Abstract
Background
There is currently a lack of comprehensive prevalence information on arthritis and its various classifications among adults in the U.S., particularly given the notable absence of detailed data regarding the Asian population. We examined the trends in the prevalence of arthritis, including osteoarthritis (OA), rheumatoid arthritis (RA), psoriatic arthritis (PsA), and other types of arthritis, among U.S. adults by race between 2011 and 2018.
Methods
We analyzed data from the National Health and Nutrition Examination Survey (NHANES), spanning from 2011 to 2018. Our study focused on a nationally representative sample of U.S. adults aged 20 and older. Participants who answered “y es” to the research question “Doctors ever said you had arthritis?” were classified as having arthritis. Further classification into specific diseases was based on responses to the question “Which type of arthritis was it?” with options including “OA or degenerative arthritis, ” “RA, ” “PsA, ” or “Other. ”
Results
We analyzed 22,566 participants from NHANES (2011–2018), averaging 44.8 years, including 10,927 males. The overall arthritis prevalence rose significantly from 22.98% (95% CI: 21.47–24.55%) in 2011–12 to 27.95% (95% CI: 26.20–29.76%) in 2017–18 (P for trend < 0.001). OA increased from 12.02% (95% CI: 10.82–13.35%) in 2011 to 14.93% (95% CI: 13.47–16.51%) in 2018 (P for trend < 0.001). RA and PsA remained stable (P for trend = 0.220 and 0.849, respectively), while other arthritis rose from 2.03% (95% CI: 1.54–2.67%) in 2011–12 to 3.14% (95% CI: 2.56–3.86%) in 2017–18 (P for trend = 0.001). In Whites, Asians, and other races , arthritis and RA prevalence increased significantly (P for trend < 0.05). OA and other arthritis rose in Whites and other races (P for trend < 0.05), but no significant change occurred in the black population. The prevalence of PsA remained stable across all racial groups, with no statistically significant changes.
Conclusions
In this nationally representative U.S. adult survey spanning 2011 to 2018, we identified a rising prevalence trend in arthritis, OA, and other arthritis, with notable variations among different racial groups.
Similar content being viewed by others
Introduction
The term “arthritis, ” derived from the Greek language, signifies “joint disease. ” It is characterized by inflammation, acute or chronic, in the joints, often accompanied by pain and structural damage [1]. The common types are osteoarthritis (OA), rheumatoid arthritis (RA), and psoriatic arthritis (PsA) [2, 3]. These conditions may lead to joint discomfort, limited functionality, and decreased mobility, significantly reducing patients’ quality of life [4, 5]. With an aging population and improved survival rates, arthritis incidence and prevalence are on the rise [6,7,8]. Arthritis, recognized as a leading cause of disability by the World Health Organization, not only causes individual suffering but also poses substantial economic and healthcare burdens on society [6, 9]. Therefore, accurately predicting the incidence and trends of chronic diseases like arthritis is vital for planning clinical and public health strategies, sha** health policies, and allocating resources effectively.
In 2017, the age-standardized prevalence rates of OA [10] and RA [6] globally were 3.75% and 0.25%, respectively, showing increases of 9.3% and 7.4%, respectively, since 1990. Few studies have reported on the prevalence and trends of OA [2, 11, 12], RA [2, 13], and PsA [14, 15] in the U.S., but these results vary. For instance, Park [2] and Hunter [13] have opposing views on the prevalence of RA in the U.S. Park’s study found that the prevalence of RA was 5.9% in 1999−2000, which decreased to 3.8% by 2013−14 [2]; whereas Hunter posits that the prevalence of RA has been on an upward trend from 2004 to 2014 [13]. Regarding PsA, prevalence estimates exhibit considerable variability, ranging from 0.02% to 0.25%, with recent estimates being higher [15]. It is noteworthy that most previous studies have focused primarily on trends in the prevalence of arthritis before 2014, leaving us with limited knowledge about these trends thereafter.
