, difference scores will be calculated (follow-up – baseline). These differences will be analysed using either the Kruskal–Wallis test or ANOVA, where appropriate. Post-hoc comparisons will be conducted using Mann–Whitney U tests or Tukey’s HSD, where appropriate.
Safety
Serious adverse events (SAEs) will be monitored and reported in accordance with the legal requirements and deadlines. The Ethics committee has granted permission for hospital admissions resulting from a COPD exacerbation not to be reported as SAE. This exemption is due to their frequent occurrence in this specific population. Instead, to monitor this fragile population, a Data and Safety Monitoring Board (DSMB) has been established. The DSMB will periodically review mortality rates, serious adverse events, and premature withdrawals from the study every six months. The application and e-health platform in use have a substantial history, spanning many years. Over the past two decades, 26 peer-reviewed scientific publications have been published. Notably, there have been no reported safety concerns, and assessments of usability, feasibility, and efficacy consistently yield positive results [43].
Discussion
Non-adherence is a significant challenge in COPD patients, and addressing this issue is receiving increased attention. The first solution we investigated was simplifying the treatment by prescribing single-inhaler triple therapy (SITT) as an alternative to multi-inhaler triple therapy (MITT). The GOLD report 2023 suggested, for the first time, that single inhaler therapy may be more convenient than multi inhaler therapy [1]. However, although our literature review reveals some promising results regarding the effect of SITT on adherence, the quality of evidence is limited due to the absence of randomized controlled trials that specifically examined the difference in adherence between SITT and MITT. Due to the observational setting and design of all studies in the first part of this review, the SITT and MITT groups showed differences in their baseline characteristics, including the number of exacerbations prior to enrolment, disease severity, and FEV-1. Moreover, the quality of the observational data was occasionally limited. For example, two studies relied on administrative databases using health insurance claims [25, 29]. Consequently, from these trials we are unable to draw conclusions on the cause-effect relationship between improved adherence and clinical outcomes. In contrast to the four studies included in our review, which all demonstrated slightly better clinical outcomes in SITT users, other literature, not incorporated into our review due to a lack of adherence as an outcome, presented contrasting results regarding the effect of SITT on clinical outcomes. Specifically, a retrospective study in Spain and an RCT showed improved clinical outcomes in SITT users [44, 45]. However, three randomized controlled trials indicated that both SITT and MITT users exhibited similar results in terms of lung function, health status, exacerbation rate, and rescue medication usage [2, 46, 47].
The use of smart inhalers was the second potential solution to non-adherence that we investigated. Our review showed that while the effect on adherence was mostly positive, no consistent differences in clinical outcomes were observed. The strength of studies showing improved adherence in the absence of improved clinical outcomes is limited. These findings are consistent with other recent reviews in both COPD and asthma [18, 20, 21]. Demonstrating the connection between adherence and clinical outcomes has proven to be challenging. Given that COPD entails irreversible lung damage and the medication aims to stabilize rather than cure the disease, an extensive follow-up period is essential to demonstrate its impact on clinical outcomes. However, the current studies have limitations regarding the duration of follow-up. The smart inhalers used, as well as the supplementary interventions, and the extent of monitoring and/or interference varied significantly among the studies. The majority of smart inhalers used in current literature can only record the time and location of actuation. They are unable to measure whether inhalation is performed correctly. Other techniques, such as smart inhalers capable of measuring airflow or hair analysis of inhaled drugs, can assist in addressing this limitation. Further research is needed to gain a deeper understanding of the contributions of the different electronic modalities, the underlying mechanisms, clinical outcomes, and optimal implementation of these devices in clinical practice. Several challenges must be addressed before integrating smart inhalers into daily practice, including technical complexities, limited evidence concerning clinical outcomes, uncertainties about cost-effectiveness, and the issue of funding for the devices [18]. The TRICOLON study aims to offer additional evidence, potentially bringing us closer to their use in daily practice.
