Abstract
Background
Genital warts (GW) are the most common sexually transmitted infections. To date, few studies using a human papillomavirus (HPV)-specific questionnaire have focused on the impact of quality of life (QoL) among patients with GW in develo** countries. The origins of GW related psychosocial burdens and variations between genders were poorly characterized as well.
Methods
A hospital-based survey was conducted in Bei**g and Nan**g of China in 2008. Eligible patients aged 18–65 who had a diagnosis of GW within 3 months were recruited. Demographic information, HPV knowledge, and assessment of psychosocial burden were collected by the HPV Impact Profile (HIP). The HIP examined 7 specific psychosocial domains by 29 items: (1) worries and concerns, (2) emotional impact, (3) sexual impact, (4) self-image, (5) partner and transmission, (6) interactions with physicians, and (7) control/life impact. HIP scores are reversely relates to the subjects’ QoL, by which a higher score indicating a heavier psychosocial burden.
Results
Patients with GW experienced heavier psychosocial burdens than those of the general population, and females experienced heavier burdens than males (male vs. female: 49.20 vs.51.38, P < 0.001). “Self Image” and “Sexual Impact” were the two domains that affected patients the most, with mean HIP scores of 63.09 and 61.64, respectively. Women suffered heavier psychosocial burdens than men in the domain of “Worries and Concerns” (female vs. male: 54.57 vs. 42.62, P < 0.001), but lower psychosocial burdens in the domains of “Sexual Impact” (female vs. male: 59.16 vs. 65.26, P < 0.001) and “Interactions with Doctors” (female vs. male: 34.40 vs. 41.97, P < 0.001). Patients from Nan**g suffered a higher psychosocial burden than those of Bei**g, especially in domains of “Emotional Impact”, “Sexual Impact”, “Partner and Transmission”, and “Interactions with Doctors”.
Conclusions
Patients with GW suffered heavy psychological burden, and self-image and sexual-related concern were the primary cause of burdens. It’s important to change the current biomedical model to bio-psycho-social model, and establish psychosocial support systems. The distinctions of origins of psychosocial burden between genders identified will be informative for prevention of GW and control efforts in China and other similar settings.
Similar content being viewed by others
Background
Genital warts (GW) are the most common sexually transmitted Infections (STI) in the world with a substantial burden of disease. The reported incidence of GW in United States is 205/100,000 person-year [1]. This high incidence elicits concern regarding GW incidence in China, a develo** country lacking complete disease surveillance and registration systems. GW are a highly visible and recurrent condition primarily caused by low risk Human Papillomavirus (HPV) infection, [2]. Timely prophylactic HPV vaccination has been shown to be an effective way to prevent precancerous lesions and GW [3]. With worldwide implementation of vaccination, the potential added benefits of preventing both the majority of cases of GW and accompanying psychosocial impact by HPV vaccination should be considered and assessed.
In addition to biological intervention, psychosocial intervention turns out to be an important area for the current disease prevention and control, and change from a biomedical model to a bio-psycho-social model. Previous studies demonstrated that GW was associated with a significant detriment to health-related Quality of life (QoL), but the origins of these psychosocial burdens were still unclear [4–7]. Recently, literature reported that female patients with GW underwent a significantly heavier psychosocial burden than the general population in China [5, 9]. As most patients with STIs are diagnosed in sexually transmitted diseases (STD) clinics in China, subjects for this cross-sectional survey were recruited from the STD Clinic department of Institute of Dermatology in Nan**g and Bei**g You An hospital in Bei**g of China.
Study population
From February to May 2008, patients were invited to join the study during their routine clinical visits if they recently had a diagnosis of GW. It usually took half an hour to finish the visit by a deputy chief physician or 15–20 minutes by an attending doctor. After informed consent and a primary screening interview conducted by the investigator, patients were invited to attend the study regardless of their gender or whether they were an incident or recurrent case. Eligible subjects were aged 18–65 years, had experienced a hospital-based diagnosis of genital warts within the past three months, signed the informed consent, and were required to be in otherwise good physical health based on self-reported medical history with no significant co-morbid conditions. For the purpose of investigating the pure psychosocial impact of genital warts and to avoid confounding factors, patients were ineligible if they reported a history of HPV vaccination, alcohol or drug abuse in the past year, or other STIs over the past six months. Subjects were also ineligible if they were concurrently enrolled in other clinical studies, or had any condition that the investigator thought to be influential to the study.