The National Health and Nutrition Examination Survey (NHANES) cycles from 2011 to 2018 oversampled non-Hispanic Asians and provided additional sampling for traditionally oversampled groups, including Hispanic and non-Hispanic Black populations [16]. Prior to the 2011–12 NHANES cycle, data for non-Hispanic Asians were amalgamated with other racial categories in publicly released information. As of 2017, the U.S. Asian population has reached 18.3 million, accounting for 5.7% of the total population, and is expected to reach 36.8 million (9.1%) by 2060 [17]. Despite being the fastest-growing racial group in the U.S. [18], Asians are underrepresented in health research [19], a trend seen in other Western countries. Given the sustained growth of the Asian American population, obtaining comprehensive insights into their health status and trends is imperative.
This study aims to fill a critical data gap by examining the prevalence and trends of arthritis among Asian Americans on a national level, facilitating comparisons with other racial groups. Using NHANES data from 2011 to 2018, we conducted a thorough analysis of arthritis trends in U.S. adults, including OA, RA, PsA, and other arthritis, while accounting for variables like age, sex, and race.
Methods
NHANES study population
The NHANES, conducted by the National Center for Health Statistics (NCHS) under the CDC, is a nationally representative survey using a complex, multistage probability sampling design [20]. The survey comprises two main components: interviews and physical examinations. During interviews, participants responded to questions related to demographics, socioeconomic factors, diet, and health. The examinations included medical, dental, and physiological measurements [21]. Since 2011, the NHANES has oversampled non-Hispanic Asians to enhance the statistical precision for this population. Despite a decrease in response rates from 66% in 2011–12 to 47.7% in 2017–18, the CDC has meticulously assessed the data and implemented improved weighting adjustments to minimize potential nonresponse bias [22]. NHANES procedures were approved by the NCHS Institutional Review Board (https://www.cdc.gov/nchs/nhanes/irba98.htm), and written consent was obtained from all adult participants. Additional details on NHANES methods and data acquisition are available on the NHANES website (https://www.cdc.gov/nchs/nhanes/index.htm).
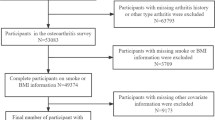
Arthritis in NHANES
Participants who answered “y es” to the research question “Doctors ever said you had arthritis?” were classified as having arthritis. Further classification into specific diseases was based on responses to the question “Which type of arthritis was it?” with options including “OA or degenerative arthritis, ” “RA, ” “PsA, ” or “Other. ” Our study focused on adults aged 20 years and older who answered questions about arthritis in four NHANES cycles (2011–12 to 2017–18). Among the 22,617 adults who participated in the NHANES from 2011 to 2018, 51 participants lacking arthritis data and 1, 719 participants lacking classification interview data were excluded. Ultimately, we obtained arthritis data from 22,566 adults and arthritis classification data from 20,898 adults.
Covariates in NHANES
During the interview phase, we employed standardized questionnaires to collect information on age, gender, and race. The NHANES questionnaire is available in two versions: English and Spanish. For participants who were not proficient in English or Spanish, and those with limited English proficiency, an interpreter provided assistance during the interview.
Racial classifications were self-reported and included Mexican American, Other Hispanic, Non-Hispanic White (referred to as White), Non-Hispanic Black (referred to as Black), Non-Hispanic Asian (encompassing East Asia, Southeast Asia, or the Indian subcontinent, such as Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippines, Thailand, and Vietnam; referred to as Asian), and Other Race (comprising American Indian, Alaskan Native, Native Hawaiian, Pacific Islander, and individuals with multiple racial backgrounds). Non-Hispanic participants reporting multiple racial backgrounds were categorized as “Other Race” [23, 24].
Statistical analysis
Following NHANES analysis guidelines, we applied sample weights in the stratified multistage probability design, as recommended by NHANES, to obtain variance estimates. Given the complex nature of the factors influencing arthritis prevalence and for comparison with previous reports from the CDC, we calculated the prevalence of various types of arthritis in the U.S. adult population for each NHANES cycle from 2011– 12 to 2017–18 (expressed as percentages) based on 2000 census data and NHANES recommendations. We conducted stratified analyses by age, sex, and race. Trends over time were explored using logistic regression, treating the survey cycle as a continuous independent variable. Unweighted values and trends were also calculated for sensitivity analysis. Statistical analyses utilized STATA 17.0 and Empower (R) (https://www.empowerstats.net/cn), with statistical significance set at P < 0.05.