To the best of our knowledge, the TRICOLON trial is the first that aims to investigate whether single inhaler usage in COPD patients receiving triple therapy can improve adherence in a large-scale, randomized, controlled, real-world setting. Moreover, unlike the majority of existing studies focusing on the impact of smart inhalers, the TRICOLON trial distinguishes itself with a prolonged follow-up period of one year. We acknowledge that patients’ adherence may be influenced by their awareness of participating in a study. To minimize this interference, we have limited the number of study visits to closely resemble real-world settings. Additionally, patients are informed that the focus of this study is on the convenience of various treatment options, and adherence is not specifically mentioned in the information provided by the researchers or in the patient information letter. This has been approved by the Medical Ethical Review Board. The Tricolon study not only investigates the impacts of a single inhaler and the use of a smart inhaler on adherence but also evaluates various clinical outcomes, including exacerbation rates, hospitalizations, and disease burden. Nevertheless, the study is powered on the primary outcome adherence to inhalation therapy. Therefore, although not powered for the clinical outcomes or for the correlation between adherence and clinical outcomes, valuable information on these outcomes will be collected to inform possible follow-up studies.
The implementation of an e-health application may present challenges, whether due to technical issues or the potential unfamiliarity among patients and healthcare professionals [48]. To proactively address these concerns, we dedicated time to thoroughly test the application before the start of the study. This involved multiple stakeholders, including the researchers, the app producer, and patients. Moreover, the application's design is intentionally kept simple and clear, ensuring that individuals of all ages, educational backgrounds, and health literacy levels can easily comprehend and use it. This was confirmed in a previous study where an older, and thus more digitally challenged, population of patients with Idiopathic Pulmonary Fibrosis (IPF) used this app for daily spirometry. The study found that 80% of the participants found the app easy to use, and 90% did not perceive it as burdensome [49].
Beyond addressing the primary research questions, this TRICOLON study creates an opportunity for a direct comparison between three methods to measure adherence: digital data from the smart inhaler, self-reported data collected through the TAI questionnaire, and drug deposition data in hair. The use of this final technique is relatively uncommon in studies concerning inhalation medication, although it has been used in previous research related to cortisol and in forensic studies [22, 50]. In a specific study involving asthma and COPD patients, the measurement of inhalation medication demonstrated a clear dose–response relationship among those using formoterol [41].
Our identification of a lack of high-quality data on the improvement of adherence of SITT over MITT therapy in COPD and limited data for smart inhalers highlights the need for further research. The multi-centre, randomized controlled, three-arm, real-world TRICOLON trial aims to increase insight in the value of SITT and the added value of electronic adherence monitoring.
Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Global Initiative for Chronic Obstructive Lung Disease. 2023 Report: global strategy for prevention, diagnosis and management of COPD [Available from: https://goldcopd.org/2023-gold-report-2/.
Vestbo J, Papi A, Corradi M, Blazhko V, Montagna I, Francisco C, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–29.
Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD. N Engl J Med. 2018;378(18):1671–80.
Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–84.
Singh D, Papi A, Corradi M, Pavlisova I, Montagna I, Francisco C, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting beta2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–73.
Ferguson GT, Rabe KF, Martinez FJ, Fabbri LM, Wang C, Ichinose M, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–58.
Lipson DA, Crim C, Criner GJ, Day NC, Dransfield MT, Halpin DMG, et al. Reduction in All-Cause Mortality with Fluticasone Furoate/Umeclidinium/Vilanterol in Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2020;201(12):1508–16.
Rabe KF, Martinez FJ, Ferguson GT, Wang C, Singh D, Wedzicha JA, et al. Triple Inhaled Therapy at Two Glucocorticoid Doses in Moderate-to-Very-Severe COPD. N Engl J Med. 2020;383(1):35–48.
Bhattarai B, Walpola R, Mey A, Anoopkumar-Dukie S, Khan S. Barriers and strategies for improving medication adherence among people living with COPD: a systematic review. Respir Care. 2020;65(11):1738–50.
van Boven JF, Chavannes NH, van der Molen T, Rutten-van Molken MP, Postma MJ, Vegter S. Clinical and economic impact of non-adherence in COPD: a systematic review. Respir Med. 2014;108(1):103–13.
Cushen B, Sulaiman I, Greene G, MacHale E, Mokoka M, Reilly RB, et al. The clinical impact of different adherence behaviors in patients with severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(12):1630–3.
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
Vrijens B, Dima AL, Van Ganse E, van Boven JF, Eakin MN, Foster JM, et al. What we mean when we talk about adherence in respiratory medicine. J Allergy Clin Immunol Pract. 2016;4(5):802–12.