Ethical approval was obtained from the Institutional Review Board of the Cancer Foundation of China.
Data collection
Basic demographic information (i.e., age, income, education, and marital status), HPV knowledge, and assessment of psychosocial burden were collected by the HIP questionnaire, [5, 10] which was completed by the patient in the presence of a trained interviewer who could assist with any questions participants had about the survey.
The HIP examined seven specific psychosocial domains by 29 items: 1) Worries and Concerns; 2) Emotional Impact; 3) Sexual Impact; 4) Self Image; 5) Partner and Transmission; 6) Interactions with Doctors; 7) Control/Life Impact (see Table 1 and Additional file 1). The questionnaire administered to both sexes was identical, except for two questions directed at male participants regarding the gender of their sexual partners. Male subjects specified if their sexual activity was homosexual, heterosexual or both, and whether intercourse was vaginal, oral, anal, or a combination. Additionally, male subjects were not required to answer questions on the topic of suffering from cervical cancer.
The HIP questionnaire was demonstrated to have favorable reliability, construct validity, and ability to discriminate amongst varying degrees of disease severity [10]. Cronbach’s alpha ranged from 0.64 to 0.90 and was ≥0.7 for 5/7 domains [10]. The Mandarin Chinese version of the HIP questionnaire was generated through a standardized process, and has previously been used in Taiwan [7, 10, 11].
Each item was scored individually to a 10-point discrete analog scale, which used visual-spatial, numeric, and verbal descriptive anchors (from “not at all” to “extremely”) to assess the different psychosocial impact of each item on the participant. Each item’s score was then linearly transformed to a 0–100 scale according to the arithmetic of HIP [10]. Transformations were performed to unify the indicated meanings of individual scores (a higher score indicated heavier burden), with some items reverse-scored to account for the inverse meaning. The individual domain scale scores were computed as the sum of the items over the number of items answered in each associated domain. To create the overall HIP score, the mean was computed as the sum of all the items over the number of items answered on all domain scales. A mean total HIP score below 40 signified little to no impact; scores between 40 and 70 implied moderate impact; and above 70, indicated heavy psychosocial impact [7].
Quality control was performed throughout the project for uniformity. This included training local interviewers before the project started, providing all participants with a letter of introduction describing self-administration in order to obtain a more consistent standard for questionnaires, and running regular quality control procedures to ensure the completion of the questionnaires and accuracy of data entry.
Data analysis
The software SAS 9.0 was used for data analysis. Demographic information was compared using the Pearson ×2 test, except for age and HIP mean score which were estimated using T test analysis. GLM proc was used for the comparisons of HIP scores by different psychosocial domains between genders and areas. Histograms were used to visualize comparisons of psychosocial burdens between genders. All the analyses used two-sided tests.
Results
Socio-demographic characteristics
A total of 204 men and 334 women were invited to participate in this study. 13 men and 4 women refused to participate due to concern of privacy or time consumption. Finally, 330 eligible women and 191 men were enrolled. The majority of participants were married (66.2%) with a mean age of 31.9 years old (yrs). In general, women were younger than men (Female vs. Male: 30.9 vs. 34.9 yrs, P < 0.001), had a lower level of education (P < 0.001) and income (P < 0.05). The coverage of insurance of women was lower than that of men as well (Female vs. Male: 34.5% vs. 52.0%, P < 0.001) (see Table 2). A quarter (25.8%) of the participants were unaware of HPV and its effects.
In addition, for questions regarding nature of sexual partners, 98.5% of males were self-reported to be heterosexual. The percentages of male intercourse types were tabulated to be 88.7%, 8.8%, and 2.5% for vaginal, vaginal associated with oral, and other combined variations (i.e. oral-anal, vaginal-anal), respectively.
Psychosocial burden assessed by HIP
Patients with genital warts suffered relatively high psychosocial burden, with a mean HIP score of 50.49 (95%CI: 49.41-51.57). Generally, females experienced heavier psychosocial burden than males (male vs. female: 49.20 vs.51.38, P < 0.001).