Results
This study employed different sample sizes for distinct measurements: the arthritis sample included 22,566 individuals, while samples for OA, RA, PsA, and other arthritis comprised 20,898 individuals. In the overall study sample, the weighted average age was 44.8 years (SE = 0.15); 10,927 were males (weighted 48.08%), and 11,639 were females (weighted 51.92%). There were 3, 030 Mexican Americans (weighted 8.63%), 2, 364 other Hispanic Americans (weighted 6.38%), 8291 Whites (weighted 64.58%), 5, 120 B lacks (weighted 11.45%), 2, 955 Asians (weighted 5.58%), and 806 individuals of other races (weighted 3.38%). Sample sizes and overall characteristics varied slightly across survey cycles, with detailed descriptions in Supplementary Table S1. Additionally, Supplementary Table S2 presents unweighted sample sizes for adults aged 20 and above in NHANES 2017–18, stratified by sex, age, and race.
Arthritis
Table 1, Fig. 1A, and Supplementary Figure S1A present the arthritis prevalence from 2011 to 2018, along with the estimated prevalence stratified by sex, age group, and race. The overall prevalence significantly increased from 22.98% (95% CI: 21.47–24.55%) in 2011–12 to 27.95% (95% CI: 28.20–30.4%) in 2017–18 (P for trend < 0.001). The prevalence among males increased from 18.60% (95% CI: 16.59–20.79%) to 24.72% (95% CI: 22.22–27.40%) (P for trend < 0.001), while among females, it increased from 27.00% (95% CI: 24.83–29.30%) to 30.94% (95% CI: 28.55–33.44%) (P for trend < 0.001). Stratification by quartile revealed a significant increase in arthritis prevalence among the 51- to 64-year-old age group (32.58–39.70%, P for trend < 0.001) and the 65- to 80-year-old age group (49.92–56.49%, P for trend = 0.002).
In addition, we observed that the prevalence of arthritis among females was consistently higher than that among males across all years (Supplementary Figure S1A). The rates increased significantly in the White, Asian, and other racial groups (P for trend < 0.001, 0.004, < 0.001, respectively). The increase observed in Black and Asian populations was primarily among males, while increases in W hite and other racial groups were observed in both sexes. Supplementary Table S3 presents the unweighted arthritis prevalence and trends, with notable differences in overall prevalence observed in the 20- to 34-year-old and 25- to 50-year-old age groups , followed by W hite women.
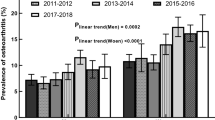
Osteoarthritis
In the overall population, the weighted prevalence of OA was 12.02% (95% CI: 10.82–13.35%), 15.29% (95% CI: 14.06–16.60%), 13.84% (95% CI: 12.53–15.27%) and 14.93% (95% CI: 13.47–16.51%) from 2011– 12 to 2017–18, respectively (P trend for < 0.001) (Table 2 and Fig. 1B). An increase in prevalence was primarily observed in White individuals (14.97–18.63%, P for trend < 0.001) and other races (11.07–19.10%, P for trend < 0.009). When stratified by age, we observed changes consistent with those of arthritis. H owever, in the 20- to 34-year-old age group, there was a decrease from 1.86% (95% CI: 1.12–3.10%) in 2011–12 to 0.99% (95% CI: 0.59–1.64%) in 2017–18 (P for trend = 0.007). Increases in prevalence were observed in both sexes (Table 2 and Supplementary Figure S1B), with a notable increase in the other racial group of male from 3.96% (95% CI: 1.56–9.72%) in 2011–12 to 16.89% (95% CI: 8.36–31.14%) in 2017–18, while growth in females was primarily observed in the W hite population (P for trend = 0.009). Supplementary Table S4 displays the unweighted prevalence and trends of OA.