George J, Kong DC, Stewart K. Adherence to disease management programs in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(3):253–62.
Plaza V, Fernandez-Rodriguez C, Melero C, Cosio BG, Entrenas LM, de Llano LP, et al. Validation of the “Test of the Adherence to Inhalers” (TAI) for Asthma and COPD Patients. J Aerosol Med Pulm Drug Deliv. 2016;29(2):142–52.
Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: Myth and reality. Respir Med. 2017;129:117–23.
Loucks J, Zuckerman AD, Berni A, Saulles A, Thomas G, Alonzo A. Proportion of days covered as a measure of medication adherence. Am J Health Syst Pharm. 2022;79(6):492–6.
Jansen EM, van de Hei SJ, Dierick BJH, Kerstjens HAM, Kocks JWH, van Boven JFM. Global burden of medication non-adherence in chronic obstructive pulmonary disease (COPD) and asthma: a narrative review of the clinical and economic case for smart inhalers. J Thorac Dis. 2021;13(6):3846–64.
O’Dwyer S, Greene G, MacHale E, Cushen B, Sulaiman I, Boland F, et al. Personalized biofeedback on inhaler adherence and technique by community pharmacists: a cluster randomized clinical trial. J Allergy Clin Immunol Pract. 2020;8(2):635–44.
Garin N, Zarate-Tamames B, Gras-Martin L, Milà R, Crespo-Lessmann A, Curto E, Hernandez M, Mestres C, Plaza V. Clinical Impact of Electronic Monitoring Devices of Inhalers in Adults with Asthma or COPD: A Systematic Review and Meta-Analysis. Pharmaceuticals (Basel). 2023;16(3):414. https://doi.org/10.3390/ph16030414.
Schulte MHJ, Aardoom JJ, Loheide-Niesmann L, Verstraete LLL, Ossebaard HC, Riper H. Effectiveness of eHealth Interventions in Improving Medication Adherence for Patients With Chronic Obstructive Pulmonary Disease or Asthma: Systematic Review. J Med Internet Res. 2021;23(7):e29475.
Rygaard K, Linnet K, Johansen SS. A Systematic Review of Metabolite-to-Drug Ratios of Pharmaceuticals in Hair for Forensic Investigations. Metabolites. 2021;11(10):686. https://doi.org/10.3390/metabo11100686.
Lin L, Liu C, Cheng W, Song Q, Zeng Y, Li X, et al. Comparison of treatment persistence, adherence, and risk of exacerbation in patients with COPD treated with single-inhaler versus multiple-inhaler triple therapy: A prospective observational study in China. Front Pharmacol. 2023;14:1147985.
Halpin DMG, Rothnie KJ, Banks V, Czira A, Compton C, Wood R, et al. Comparative Adherence and Persistence of Single- and Multiple-Inhaler Triple Therapies Among Patients with Chronic Obstructive Pulmonary Disease in an English Real-World Primary Care Setting. Int J Chron Obstruct Pulmon Dis. 2022;17:2417–29.
Mannino D, Bogart M, Wu B, Germain G, Laliberte F, MacKnight SD, et al. Adherence and persistence to once-daily single-inhaler versus multiple-inhaler triple therapy among patients with chronic obstructive pulmonary disease in the USA: A real-world study. Respir Med. 2022;197:106807.
Deslee G, Fabry-Vendrand C, Poccardi N, Thabut G, Eteve Pitsaer C, Coriat A, Renaudat C, Maguire A, Pinto T. Use and persistence of single and multiple inhaler triple therapy prescribed for patients with COPD in France: a retrospective study on THIN database (OPTI study). BMJ Open Respir Res. 2023;10(1):e001585. https://doi.org/10.1136/bmjresp-2022-001585.
Gessner C, Trinkmann F, Bahari Javan S, Hovelmann R, Bogoevska V, Georges G, et al. Effectiveness of Extrafine Single Inhaler Triple Therapy in Chronic Obstructive Pulmonary Disease (COPD) in Germany - The TriOptimize Study. Int J Chron Obstruct Pulmon Dis. 2022;17:3019–31.
Brusselle G, Himpe U, Fievez P, Leys M, Perez Bogerd S, Peche R, et al. Evolving to a single inhaler extrafine LABA/LAMA/ICS - Inhalation technique and adherence at the heart of COPD patient care (TRIVOLVE). Respir Med. 2023;218:107368.
