Abstract
Background
Acute gastroenteritis (AGE) causes significant morbidity in children worldwide; however, the disease burden of children hospitalized with viral gastroenteritis in China has been rarely described. Through this study, we analyzed the data of hospitalized children with viral gastroenteritis to explore the changes in the epidemiology and clinical characteristics of viral gastroenteritis in the mainland of China.
Methods
Data were extracted from Futang Children's Medical Development Research Center (FRCPD), between 2016 and 2020, across 27 hospitals in 7 regions. The demographics, geographic distribution, pathogenic examination results, complications, hospital admission date, length of hospital stays, hospitalization charges and outcomes were collected and analyzed.
Results
Viral etiological agents included rotavirus (RV), adenovirus (ADV), norovirus (NV) and coxsackievirus (CV) that were detected in 25,274 (89.6%), 1,047 (3.7%), 441 (1.5%) and 83 (0.3%) cases. There was a higher prevalence of RV and NV infection among children younger than 3 years of age. RV and NV had the highest detection rates in winter, while ADV in summer. Children with viral gastroenteritis were often accompanied by other diseases, such as myocardial diseases (10.98–31.04%), upper respiratory tract diseases (1.20–20.15%), and seizures (2.41–14.51%). Among those cases, the co-infection rate with other pathogens was 6.28%, with Mycoplasma pneumoniae (M. pneumoniae), Epstein-Barr virus (EBV), and influenza virus (FLU) being the most common pathogens. The median length of stay was 5 days, and the median cost of hospitalization corresponded to587 US dollars.
Conclusions
This finding suggests that viral gastroenteritis, especially those caused by RV, is a prevalent illness among younger children. Co-infections and the presence of other diseases are common. The seasonality and regional variation of viral etiological agents highlight the need for targeted prevention and control measures. Although viral gastroenteritis rarely leads to death, it also results in a significant economic burden on healthcare systems.
Similar content being viewed by others
Background
Acute gastroenteritis is a common disease that affects people of all ages, leading to serious complications in young children and the elderly [1,2,3,4]. In China, infectious diarrhea (excluding cholera, dysentery and enteric fever) has been classified as a class C infectious disease according to the national notifiable infectious diseases reporting system. Enteric viral pathogens are gradually becoming the leading pathogens of gastroenteritis which is also known as infectious diarrhea, due to the improved the quality of drinking water and the frequent use of antibiotics. Clinical manifestations of viral gastroenteritis include fever, abdominal pain, watery diarrhea, nausea and vomiting. Viral gastroenteritis is usually a self-limiting illness, requiring mainly supportive therapy, which usually resolves within 2–5 days. Viral pathogens include rotavirus (RV), norovirus (NV), astrovirus (AV) and adenovirus (ADV). NV infection affects people of all ages, while RV mainly infects children, particularly those under five years of age [5,6,7,8].
The implementation of RV vaccination has reduced RV problems to some extent, but the contribution of RV to pediatric acute gastroenteritis has not been replaced by other pathogens [3, 6, 9]. Vaccination has helped to reduce RV hospitalization, as well as change the epidemiology of RV disease in the United States and Spain [10, 11]. RV vaccine is part of the National Immunization Programs (NIPs) in many countries, but it has not been included in China’s NIPs. The epidemiology and distribution of common pathogens causing infectious gastroenteritis, particularly viruses, are unclear in develo** countries including China.
In China, there are few multicenter studies on the clinical epidemiological characteristics and disease burden of viral gastroenteritis in children. By using the hospitals’ electronic medical record management system, the medical data generated during the hospitalization of patients can be summarized into face sheet of discharge medical records (FSMRs). This study aimed to summarize and provide relevant data on the clinical epidemiology and disease burden of viral gastroenteritis in hospitalized children in China.
Methods
Study design and participants
In China, Futang Children's Medical Development Research Center (FRCPD) is the first non-profit social service organization established to care for children's lives and health and engage in children’s development research [12], supervised and managed by the Ministry of Civil Affairs of the People’s Republic of China and led by the Children’s Medical Center. The center currently consists of 47 provincial and municipal medical institutions and has established a nationwide children health service network [13]. In Dec 2015, FRCPD began to collect the data of FSMRs from its member hospitals. The National Center for Children's Health (Bei**g), Bei**g Children’s Hospital, Capital Medical University collected the data of the hospitalized children’s medical records from Jan 1st, 2016 to Dec 31st, 2020 in 27 tertiary children's hospitals under the FRCDP (Supplementary Material 1).