Rheumatoid arthritis
The prevalence of RA remained stable from 2011 to 2018, with rates of 3.84% (95% CI: 3.20–4.61%), 4.01% (95% CI: 3.42–4.69%), 4.12% (95% CI: 3.50–4.85%), and 4.61% (95% CI: 3.88–5.48%) (P for trend = 0.220) (Table 3; Fig. 1C), with no statistically significant differences observed among age groups. When stratified by race, while B lack individuals had the highest prevalence, the rate remained stable (P for trend = 0.181) (Table 3). However, an increasing trend in RA prevalence was observed in other Hispanic (P for trend < 0.001), Asian (P for trend = 0.001), and other racial groups (P for trend = 0.023); among these, an increase in prevalence among Asians (P for trend < 0.001) and other racial groups (P for trend < 0.001) was mainly driven by males, while in the other Hispanic group, the increase was primarily seen in females (P for trend = 0.006). Gender-stratified analysis revealed an increase in prevalence only in males (Table 3 and Supplementary Figure S1C), with a gradual increase in age at onset observed in males (P for trend = 0.024), while no such difference was observed among females (eFig. 1C). Supplementary Table S5 presents the unweighted prevalence and trends of RA.
Psoriatic arthritis
Over the period from 2011 to 2018, the prevalence of PsA among adults in the U.S. remained stable (P for trend = 0.849), both in the overall population and when stratified by sex, age, and race (P for trend > 0.05) (Table 4; Fig. 1D; and Supplementary Figure S1D). Supplementary Table S6 provides a detailed overview of the unweighted prevalence and trends of PsA, showing no significant differences.
Other Arthritis
The overall prevalence of other arthritis increased from 2.03% (95% CI: 1.54–2.67%) in 2011–12 to 3.14% (95% CI: 2.56–3.86%) in 2017–18 (P for trend = 0.001) (Table 5; Fig. 1E). However, this increasing trend was significant only for White individuals (P for trend = 0.021) and individuals from other racial backgrounds (P for trend = 0.033). Age-stratified analysis revealed that growth was primarily concentrated in the 35- to 50-year-old age group (P for trend = 0.009) and the 65- to 80-year-old age group (P for trend = 0.002). Gender-stratified analysis indicated an increase in prevalence in both sexes, but it was more pronounced in the female population (P for trend = 0.022), while the male population did not show significant differences (P for trend = 0.091) (Table 5 and Supplementary Figure S1E). Supplementary Table S7 provides unweighted prevalence and trends for other arthritis, demonstrating opposite trends between male and female populations in weighted data.
Discussion
This study, using nationally representative data encompassing diverse racial backgrounds, offers detailed estimates of the national trends in various types of arthritis among U.S. adults from 2011–12 to 2017–18. We explore these trends across age, sex, and racial groups. Overall, the prevalence of arthritis in U.S. adults remains relatively high and is on the rise, although significant differences exist among different sexes, age groups, and racial groups . The White population shows an increasing trend in arthritis, OA, and other types of arthritis, while the Asian population exhibits an increase in the prevalence of arthritis and RA. The other Hispanic group only showed an increase in RA prevalence. In contrast, Black and Mexican American individuals demonstrate relatively stable prevalence rates across various types of arthritis. Other racial groups are the only ones showing an increase in all types of arthritis, except for PsA.
In the U.S., doctor-diagnosed arthritis is a prevalent chronic condition [25, 26] and a major cause of disability [27], contributing to approximately $81 billion in annual direct medical expenses related to arthritis [28]. Annually, approximately one million knee and hip replacements are performed, 99% of which are attributed to pain and functional limitations caused by arthritis [29]. The aging population is a driving factor in predicting the prevalence of arthritis and its associated impacts [30]. This study revealed an arthritis prevalence of 56.49% in the population aged 65 and older, which was significantly greater than that in the population younger than 65 years. According to the U.S. Census Bureau, by 2030, one-fifth of U.S. adults will be aged 65 or older [31], and arthritis prevalence is expected to continue to increase. Hootman et al. reported that between 2010 and 2012, 52.5 million adults (22.7% of all adults) had doctor-diagnosed arthritis. P rojections indicate that by 2040, the number of U.S. adults with doctor-diagnosed arthritis will reach 78.4 million (25.9% of all adults) [11]. Our study revealed that in 2011–12, the prevalence of arthritis among U.S. adults was approximately 22.98%, which is consistent with previous estimates. However, by 2013–14, the prevalence had exceeded the 25.9% predicted by Hootman et al., reaching 26.54%. This further substantiates the ongoing trend of increasing arthritis prevalence in the future.