Bogart M, Bengtson LGS, Johnson MG, Bunner SH, Gronroos NN, DiRocco KK. Outcomes Following Initiation of Triple Therapy with Fluticasone Furoate/Umeclidinium/Vilanterol versus Multiple-Inhaler Triple Therapy Among Medicare Advantage with Part D Beneficiaries and Those Commercially Enrolled for Health Care Insurance in the United States. Int J Chron Obstruct Pulmon Dis. 2024;19:97–110.
Beeh KM, Scheithe K, Schmutzler H, Kruger S. Real-World Effectiveness of Fluticasone Furoate/Umeclidinium/Vilanterol Once-Daily Single-Inhaler Triple Therapy for Symptomatic COPD: The ELLITHE Non-Interventional Trial. Int J Chron Obstruct Pulmon Dis. 2024;19:205–16.
Hesso I, Nabhani-Gebara S, Kayyali R. Objective Assessment of Adherence and Inhaler Technique among Asthma and COPD Patients in London: A Study in Community Pharmacies Using an Electronic Monitoring Device. Pharmacy (Basel). 2023;11(3):94. https://doi.org/10.3390/pharmacy11030094.
Criner GJ, Cole T, Hahn KA, Kastango K, Eudicone J, Gilbert I. The Impact of Budesonide/Formoterol pMDI Medication Reminders on Adherence in Chronic Obstructive Pulmonary Disease (COPD) Patients: Results of a Randomized, Phase 4, Clinical Study. Int J Chron Obstruct Pulmon Dis. 2021;16:563–77.
Dierick BJH, Been-Buck S, Klemmeier T, Hagedoorn P, van de Hei SJ, Kerstjens HAM, et al. Digital spacer data driven COPD inhaler adherence education: The OUTERSPACE proof-of-concept study. Respir Med. 2022;201:106940.
Kaye L, Gondalia R, Thompson A, Stempel DA, Barrett MA. The relationship between objective app engagement and medication adherence in asthma and COPD: a retrospective analysis. Sci Rep. 2021;11(1):24343.
Yawn BP, McCreary GM, Linnell JA, Pasquale CB, Malanga E, Choate R, et al. Pilot Study of a Patient Experience with an ELLIPTA Inhaler electronic medication monitor and associated integrated system: a prospective observational study using the COPD Patient-Powered Research Network. Chronic Obstr Pulm Dis. 2021;8(4):488–501.
Kaye L, Gondalia R, Barrett MA, Williams M, Stempel DA. Concurrent improvement observed in patient-reported burden and sensor-collected medication use among patients enrolled in a COPD Digital Health Program. Front Digit Health. 2021;3:624261.
Gregoriano C, Dieterle T, Breitenstein AL, Durr S, Baum A, Giezendanner S, et al. Does a tailored intervention to promote adherence in patients with chronic lung disease affect exacerbations? A randomized controlled trial. Respir Res. 2019;20(1):273.
Broadbent E, Garrett J, Jepsen N, Li Ogilvie V, Ahn HS, Robinson H, et al. Using Robots at Home to Support Patients With Chronic Obstructive Pulmonary Disease: Pilot Randomized Controlled Trial. J Med Internet Res. 2018;20(2):e45.
Alshabani K, Attaway AA, Smith MJ, Majumdar U, Rice R, Han X, et al. Electronic inhaler monitoring and healthcare utilization in chronic obstructive pulmonary disease. J Telemed Telecare. 2020;26(7–8):495–503.
Nides MA, Tashkin DP, Simmons MS, Wise RA, Li VC, Rand CS. Improving inhaler adherence in a clinical trial through the use of the nebulizer chronolog. Chest. 1993;104(2):501–7.
Hassall D, Brealey N, Wright W, Hughes S, West A, Ravindranath R, et al. Hair analysis to monitor adherence to prescribed chronic inhaler drug therapy in patients with asthma or COPD. Pulm Pharmacol Ther. 2018;51:59–64.
Cooper GA, Kronstrand R, Kintz P, Society of Hair T. Society of Hair Testing guidelines for drug testing in hair. Forensic Sci Int. 2012;218(1–3):20–4.