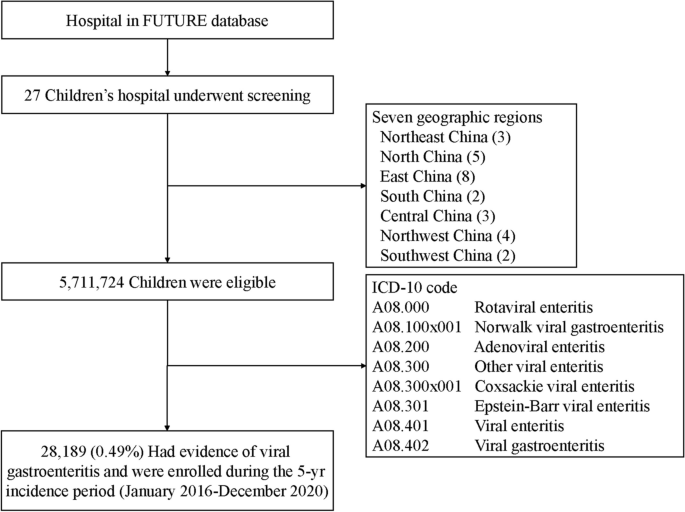
We designed this study to collect basic medical information of children hospitalized with viral gastroenteritis in the FUTang Updating medical REcords (FUTURE) database from 2016 to 2020, and extracted relevant information from the system based on the tenth revision of the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) code for children diagnosed with viral gastroenteritis (Fig. 1). The demographic information isdisplayed in Table 1. Subgroups were divided according to the sex, age, region, and time of hospitalization status. All hospitals were divided into seven geographic regions. According to different ages, hospitalized children with viral gastroenteritis were divided into six groups, including neonate (≤ 28 days), infant (28 days < ~ ≤ 1 year old, neonate were excluded), toddler (1 < ~ ≤ 3 years old), preschooler (3 < ~ ≤ 6 years old), school–age children (6 < ~ ≤ 12 years old), adolescence (12 < ~ < 18 years old).
Inclusion and exclusion criteria
This retrospective study included only children under the age of 18 who were hospitalized for viral gastroenteritis based on the classification of viral gastroenteritis according to ICD-10 codes, we collected basic medical information from the FUTURE database. Children were diagnosed with viral gastroenteritis according to the clinical and etiological diagnosis [3, 4]. Data of children with unknown sex, age, region or resident condition were excluded.
Statistical analysis
Continuous variables were presented as mean ± standard deviation (SD) and compared between groups by Student’s t-test when normally distributed. For not normally distributed variables, the data were expressed as median (interquartile range, IQR), and Kruskal–Wallis test as well as Steel–Dwass test (for multiple comparisons) were performed to compare the difference among groups. Categorical variables were expressed as number (%) or proportions and compared between/among groups by χ2 or Fisher’s exact tests, when appropriate. IBM SPSS Statistics 23.0 software (SPSS Inc., USA) was used for data analysis. P value < 0.05 was considered statistically significant.
Results
Prevalence of viral gastroenteritis in children
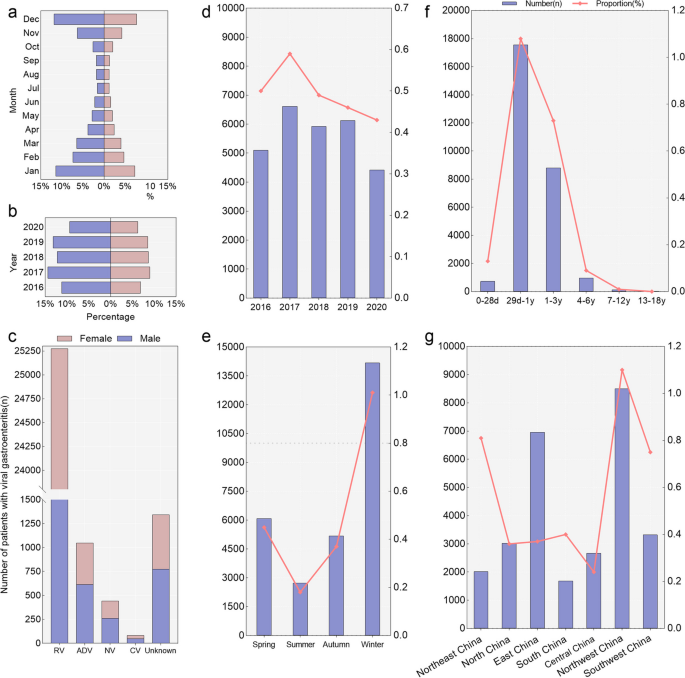
During 2016–2020, a total of 28,189 hospitalized children with viral gastroenteritis were enrolled in the FUTang Updating medical Records (FUTURE) database, which accounted for 0.5% (28,189/5,711,724) of all hospitalized cases, with 60.6% male (17,099) and 39.3% female (11,096) (Table 1). In different month and admission years, the proportions of male were higher compared to female (Fig. 2). The information on sex, age, year, season, regions and outcomes is shown in Table 1.