OA is the most prevalent joint disease in developed countries and primarily impacts the knee or hip joints [32,33,34]. The etiology of OA is diverse, stemming from the combined effects of various factors [32, 35]. Research on different races revealed that in the U.S., the prevalence of OA is notably high among W hite individuals, reaching 18.63%, while Asians exhibit a lower rate of 5.53%. When considering the non-modifiable factors of OA, age and sex were considered to be the strongest predictors. Specifically, females are more susceptible to OA than males [35,36,37], a finding substantiated in our study (males: 11.14%, females: 18.42%). The influence of age may closely correlate with changes in joint biomechanics [33]. In our investigation, the prevalence of OA in the 20- to 34-year-old age group in 2017–18 was 0.99%, which significantly increased to 35.12% in the 65- to 80-year-old age group. Furthermore, obesity is considered a highly influential modifiable risk factor for the development of OA [32, 38]. A meta-analysis revealed that the likelihood of knee OA in individuals classified as obese or overweight is nearly three times greater than that in individuals with normal body weight [38]. In terms of geographical prevalence, the rate we observed, at 14.93%, is consistent with the range reported across Europe, which spans from 10 to 17% [39]. It also closely matches the prevalence found in prior research conducted in the United States, at 13.9% [34]. However, when compared to South America, our figure is considerably higher, given that estimates there are significantly lower, ranging from 2 to 4% [39]. Additionally, our observed rate is notably lower than those in Asian, African, and Middle Eastern regions, where the prevalence is reported to be higher, specifically within the ranges of 16–23% [39], 17–25% [39], and 17–29% [40, 41], respectively. We observed a 24.21% increase in OA prevalence from 2011 to 2018, further confirming existing epidemiological evidence indicating a rising trend in OA prevalence [10, 42]. The increase in OA prevalence may reflect population aging, an increase in factors contributing to OA risk, and heightened awareness of OA.
RA is an autoimmune disease characterized by joint inflammation and the potential for destructive bone erosion [43], affecting approximately 1% of the global population [44, 45]. RA is considered a multifactorial disease influenced by various genetic and environmental factors [46, 47], contributing to variations in prevalence both between and within countries [48]. Among RA patients, the prevalence of work-related disabilities related to RA is estimated to be approximately 35% [49]. Multiple studies on the trends in RA incidence in the U.S. have reported inconsistent results [2, 13]. Approximately 1.3 million American adults, constituting 0.6–1% of the adult population, are affected by RA [34, 50]. However, our research revealed that the prevalence of RA ranged from 3.84% to 4.61% between 2011 and 2018. Park et al. reported a decreasing trend in the incidence of RA among American adults from 1999 to 2014 [2], while Hunter et al. argued that during the same period, the incidence of RA in the U.S. seemed to increase [13]. In addition, these studies only evaluated the trend of RA before 2014, and the subsequent trends are still unknown. The most recent study based on the NHANES reported the prevalence of RA for the years 2017–18, revealing an increase in the incidence among males and a decrease among females [51], a trend validated by our research. Regarding race, the results showed an increasing trend in prevalence among the other Hispanic (P for trend < 0.001), Asian (P for trend = 0.001), and other racial groups (P for trend = 0.023).
PsA is a chronic inflammatory musculoskeletal disease that is usually negative for rheumatoid factors in the blood and is associated with psoriasis. The general population’s prevalence ranges from 0.02% to 0.42%, with 13.8–30% among psoriasis patients [52]. Global PsA prevalence studies encompass multiple countries, estimating that the prevalence in the U.S. is between 0.06% and 0.25%, while Sweden and Norway exhibit rates ranging from 0.02% to 0.67% [53, 54]. Reports on PsA prevalence in South America and Asia are limited, suggesting lower rates in these regions (e.g., China at 0.02%) [55, 56]. While research on the prevalence of PsA in the general population is relatively limited, a recent meta-analysis incorporating 28 studies indicated a global prevalence of approximately 0.13% [57]. Our study estimates that the prevalence of PsA among U.S. adults in 2017–18 was approximately 0.39%, surpassing the global average. The occurrence of this phenomenon can be attributed to several factors: firstly, racial/ethnic differences, with the prevalence rate of the disease typically being higher in non-Hispanic Whites than in Blacks [58]; secondly, geographical disparities, with the prevalence rate often being lower in regions with abundant sunshine [59]; and lastly, differences in the methods of diagnosis and reporting, which can also influence the statistical reporting of prevalence rates [60].