Considering the sources of psychosocial burdens, “Self Image” and “Sexual Impact” were the two HPV-related domains that affected patients the most, with mean HIP scores of 63.09 and 61.64, respectively, followed by “Worries and Concerns” (49.72), “Partner and Transmission” (48.42), “Control/Life Impact” (48.19), “Emotional Impact” (47.40), and “Interactions with Doctors” (37.47).
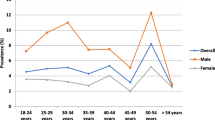
Comparing HIP domain scores between genders, significant differences were found in three domains. Women had heavier psychosocial burdens than men in domain of “Worries and Concerns” (female vs. male: 54.57 vs. 42.62, P < 0.001), but lower psychosocial burdens in the domains of “Sexual Impact” (female vs. male: 59.16 vs. 65.26, P < 0.001) and “Interactions with Doctors” (female vs. male: 34.40 vs. 41.97, P < 0.001) (see Figure 1). For domains of “Emotional Impact” (female vs. male: 47.58 vs. 47.14), “Self Image” (female vs. male: 63.31 vs. 62.77), “Control/Life Impact” (female vs. male: 48.35 vs. 47.96), and “Partner and Transmission” (female vs. male: 47.53 vs. 49.71) domains, females and males had comparable scores (P > 0.05) (see Table 3).
We also compared the psychosocial burdens of patients from different settings. In general, patients from Nan**g showed a higher psychosocial burden than those of Bei**g, especially in domains of “Emotional Impact” (Nan**g vs. Bei**g: 52.85 vs. 44.59, P < 0.001), “Sexual Impact” (Nan**g vs. Bei**g: 70.49 vs. 57.07, P < 0.001), “Partner and Transmission” (Nan**g vs. Bei**g: 56.38 vs. 44.31, P < 0.001), and “Interactions with Doctors” (Nan**g vs. Bei**g: 47.86 vs. 32.10, P < 0.001) (see Figure 2).
Discussion
The current work is a unique study focusing on the HPV-related psychosocial burden of male and female patients with GW using the HPV-specific HIP questionnaire. Our results showed that patients with GW had a substantially higher psychosocial burden. Most importantly, by using the HIP questionnaire, this study is the first to identify the origins of psychosocial burden of GW patients for both genders. We found that female patients with GW had heavier worries and concerns than male patients, but men had heavier psychosocial burden regarding domains of self-image and interaction with doctors. The origins of the psychosocial burden were mostly from “Self Image” and “Sexual Impact” domains, which highlighted the key domains that doctors should focus on. Results from this study will be informative for prevention of GW and control efforts in China and other similar settings.
Predominant domain of psychosocial burden for patients with GW
It has been evidenced that patients with GW lost quality of life and had significantly heavy psychosocial burden by various measures such as EQ-5D, group interview, and the Short-Form (SF)-12 [16]. A formal system for “Medical-psychological counseling” should be established in comprehensive hospitals, including establishing special psychological counseling departments and providing essential financial support for consultation. In addition, appropriate training for the identification of psychosocial disease should be developed for Chinese medical students and physicians, as this is currently lacking.
Secondly, we know that as a develo** country, there is a huge gap between basic medical therapy and the demand of patients in China. To help alleviate the psychosocial burden, we suggest the development of innovative approaches to help with consultation. There are tiered levels of medical workers in China, including the provincial, municipal, county, and village levels. Although these medical workers receive different levels of formal medical training, even the lesser-trained workers usually function as physicians within their local communities, gaining trust and respect from their patients. We suggest physicians and other medical workers work together to provide educational lectures and counseling services during the primary stages of the aforementioned consultation system establishment. In addition, we suggest that doctors not only focus their discussion with patients on the recurrent nature and hard-to-cure status when consulted for GW, but also provide patients effective preventable measures and lead them to local medical workers for helpful consultation [5]. The provider-patient relationship is a delicate one, and a compassionate, intelligent approach to treatment and prevention is imperative. STIs are sensitive subjects to discuss due to harsh stigmatization, and it would behoove health care providers to treat these situations as such. As for educational measures, local medical workers might also put up posters in the community and hold discussion sessions to increase awareness of disease etiology and preventive measures.