The proportion of children hospitalized for viral gastroenteritis by different gender, years, ages and regions. Panel a-c show the proportion of different years, months and pathogens according to gender. Panel d-g show the number and proportion in different years, age groups, seasons and regions of China, the left Y axis (the bars) is the number, while the right Y axis (the line plots) is the proportion of hospitalized children with viral gastroenteritis. The definition of "unknown" is that children with viral gastroenteritis were for an unspecified viral cause
In different genders, years, regions, and age groups, we evaluated the proportion of viral gastroenteritis hospitalizations to total hospitalization (Table 1, Fig. 2). Females had a higher proportion of children with viral gastroenteritis than males (P < 0.001), with the rates of 0.5% (11,090/2,179,388) and 0.5% (17,099/3,532,336), respectively (Table 1). The rate of viral gastroenteritis in the age group from 29 days to 1 year old was significantly higher than those in other age groups (Table 1) (P < 0.001). The proportion of viral gastroenteritis hospitalizations to total hospitalization also differed with seasonal variability, which was higher in winter and lower in summer (Table 1) (P < 0.001). Northwest China had the highest proportion (1.1%, 8,505/775,561) and Central China had the lowest proportion (0.2%, 2,671/1,098,999) (P < 0.001).
Viral gastroenteritis characterized by different viral pathogens
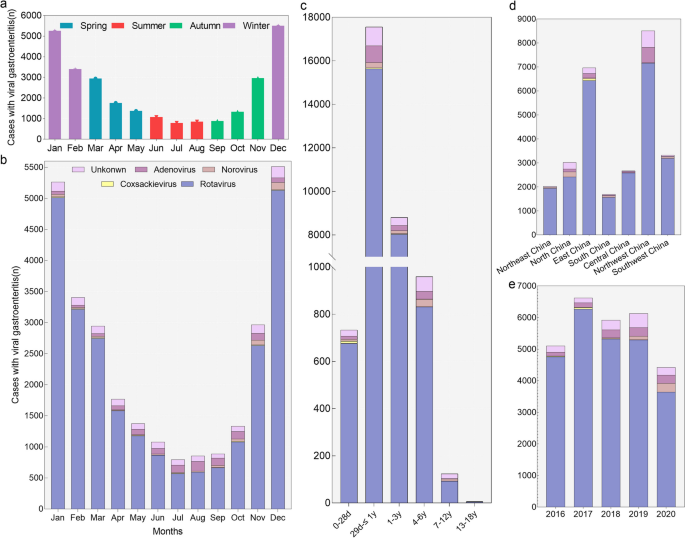
Among those admitted to the hospital with a diagnosis of viral gastroenteritis, 95.2% (26,845/28,189) cases were positive for viral infection (RV, NV, CV and ADV) (Table 2, Fig. 3). RV had the highest positive proportion (89.7%) than the other viruses (P < 0.001). RV, NV, CV and ADV had the highest positive rate in the 28 days < ~ ≤ 1 year group than other age groups (P < 0.001). RV and NV had the highest detection rate in winter compared with other seasons, while ADV had the highest detection rate in summer (P < 0.001). RV showed high detection rates in Northwest China and East China (28.3% and 25.4%), while NV had a high detection rate in North China, CV in East China and ADV in Northwest China (46.9%, 94.0% and 61.5%) compared to other regions (P < 0.001) (Table 2).