Furthermore, other arthritis in the study may include joint diseases with low prevalence, such as reactive arthritis, Kaschin-Beck disease, or hemophiliac arthritis. The results indicate a recent increase in the incidence of these types of arthritis (P for trend = 0.001), predominantly observed in White individuals and other races, as well as among individuals aged 35 to 50 years and 65 to 80 years . Due to the lack of specific subgrou** for these types of arthritis in our study, the exact prevalence rates remain unknown. Further research is needed to elucidate the epidemiological patterns of these patients with low-prevalence arthritis conditions .
Strengths and limitations
A major strength of this study lies in the utilization of NHANES data, which provides an opportunity to assess the nationwide prevalence and trends of arthritis, including OA, RA, PsA, and other forms of arthritis. Additionally, our study employs a sufficiently large sample size, allowing for differentiation among non-Hispanic Asians and other racial groups, thereby revealing a distinctive pattern of arthritis prevalence among Asian Americans—a pattern that has been overlooked in prior research.
Similarly, this study has several limitations. First, we relied on self-reported physician-diagnosed arthritis data, introducing the possibility of participant recall and self-reporting biases. Second, although the NHANES remains a leading national survey with a relatively high response rate, similar to many other national face-to-face surveys [61], response rates have gradually declined over time, potentially introducing selection bias. However, the NCHS has addressed this issue by employing enhanced weighting adjustments for NHANES data to minimize potential nonresponse bias. Finally, the NHANES lacks information on other risk factors for arthritis, limiting our ability to fully assess their impact on prevalence.
Conclusions
This nationally representative survey provides robust data for understanding the significant trends in arthritis prevalence among U.S. adults. From 2011 to 2018, we observed variations in arthritis prevalence trends among different races. Across all indicators, rates were higher among White, Black, and other racial groups , with Black individuals showing a relatively stable prevalence without a statistically significant increase over the years. Additionally, we found that the prevalence of arthritis and RA increased only in the Asian population. This discovery contributes to a deeper understanding of the disparities in arthritis prevalence among different populations.
Data availability
Publicly available datasets were analyzed in this study. All data generated or analyzed during this study are included in this published article and the NHANES website (https://www.cdc.gov/nchs/nhanes/index.htm).
References
Ma L, Cranney A, Holroyd-Leduc JM. Acute monoarthritis: what is the cause of my patient’s painful swollen joint? CMAJ Can Med Assoc. J J Assoc Medicale Can. 2009;180:59–65.
Park J, Mendy A, Vieira ER. Various types of arthritis in the United States: prevalence and age-related trends from 1999 to 2014. Am J Public Health. 2018;108:256–8.
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376:957–70.
March LM, Brooks PM. Arthritis: the hidden disability. Med J Aust. 1993;158:369–71.
Schofield D, Cunich M, Shrestha RN, Tanton R, Veerman L, Kelly S, et al. The long-term economic impacts of arthritis through lost productive life years: results from an Australian microsimulation model. BMC Public Health. 2018;18:654.
Safiri S, Kolahi AA, Hoy D, Smith E, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis. 2019;78:1463–71.
van Onna M, Boonen A. The challenging interplay between rheumatoid arthritis, ageing and comorbidities. BMC Musculoskelet Disord. 2016;17:184.
Long H, Liu Q, Yin H, Wang K, Diao N, Zhang Y, et al. Prevalence trends of Site-Specific Osteoarthritis from 1990 to 2019: findings from the global burden of Disease Study 2019. Arthritis Rheumatol Hoboken NJ. 2022;74:1172–83.
Hunter DJ, Schofield D, Callander E. The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol. 2014;10:437–41.
Safiri S, Kolahi A-A, Smith E, Hill C, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of Disease Study 2017. Ann Rheum Dis. 2020;79:819–28.
Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015–2040. Arthritis Rheumatol Hoboken NJ. 2016;68:1582–7.
Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol. 2006;33:2271–9.
Hunter TM, Boytsov NN, Zhang X, Schroeder K, Michaud K, Araujo AB. Prevalence of rheumatoid arthritis in the United States adult population in healthcare claims databases, 2004–2014. Rheumatol Int. 2017;37:1551–7.
Gelfand JM, Gladman DD, Mease PJ, Smith N, Margolis DJ, Nijsten T et al. Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol. 2005;53:573.e1-573.e13.