Alcazar-Navarrete B, Jamart L, Sanchez-Covisa J, Juarez M, Graefenhain R, Sicras-Mainar A. Clinical Characteristics, Treatment Persistence, and Outcomes Among Patients With COPD Treated With Single- or Multiple-Inhaler Triple Therapy: A Retrospective Analysis in Spain. Chest. 2022;162(5):1017–29.
Halpin DMG, Worsley S, Ismaila AS, Beeh KM, Midwinter D, Kocks JWH, Irving E, Marin JM, Martin N, Tabberer M, Snowise NG, Compton C. INTREPID: single- versus multiple-inhaler triple therapy for COPD in usual clinical practice. ERJ Open Res. 2021;7(2):00950–2020. https://doi.org/10.1183/23120541.00950-2020.
Ferguson GT, Brown N, Compton C, Corbridge TC, Dorais K, Fogarty C, et al. Once-daily single-inhaler versus twice-daily multiple-inhaler triple therapy in patients with COPD: lung function and health status results from two replicate randomized controlled trials. Respir Res. 2020;21(1):131.
Bremner PR, Birk R, Brealey N, Ismaila AS, Zhu CQ, Lipson DA. Single-inhaler fluticasone furoate/umeclidinium/vilanterol versus fluticasone furoate/vilanterol plus umeclidinium using two inhalers for chronic obstructive pulmonary disease: a randomized non-inferiority study. Respir Res. 2018;19(1):19.
Pinnock H, Hui CY, van Boven JFM. Implementation of digital home monitoring and management of respiratory disease. Curr Opin Pulm Med. 2023;29(4):302–12.
Moor CC, Wapenaar M, Miedema JR, Geelhoed JJM, Chandoesing PP, Wijsenbeek MS. A home monitoring program including real-time wireless home spirometry in idiopathic pulmonary fibrosis: a pilot study on experiences and barriers. Respir Res. 2018;19(1):105.
Greff MJE, Levine JM, Abuzgaia AM, Elzagallaai AA, Rieder MJ, van Uum SHM. Hair cortisol analysis: An update on methodological considerations and clinical applications. Clin Biochem. 2019;63:1–9.
Acknowledgements
We appreciate the assistance of Carmen van der Heijden, librarian at the Medical Library in the Franciscus Gasthuis & Vlietland hospital, in conducting the PubMed searches. We would like to thank the members of the investigational teams across all participating hospitals for their dedicated time and effort in conducting this study.
TRICOLON study group
The TRICOLON Study Group consortium consists of the individuals listed below:
Liz J.A. Cuperus MD1,2,3, Job van der Palen PhD4, Arnoud Aldenkamp MD5, Astrid van Huisstede MD PhD6, Erik W.M.A. Bischoff MD PhD7, Job F.M. van Boven PharmD PhD8, Folkert Brijker MD9, Stephan Dik MD10, Jeroen A.J.M. van Excel MD11, Martijn Goosens MD12, Peter Th.W. van Hal MD PhD13, Jolanda C. Kuijvenhoven MD PhD14, Lisette I.Z. Kunz MD PhD15, Erwin C. Vasbinder PhD16, Huib A.M. Kerstjens MD PhD2, Johannes C.C.M. in ’t Veen MD PhD 1,3, Marjo van der Poel17, Marijke Amelink9, Anke Rol18, Jennifer de Graaf18, Petra Hirmann19, Fleur van Tour20, Elly Jordens13, Lydia Alfing13, Gerda Lenderink21, Thecla Rupert21, Truus Rietveld21, Jasmijn van Campen15, Jantine de Bruijn15, Janice van ter Burg15, Walter van Litsenburg5, Len Knoops22, Margot Eggermont-Schilt23, Manon de Waard-Heijligers23, Ilonka Paalvast-Schouten23, Sarah van Oord11
1Pulmonology Department, Franciscus Gasthuis and Vlietland, Rotterdam, the Netherlands
2Pulmonology Department, University of Groningen, University Medical Center Groningen, and Groningen Research Institute for Asthma and COPD, Groningen, the Netherlands
3Pulmonology Department, Erasmus Medical Centre, Rotterdam, the Netherlands
4Department of Epidemiology, Medisch Spectrum Twente, Enschede, The Netherlands
5Department of Pulmonary Medicine, Catharina Hospital, Eindhoven, The Netherlands
6Department of Pulmonology, Northwest Clinics, Alkmaar, the Netherlands
7Department of Primary and Community Care, Radboud University Medical Center, Nijmegen, Netherlands
8Department of Clinical Pharmacy & Pharmacology Groningen Research Institute for Asthma and COPD (GRIAC), University Medical Center Groningen, University of Groningen, Groningen, The Netherlands