Pathogens detected in children with viral gastroenteritis requiring hospitalization. Panel a show the number of hospitalized children with viral gastroenteritis in different seasons. Panel b show the pathogens distribution in different months. Seasons were based on months as follows: winter, January through March; spring, April through June; summer, July through September; fall, October through December. Panel c-e show the pathogens distribution in in different age groups, years and regions of China. The definition of "unknown" is that children with viral gastroenteritis were for an unspecified viral cause
Viral gastroenteritis combined with other diseases
Children hospitalized with viral gastroenteritis were often presented with one or more coexisting diseases. Among the 25,274 cases of RV-positive children, they had various other diseases. Specifically, 31.04% had myocardial diseases, 14.41% had upper respiratory tract diseases, 11.83% had bronchitis, and 6.92% had bronchopneumonia. Meantime, myocardial diseases and upper respiratory tract diseases are also common in children infected with CV, NV and ADV (Table 3). Among positive cases of CV (23 cases), RV (7845 cases), NV (75 cases), and ADV (115 cases) with myocardial diseases, myocardial injury rates were highest for cases of myocardial impairment, with 100.00% (23 cases), 78.88% (6188 cases), 95.0% (72 cases), and 73.04% (84 cases), respectively. Nervous system diseases such as seizure accounted for 14.51% of children with NV, 6.02% with ADV, 5.60% with RV and 2.41% with CV. Among RV-positive children with seizures, there were 14 cases of febrile seizures (0.99%), 31 cases of benign convulsions with gastroenteritis (2.19%), and 218 cases of benign infantile convulsions (15.41%). Moreover, other diseases were relatively low, such as urogenital diseases, and nutritional diseases (Table 3).
Coinfection with other pathogens
For 26,845 viral gastroenteritis cases with RV, CV, NV or ADV, the co-infection rate was 6.28% (1686/26845): viruses in 792 (2.95%), bacteria in 176 (0.66%), fungi and atypical pathogens in 718 (2.67%). The most commonly co-infection pathogens were Mycoplasma pneumoniae (M. pneumoniae) (1.95%, 523 cases), Epstein-Barr virus (EBV) (0.98%, 262 cases), influenza virus (FLU) (0.67%, 181 cases), cytomegalovirus (CMV) (0.53%, 141 cases), candida albicans (C. albicans) (0.48%, 129 cases), and respiratory syncytial virus (RSV) (0.41%, 110 cases) (Table 4). M. pneumoniae was detected more commonly in viral gastroenteritis children infected with RV or NV than with CV or ADV (2.01–2.27% vs. 0–0.57%). EBV (1.00%, 253/25274) and RSV (0.42%, 107/25274) were more commonly co-infected with RV in children with viral gastroenteritis, while CMV more commonly with CV (1.20%, 1/83) and FLU with NV (0.91%, 4/441) (Table 4).
Complications
Complications of viral gastroenteritis included dehydration, acidosis, electrolyte disorders and shock (Table 5). Children aged 28 days < ~ ≤ 1 year were most likely to suffer from acidosis, while those aged 6 < ~ ≤ 12 years old were most likely to suffer from dehydration (P < 0.001). Dehydration was more common in children with NV infection, while electrolyte disturbances were more prevalent in children with RV infection, and acidosis with ADV infection (P < 0.001).
LOS, hospitalization expense, discharge and outcome
The median length of stay (LOS) for hospitalized viral gastroenteritis patients was 5 days (IQR: 3–6 days), and the median expense was 587 USD (541–642 USD) (Table 6). The LOS was shortest for children aged 1 < ~ ≤ 3 years and longest for children aged 28 days < ~ ≤ 1 year. Total costs were highest among hospitalized patients aged ≤ 28 days(P < 0.001). Children with RV gastroenteritis had the longest LOS (P < 0.001). The hospital cost was the highest with ADV gastroenteritis (642 US$) and lowest with RV gastroenteritis (541 US$). The majority of hospitalized patients recovered and were able to be discharged within a few days, in which the percentage of discharge by patient with medical advice was 93.5% (26,363 cases) (Table 1). Fortunately, there were no deaths in our study.
Discussion
This study summarized and analyzed the FSMRs data of 28,189 hospitalized children with viral gastroenteritis from 2016 to 2020 in the mainland of China to provide further evidence for the role of gastrointestinal viral infections in this most common gastrointestinal emergency in children. We found that the burden of viral gastroenteritis related hospitalization was the highest among children younger than 3 years of age. RV, CV, ADV and NV accounted for 95.2% of the children with viral gastroenteritis. We demonstrated that the coexistence rates of viral gastroenteritis with upper respiratory tract diseases, myocardial diseases, or seizure were high, and the co-occurrence of other viral, bacterial or atypical pathogen infections was common in pediatric patients hospitalized with viral gastroenteritis, such as M. pneumoniae, EBV and CMV.