Wilson FC, Icen M, Crowson CS, McEvoy MT, Gabriel SE, Kremers HM. Time trends in epidemiology and characteristics of psoriatic arthritis over three decades. J Rheumatol. 2009;36:361–7.
Paulose-Ram R, Burt V, Broitman L, Ahluwalia N. Overview of Asian American Data Collection, Release, and analysis: National Health and Nutrition Examination Survey 2011–2018. Am J Public Health. 2017;107:916–21.
US Census Bureau. 2017 National Population Projections Tables: Main Series-Projections for the United States: 2017 to 2060. 2020.
Budiman A, Ruiz NG. Asian Americans are the fastest-growing racial or ethnic group in the U.S. 2021.
Kanaya AM, Hsing AW, Panapasa SV, Kandula NR, Araneta MRG, Shimbo D, et al. Knowledge gaps, challenges, and opportunities in Health and Prevention Research for Asian americans, native hawaiians, and Pacific islanders: a Report from the 2021 National Institutes of Health Workshop. Ann Intern Med. 2022;175:574–89.
Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES Dietary data: focus on collection, release, analytical considerations, and uses to inform Public Policy. Adv Nutr Bethesda Md. 2016;7:121–34.
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital Health Stat Ser 1 Programs Collect Proced. 2013;:1–37.
Fakhouri THI, Martin CB, Chen T-C, Akinbami LJ, Ogden CL, Paulose-Ram R et al. An investigation of nonresponse bias and survey location variability in the 2017–2018 national health and nutrition examination survey. Vital Health Stat 2. 2020;:1–36.
National Center for Health Statistics. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011–2014 and 2015–2016. 2018. https://wwwn.cdc.gov/nchs/data/nhanes/analyticguidelines/11-16-analytic-guidelines.pdf.
Chen T-C, Clark J, Riddles MK, Mohadjer LK, Fakhouri THI. National Health and Nutrition Examination Survey, 2015–2018: Sample Design and Estimation procedures. Vital Health Stat 2. 2020;:1–35.
Centers for Disease Control and Prevention (CDC). Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation–United States, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;62:869–73.
Barbour KE, Helmick CG, Boring M, Zhang X, Lu H, Holt JB. Prevalence of doctor-diagnosed arthritis at state and county levels - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:489–94.
Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults–United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–6.
Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56:1397–407.
Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: Prevalence of Doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2013–2015. Morb Mortal Wkly Rep. 2017;66:246–53.
Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54:226–9.
Colby SL, Ortman JM. Projections of the size and composition of the US population: 2014 to 2060. Population estimates and projections. Current population reports. US Census Bur. 2015;9:25–1143.
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99.
Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2013;39:1–19.
Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35.
Chaganti RK, Lane NE. Risk factors for incident osteoarthritis of the hip and knee. Curr Rev Musculoskelet Med. 2011;4:99–104.
Maleki-Fischbach M, Jordan JM. New developments in osteoarthritis. Sex differences in magnetic resonance imaging-based biomarkers and in those of joint metabolism. Arthritis Res Ther. 2010;12:212.
Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–81.
Blagojevic M, **ks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18:24–33.
Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587.
Al-Awadhi A, Olusi S, Moussa M, Al-Zaid N, Shehab D, Al-Herz A et al. Validation of the Arabic version of the WHO-ILAR COPCORD Core Questionnaire for community screening of rheumatic diseases in Kuwaitis. World Health Organization. International League Against Rheumatism. Community Oriented Program for the Control of Rheumatic Diseases. J Rheumatol. 2002;29:1754–9.
Davatchi F, Jamshidi A-R, Banihashemi AT, Gholami J, Forouzanfar MH, Akhlaghi M, et al. WHO-ILAR COPCORD Study (Stage 1, Urban Study) in Iran. J Rheumatol. 2008;35:1384.
Swain S, Sarmanova A, Mallen C, Kuo CF, Coupland C, Doherty M, et al. Trends in incidence and prevalence of osteoarthritis in the United Kingdom: findings from the Clinical Practice Research Datalink (CPRD). Osteoarthritis Cartilage. 2020;28:792–801.