9Department of Pulmonary Medicine, Spaarne Gasthuis, Haarlem, The Netherlands
10Department of Pulmonary Medicine, Albert Schweitzer ziekenhuis, Dordrecht, The Netherlands
11Department of Pulmonary Medicine, HagaZiekenhuis, The Hague, The Netherlands
12Department of Pulmonary Medicine, Gelre Ziekenhuizen, Zutphen, The Netherlands
13Department of Respiratory Medicine, Van Weel-Bethesda Hospital, Dirksland, the Netherlands
14Department of Respiratory Medicine, Medical Centre Leeuwarden, Leeuwarden, the Netherlands
15Department of Pulmonology, Haaglanden Medical Centre, The Hague, the Netherlands
16Department of Clinical Pharmacy, Franciscus Gasthuis, Rotterdam, the Netherlands
17Spaarne Gasthuis, Haarlem, The Netherlands
18Northwest Clinics, Alkmaar, the Netherlands
19Medical Centre Leeuwarden, Leeuwarden, the Netherlands
20Albert Schweitzer ziekenhuis, Dordrecht, The Netherlands
21Gelre Ziekenhuizen, Zutphen, The Netherlands
22Catharina Hospital, Eindhoven, The Netherlands
23HagaZiekenhuis, The Hague, The Netherlands
Funding
The faculty received an unrestricted grant from Chiesi Pharmaceuticals B.V. Furthermore, the funding includes contributions from the research group in the Franciscus Gasthuis & Vlietland hospital and transformation funds from health insurance companies.
Author information
Authors and Affiliations
Consortia
Contributions
LC and JV conducted the assessment and selection of articles from the PubMed searches, HK was consulted in case of author disagreements. JV initiated the Tricolon trial and acquired the funding. LC, JV, HK, JvdP, EB, JvB were involved in the study design and protocol. LC is the coordinating investigator, JV is the principal investigator. LC, JV and HK wrote the main manuscript text. All authors have thoroughly read, critically revised, and approved the submitted version of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the Tricolon study was waived by the Medical research Ethics Committees United (NL79938.100.22). This study is performed after approval by the Institutional Research Board and Board of Directors of the participating hospitals. The study is registered at clinicaltrials.gov (NCT05495698). Informed consent was obtained from all subjects.
Consent for publication
Not Applicable.
Competing interests
LC: none.
JvdP: none.
AA: none.
AvH: none.
EB: unrestricted grants and speaking fees received from Chiesi Pharmaceuticals B.V., Boehringer Ingelheim bv, GlaxoSmithKline.
JvB: received unrestricted research grants from Aardex, AstraZeneca, Chiesi, European Commission COST Action 19132 (ENABLE), European Respiratory Society CRC “CONNECT”, Novartis, Pfizer, Pill Connect, Trudell Medical and consultancy/speaker fees from AstraZeneca, Chiesi, GSK, Novartis, Teva and Vertex. All payments were unrelated to this manuscript and all paid to his institution (UMCG).
FB: none.
SD: none.
JvE: none.
MG: none.
PvH: none.
JK: none.
LK: received speaker fees from AZ.
EV: received unrestricted research grants from AstraZeneca and Pfizer.
HK: reports grants and consultancy/advisory board participation from/for AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, and Novartis, all outside the submitted work. All were paid to his institution.
JiV: received unrestricted faculty research grants from GSK, Teva, AZ, Chiesi, Sanofi, and speaker fees from AZ, GSK, Sanofi, Chiesi, Stichting RoLeX and Health Investment.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cuperus, L.J.A., van der Palen, J., Aldenkamp, A. et al. Adherence to single inhaler triple therapy and digital inhalers in Chronic Obstructive Pulmonary Disease: a literature review and protocol for a randomized controlled trial (TRICOLON study). BMC Pulm Med 24, 317 (2024). https://doi.org/10.1186/s12890-024-03044-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03044-3