Children with viral gastroenteritis under 18 years of age have a ratio of 1.54 to1 between males and females. The result coincided with previous research in China, which showed the ratio was 1.68:1 for children under 5 years of age with gastroenteritis in western China from 2015 to 2019 [14]. Our data suggests that children bearing the greatest burden of hospitalization associated with AGE especially infected with RV were children younger than 3 years (96.3%). In comparison with other studies worldwide [15,16,17], there is a significant difference in the detection rate of rotavirus and norovirus. This may be attributed to the involvement of multiple hospitals in this study, each of which adopted different diagnostic methods. Additionally, RV infection often results in fever, vomiting, dehydration, and severe diarrhea compared to NV infection, increasing the likelihood of hospitalization [18,19,31]. Advancements in the medical infectious disease reporting system, pathogen detection technology, and awareness about sending specimens for testing for pathogens have resulted in the detection of more positive cases. The first-dose RV vaccine coverage in China was 20.3%, with only 1.8% coverage for the third dose; consequently, despite a decrease in hospitalization and mortality rates for RVGE in China, the disease burden persists [32].
Viral gastroenteritis combined with myocardial diseases refers to the condition where viral infection leads to myocardial damage and myocarditis [33, 34]. In this study, the proportion of viral gastroenteritis combined with myocarditis was high, ranging from 10.98% to 31.04%, in which over 70% of cases were diagnosed with myocardial injuries. Cioc et al. revealed that among 13 cases of sudden cardiac arrest patients, 5 cases of CV and 4 cases of RV in myocardial tissue samples, and a number of case reports have described especially myocarditis of RV infection [35, 36]. Viral gastroenteritis can also be associated with central nervous system (CNS) diseases, known as encephalitis or meningitis. This study found that the proportion of cases with seizures was from 2.41–14.51%, in which benign infantile convulsions had the highest proportion, and benign convulsions with gastroenteritis only accounted for 0–21.88% of cases with seizures, similar to other reports [37,38,39]. There have been numerous cases with respiratory diseases, including 60 cases (6.59%) of ADV-associated pneumonia and bronchopneumonia. According to previous studies, ADV is more commonly cause gastrointestinal diseases by serotypes 40 or 41 [40, 41]. Therefore, for children hospitalized with viral gastroenteritis, we should pay attention to the possibility of concurrent other systemic diseases and remain vigilant for the occurrence of severe cases.
In terms of the co-infection with other pathogens, M. pneumoniae, EBV, FLU, and CMV were the main pathogens of viral gastroenteritis in hospitalized children. M. pneumoniae and FLU infections usually cause respiratory diseases, such as Mycoplasma pneumoniae pneumonia and viral pneumonia, which aligned with the high proportion of respiratory diseases among children with viral gastroenteritis that were mentioned earlier. In this study EBV-positive cases included infectious mononucleosis, EBV viremia, and other EBV-related diseases. It is important to note that a positive result does not necessarily indicate that EBV infection will result in disease or symptoms, because most patients may have latent EBV infection [42]. Similar to EBV, CMV is typically asymptomatic in the majority of individuals. However, in children with compromised immune function who are hospitalized with viral gastroenteritis, CMV infection can cause clinical symptoms and complications, such as hepatitis, pneumonia, and impairment of the brain and visual system. For children with viral gastroenteritis, properly controlling infections caused by other pathogens is crucial to immunocompromised patients, including immune deficiencies, hematopoietic stem cell transplantation or liver transplantation [43, 44].
AGE is generally a self-limiting condition and resolves within one week, which is most commonly associated with viral infection [45,46,47]. There were no fatal cases in our study, as a result of viral gastroenteritis, patients usually suffered from complications, such as dehydration, electrolyte disorders, and acidosis. Our study showed there was more dehydration in children with NV infections, electrolyte disturbances in children with RV infections, and electrolyte disorders with ADV infections. LOS and hospitalization expense of children with viral gastroenteritis were associated with age, region and pathogens in children.
Our study has some limitations. The most frequently seen patients with viral gastroenteritis are outpatients, while our database only contains the data generated from hospitalized children, so little is known regarding the total incidence of viral gastroenteritis. Meanwhile, various detection methods for pathogens in different hospitals lead to the effectiveness of the detection method for the same pathogen is diverse, so we are unable to make comparisons between different pathogens. In this study, no follow-up information was available for the children with viral gastroenteritis, especially patients who had been transferred to other hospitals. Due to a lack of clear information regarding the patient's RV vaccination status, it is hard to assess the protective effect of RV vaccination in viral gastroenteritis.
Conclusion
Rotavirus was detected in nearly 90% of children with viral gastroenteritis among hospitalized children in the mainland of China. Most cases occurred among children younger 3 years during the winter months. Children with viral gastroenteritis were often accompanied by other diseases and pathogens, with myocardial diseases the most common disease and M. pneumoniae the most common pathogen. Continuous surveillance is needed to monitor the prevalence of viral gastroenteritis, and the immunization schedule of rotavirus is essential for adequate management of viral gastroenteritis.