Shapira Y, Agmon-Levin N, Shoenfeld Y. Geoepidemiology of autoimmune rheumatic diseases. Nat Rev Rheumatol. 2010;6:468–76.
Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. JAMA. 2018;320:1360–72.
GBD 2021 Rheumatoid Arthritis Collaborators. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: a systematic analysis of the global burden of Disease Study 2021. Lancet Rheumatol. 2023;5:e594–610.
Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, et al. Rheumatoid arthritis. Nat Rev Dis Primer. 2018;4:18001.
Liao KP, Alfredsson L, Karlson EW. Environmental influences on risk for rheumatoid arthritis. Curr Opin Rheumatol. 2009;21:279–83.
Tobón GJ, Youinou P, Saraux A. The environment, geo-epidemiology, and autoimmune disease: rheumatoid arthritis. J Autoimmun. 2010;35:10–4.
Allaire S, Wolfe F, Niu J, Lavalley MP. Contemporary prevalence and incidence of work disability associated with rheumatoid arthritis in the US. Arthritis Rheum. 2008;59:474–80.
Cross M, Smith E, Hoy D, Carmona L, Wolfe F, Vos T, et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1316–22.
Xu Y, Wu Q. Prevalence Trend and disparities in Rheumatoid Arthritis among US adults, 2005–2018. J Clin Med. 2021;10:3289.
Gladman DD. Psoriatic arthritis. Dermatol Ther. 2009;22:40–55.
Hoff M, Gulati AM, Romundstad PR, Kavanaugh A, Haugeberg G. Prevalence and incidence rates of psoriatic arthritis in central Norway: data from the Nord-Trøndelag health study (HUNT). Ann Rheum Dis. 2015;74:60–4.
Löfvendahl S, Theander E, Svensson Å, Carlsson KS, Englund M, Petersson IF. Validity of diagnostic codes and prevalence of physician-diagnosed psoriasis and psoriatic arthritis in southern Sweden–a population-based register study. PLoS ONE. 2014;9:e98024.
Soriano ER, Rosa J, Velozo E, Schpilberg M, Imamura PM, Diaz J, et al. Incidence and prevalence of psoriatic arthritis in Buenos Aires, Argentina: a 6-year health management organization-based study. Rheumatol Oxf Engl. 2011;50:729–34.
Li R, Sun J, Ren L-M, Wang H-Y, Liu W-H, Zhang X-W, et al. Epidemiology of eight common rheumatic diseases in China: a large-scale cross-sectional survey in Bei**g. Rheumatol Oxf Engl. 2012;51:721–9.
Scotti L, Franchi M, Marchesoni A, Corrao G. Prevalence and incidence of psoriatic arthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2018;48:28–34.
Gordon N, Kaiser Permanente Division of Research. Internal Division of Research report. Oakland, CA: ; 2012. Similarity of the adult kaiser permanente membership in northern California to the insured and general population in northern California: statistics from the 2009 California Health Interview Survey. 2014.
Chandran V, Raychaudhuri SP. Geoepidemiology and environmental factors of psoriasis and psoriatic arthritis. J Autoimmun. 2010;34:J314–321.
Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Identification and management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377–85.
Williams D, Brick JM. Trends in U.S. Face-To-Face Household Survey Nonresponse and Level of Effort. J Surv Stat Methodol. 2018;6:186–211.
Acknowledgements
Not applicable.
Funding
This work was supported by the Key Project of the National Natural Science Foundation of China (U21A20390), Jilin Province Development and Reform Commission (2023C039-3), Jilin Scientific and Technological Development Program (20230203089SF) and Graduate Innovation Program of Jilin University (2024CX142) .
Author information
Authors and Affiliations
Contributions
YGQ, JLX and XFT concepted and designed the study. SHX and YQS collected data. SHX, XYS and BC analyzed and interpreted the data. SHX edited the manuscript. YGQ, JLX and XFT revised the manuscript for important intellectual content.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocols of NHANES were approved by the institutional review board of the National Center for Health Statistics, CDC (https://www.cdc.gov/nchs/nhanes/irba98.htm). NHANES has obtained written informed consent from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, S., Shen, X., Chen, B. et al. Trends in prevalence of arthritis by race among adults in the United States, 2011–2018. BMC Public Health 24, 1507 (2024). https://doi.org/10.1186/s12889-024-18966-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18966-0