Availability of data and materials
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AGE:
-
Acute gastroenteritis
- FRCPD:
-
Futang Children's Medical Development Research Center
- RV:
-
Rotavirus
- NV:
-
Norovirus
- ADV:
-
Adenovirus
- CV:
-
Coxsackievirus
- EV:
-
Enterovirus
- M. pneumoniae :
-
Mycoplasma pneumoniae
- EBV:
-
Epstein-Barr virus
- FLU:
-
Influenza virus
- AV:
-
Astrovirus
- NIPs:
-
National Immunization Programs
- FSMRs:
-
Face sheet of discharge medical records
- ICD-10:
-
International Statistical Classification of Diseases and Related Health Problems 10th Revision
- IQR:
-
Interquartile range
- CMV:
-
Cytomegalovirus
- C. albicans :
-
Candidaalbicans
- RSV:
-
Respiratory syncytial virus
- LOS:
-
Length of stay
- WHO:
-
World Health Organization
- LLR:
-
Lanzhou lamb rotavirus
- RV5:
-
RotaTeq
- LLR3:
-
Lanzhou lamb reassortant rotavirus vaccine, live, oral, trivalent (Vero cell)
- RVGE:
-
Rotavirus gastroenteritis
- CNS:
-
Central nervous system
References
Reiner RC Jr, Graetz N, Casey DC, Troeger C, Garcia GM, Mosser JF, et al. Variation in childhood diarrheal morbidity and mortality in Africa, 2000–2015. N Engl J Med. 2018;379(12):1128–38.
Zhang J, Duan Z, Payne DC, Yen C, Pan X, Chang Z, et al. Rotavirus-specific and overall diarrhea mortality in chinese children younger than 5 years: 2003 to 2012. Pediatr Infect Dis J. 2015;34(10):e233–7.
Meier JL. Viral acute gastroenteritis in special populations. Gastroenterol Clin North Am. 2021;50(2):305–22.
Hartman S, Brown E, Loomis E, Russell HA. Gastroenteritis in children. Am Fam Physician. 2019;99(3):159–65.
Collaborators GDaI. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the global burden of disease study 2016. Lancet Infect Dis. 2018;18(11):1211–28.
Yang L, Shi S, Na C, Li B, Zhao Z, Yang T, et al. Rotavirus and norovirus infections in children under 5 years old with acute gastroenteritis in Southwestern China, 2018–2020. J Epidemiol Glob Health. 2022;12(3):292–303.
Pitkänen O, Markkula J, Hemming-Harlo M. A major decrease in viral acute gastroenteritis in hospitalized finnish children as rotavirus returns as the most detected pathogen. Int J Infect Dis. 2022;114:273–8.
Öner SZ, Kaleli İ, Demi RM, Mete E, Çalişkan A. Rotavirus and adenovirus prevalence in patients with acute viral gastroenteritis in Denizli, Turkey, 2017–2021. J Med Virol. 2022;94(8):3857–62.
Paternina-Caicedo A, Parashar U, Garcia-Calavaro C, de Oliveira LH, Alvis-Guzman N, De la Hoz-Restrepo F. Diarrheal deaths after the introduction of rotavirus vaccination in 4 countries. Pediatrics. 2021;147(1):e20193167.
Burke RM, Tate JE, Han GS, Quenelle R, Gautam R, Wadford DA, et al. Rotavirus vaccination coverage during a rotavirus outbreak resulting in a fatality at a subacute care facility. J Pediatric Infect Dis Soc. 2020;9(3):287–92.
Hallowell BD, Parashar UD, Curns A, DeGroote NP, Tate JE. Trends in the laboratory detection of rotavirus before and after implementation of routine rotavirus vaccination - United States, 2000–2018. MMWR Morb Mortal Wkly Rep. 2019;68(24):539–43.
Feng G, Zeng Y, Tian J, Wang X, Tai J, Song F, et al. Disease spectrum analysis of hospitalized children in China: a study of 18 tertiary children’s hospitals. Pediatr Investig. 2019;3(3):159–64.
Guo K, Wang XY, Feng GS, Tian J, Zeng YP, Ma SX, et al. The epidemiology of blood transfusion in hospitalized children: a national cross-sectional study in China. Transl Pediatr. 2021;10(4):1055–62.
Cao RR, Ma XZ, Li WY, Wang BN, Yang Y, Wang HR, et al. Epidemiology of norovirus gastroenteritis in hospitalized children under five years old in western China, 2015–2019. J Microbiol Immunol Infect. 2021;54(5):918–25.
Amodio E, De Grazia S, Genovese D, Bonura F, Filizzolo C, Collura A, et al. Clinical and epidemiologic features of viral gastroenteritis in hospitalized children: an 11-year surveillance in palermo (Sicily). Viruses. 2022;15(1):41.
Calduch EN, Cattaert T, Verstraeten T. Model estimates of hospitalization discharge rates for norovirus gastroenteritis in Europe, 2004–2015. BMC Infect Dis. 2021;21(1):757.
Aliabadi N, Antoni S, Mwenda JM, Weldegebriel G, Biey JNM, Cheikh D, et al. Global impact of rotavirus vaccine introduction on rotavirus hospitalisations among children under 5 years of age, 2008–16: findings from the global rotavirus surveillance network. Lancet Glob Health. 2019;7(7):e893–903.
Zhang J, Yang F. Correlation between infection with rotavirus and norovirus and acute gastroenteritis in children. Endemic Dis Bull (in Chinese). 2018;33(03):74–6.
Cui X, Feng G, Jln F, Xu X. Investigation and clinical analysis of norovirus and rotavirus infection in 942 children with acute diarrhea. Chin J Practical Pediatr (in Chinese). 2016;31(08):603–7.
Wei K, Liu X, Liu D, Chang Q, **ang J, Wang P. Investigation on the prevalence of group A rotavirus and norovirus in hospitalized children with diarrhea in Wuwei area, Gansu province. Chin J Viral Dis (in Chinese). 2014;4(02):137–40.
Sharma P, Katewa S, Meel SK, Katewa V, Bishnoi A, Verma VK, et al. Clinicoepidemiological profile and genetic characterization of circulating rotavirus strain among children < 5 years hospitalized for acute gastroenteritis in Western Rajasthan. India Indian J Pediatr. 2021;88(Suppl 1):97–104.
Lu W, Li J, Li J, Ai D, Song H, Duan Z, et al. Short-term impacts of meteorology, air pollution, and internet search data on viral diarrhea infection among children in Jilin Province, China. Int J Environ Res Public Health. 2021;18(21):11615.
Nan X, **yuan W, Yan Z, Maosheng S, Hongjun L. Epidemiological and clinical studies of rotavirus-induced diarrhea in China from 1994–2013. Hum Vaccin Immunother. 2014;10(12):3672–80.
Fu C, Dong Z, Shen J, Yang Z, Liao Y, Hu W, et al. Rotavirus gastroenteritis infection among children vaccinated and unvaccinated with rotavirus vaccine in Southern China: a population-based assessment. JAMA Netw Open. 2018;1(4):e181382.
Zhang H, Lai X, Mak J, Sriudomporn S, Zhang H, Fang H, et al. Coverage and equity of childhood vaccines in China. JAMA Netw Open. 2022;5(12):e2246005.
Steens A, Knol MJ, Freudenburg-de Graaf W, de Melker HE, van der Ende A, van Sorge NM. Pathogen- and type-specific changes in invasive bacterial disease epidemiology during the first year of the COVID-19 pandemic in The Netherlands. Microorganisms. 2022;10(5):972.
Lamrani Hanchi A, Guennouni M, Ben Houmich T, Echchakery M, Draiss G, Rada N, et al. Changes in the epidemiology of respiratory pathogens in children during the COVID-19 pandemic. Pathogens. 2022;11(12):1542.
Luciani L, Ninove L, Zandotti C, Nougairède A. COVID-19 pandemic and its consequences disrupt epidemiology of enterovirus meningitis. South-East France J Med Virol. 2021;93(4):1929–31.
Kies KD, Thomas AS, Binnicker MJ, Bashynski KL, Patel R. Decrease in enteroviral meningitis: an unexpected benefit of coronavirus disease 2019 (COVID-19) mitigation? Clin Infect Dis. 2021;73(9):e2807–9.
Burke RM, Shih S, Hsiung CA, Yen C, Jiang B, Parashar UD, et al. Impact of rotavirus vaccination on rotavirus hospitalizations in Taiwanese children. Vaccine. 2021;39(49):7135–9.
Shim JO, Chang JY, Shin S, Moon JS, Ko JS. Changing distribution of age, clinical severity, and genotypes of rotavirus gastroenteritis in hospitalized children after the introduction of vaccination: a single center study in Seoul between 2011 and 2014. BMC Infect Dis. 2016;16:287.
Luo HM, Ran L, Meng L, Lian YY, Wang LP. Analysis of epidemiological characteristics of report cases of rotavirus diarrhea in children under 5 years old in China, 2005–2018. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(2):181–6.
Rauff B, Malik A, Bhatti YA, Chudhary SA, Fatima K, Rafiq S, et al. Association of viruses in the development of cardiovascular diseases. Curr Pharm Des. 2021;27(37):3913–23.
Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020;13(11):e007405.
Dian Z, Sun Y, Zhang G, Xu Y, Fan X, Yang X, et al. Rotavirus-related systemic diseases: clinical manifestation, evidence and pathogenesis. Crit Rev Microbiol. 2021;47(5):580–95.
Cioc AM, Nuovo GJ. Histologic and in situ viral findings in the myocardium in cases of sudden, unexpected death. Mod Pathol. 2002;15(9):914–22.
Ogawa C, Kidokoro H, Ishihara N, Tsuji T, Kurahashi H, Hattori A, et al. Splenial lesions in benign convulsions with gastroenteritis associated with rotavirus infection. Pediatr Neurol. 2020;109:79–84.
Wang D, Jiang Y, Hong S, Ma J, Liao S, Cheng M, et al. Prognostic factors for the recurrence of afebrile seizures after benign convulsions associated with mild gastroenteritis. Epilepsia. 2021;62(12):3068–75.
Hungerford DJ, French N, Iturriza-Gómara M, Read JM, Cunliffe NA, Vivancos R. Reduction in hospitalisations for acute gastroenteritis-associated childhood seizures since introduction of rotavirus vaccination: a time-series and change-point analysis of hospital admissions in England. J Epidemiol Community Health. 2019;73(11):1020–5.
Sdiri-Loulizi K, Gharbi-Khelifi H, de Rougemont A, Hassine M, Chouchane S, Sakly N, et al. Molecular epidemiology of human astrovirus and adenovirus serotypes 40/41 strains related to acute diarrhea in Tunisian children. J Med Virol. 2009;81(11):1895–902.
Dey RS, Ghosh S, Chawla-Sarkar M, Panchalingam S, Nataro JP, Sur D, et al. Circulation of a novel pattern of infections by enteric adenovirus serotype 41 among children below 5 years of age in Kolkata. India J Clin Microbiol. 2011;49(2):500–5.
Cohen JI. Epstein-Barr virus infection. N Engl J Med. 2000;343(7):481–92.
Kohli R, Cortes M, Heaton ND, Dhawan A. Liver transplantation in children: state of the art and future perspectives. Arch Dis Child. 2018;103(2):192–8.
Bateman CM, Kesson A, Powys M, Wong M, Blyth E. Cytomegalovirus Infections in children with primary and secondary immune deficiencies. Viruses. 2021;13(10):2001.
Posovszky C, Buderus S, Classen M, Lawrenz B, Keller KM, Koletzko S. Acute infectious gastroenteritis in infancy and childhood. Dtsch Arztebl Int. 2020;117(37):615–24.
Lee B, Damon CF, Platts-Mills JA. Pediatric acute gastroenteritis associated with adenovirus 40/41 in low-income and middle-income countries. Curr Opin Infect Dis. 2020;33(5):398–403.
Bányai K, Estes MK, Martella V, Parashar UD. Viral gastroenteritis. Lancet. 2018;392(10142):175–86.
Acknowledgements
We are grateful to investigators from members of the Futang Research Center of Pediatric Development (FRCPD).
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82172245 and 81971922); Bei**g Natural Science Foundation (grant number L192014); CAMS Innovation Fund for Medical Sciences (grant number 2019-I2M-5–026); and Bei**g Excellent Talents Training Program (grant number 2018000021469G274).
Author information
Authors and Affiliations
Contributions
XPC and ZDX conceptualized and designed the study, reviewed and revised the final manuscript. FL collected clinical data, analyzed the results, and drafted the initial manuscript. LYG, QL, HX and GSF analyzed the results and provided clinical context for study methods; YLF, LCH, and GL critically contributed to the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the medical ethics committee of the Bei**g Children’s Hospital, Capital Medical University. The ethics committee approved the waiver of informed consent from parents/guardians of the minors, because the present study was a retrospective analysis of clinical data and all methods were performed in accordance with the ethical guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, F., Guo, L., Li, Q. et al. Changes in the epidemiology and clinical characteristics of viral gastroenteritis among hospitalized children in the Mainland of China: a retrospective study from 2016 to 2020. BMC Pediatr 24, 303 (2024). https://doi.org/10.1186/s12887-024-04776-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04776-1