Study limitations
Firstly, selection biases could occur in this study due to the hospital-based, convenient sampling method we used; we also failed to assess the differences in characteristics between the study participants and those who declined to participate due to lacking of information of non-participants. Secondly, the cross-sectional data is limited for the time-dependent trend of psychosocial burdens of genital warts. Additional follow-up assessments should focus on multiple longitudinal time points after diagnoses, to help identify domains with sustainable impact and prioritize contents for consultation. Thirdly, the sample size was not large enough to acquire a high level of reliability, yet our data still provides novel information regarding specific HPV-related negative impacts of GW.
Conclusions
In conclusion, patients with genital warts had heavier psychosocial burdens than those of the general population, with females bearing a heavier burden than males. Self-image and sexual function were issues with which study patients experienced the highest psychosocial burdens. The distinctions of origins of psychosocial burdens between genders also help to prioritize causes of psychosocial burden and provide targeted psychosocial consultation services of GW. This study will also provide baseline utility data for a more detailed cost-effectiveness analysis of prophylactic HPV vaccination, which could help guide the development of educational public health campaigns.
Abbreviations
- GW:
-
Genital warts
- HPV:
-
Human papillomavirus
- HIP:
-
HPV Impact Profile
- QoL:
-
Quality of life
- STD:
-
Sexual transmitted diseases
- STI:
-
Sexually transmitted Infections.
References
Koshiol JE, Laurent SA, Pimenta JM: Rate and predictors of new genital warts claims and genital warts-related healthcare utilization among privately insured patients in the United States. Sex Transm Dis. 2004, 31 (12): 748-752. 10.1097/01.olq.0000145851.76025.ad.
Patel RV, Yanofsky VR, Goldenberg G: Genital warts: a comprehensive review. J Clin Aesthet Dermatol. 2012, 5 (6): 25-36.
Garland SM, Hernandez-Avila M, Wheeler CM, Perez G, Harper DM, Leodolter S, Tang GW, Ferris DG, Steben M, Bryan J, Taddeo FJ, Railkar R, Esser MT, Sings HL, Nelson M, Boslego J, Sattler C, Barr E, Koutsky LA, Females United to Unilaterally Reduce Endo/Ectocervical Disease (FUTURE) I Investigators: Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007, 356 (19): 1928-1943. 10.1056/NEJMoa061760.
Woodhall S, Ramsey T, Cai C, Crouch S, Jit M, Birks Y, Edmunds WJ, Newton R, Lacey CJ: Estimation of the impact of genital warts on health-related quality of life. Sex Transm Infect. 2008, 84 (3): 161-166. 10.1136/sti.2007.029512.
Wang SM, Shi JF, Kang DJ, Song P, Qiao YL: Impact of human papillomavirus-related lesions on quality of life: a multicenter hospital-based study of women in Mainland China. Int J Gynecol Cancer. 2011, 21 (1): 182-188. 10.1097/IGC.0b013e3181ffbed8.
Pirotta M, Ung L, Stein A, Conway EL, Mast TC, Fairley CK, Garland S: The psychosocial burden of human papillomavirus related disease and screening interventions. Sex Transm Infect. 2009, 85 (7): 508-513. 10.1136/sti.2009.037028.
Wang KL, Jeng CJ, Yang YC, Chen CA, Cheng WF, Chen TC, Mast TC, Wang YC, Hsieh CY: The psychological impact of illness among women experiencing human papillomavirus-related illness or screening interventions. J Psychosom Obstet Gynaecol. 2010, 31 (1): 16-23. 10.3109/01674820903564440.
Shi JF, Kang DJ, Qi SZ, Wu HY, Liu YC, Sun LJ, Li L, Yang Y, Li Q, Feng XX, Zhang LQ, Li J, Li XL, Yang Y, Niyazi M, Xu AD, Liu JH, **ao Q, Li LK, Wang XZ, Qiao YL: Impact of genital warts on health related quality of life in men and women in mainland China: a multicenter hospital-based cross-sectional study. BMC Public Health. 2012, 12: 153-10.1186/1471-2458-12-153.
Wen Chen KZ, Jufang S, Jane L, Lihong C, Xun Z, Bin L, Ivy W, Yu** W, Youlin Q: Chinese HPV ty** group: HPV type-distribution on genital warts in china: a multi-center study. 2009, Malmo, Sweden: 25th International Papillomavirus Conference, 30-41.
Mast TC, Zhu X, Demuro-Mercon C, Cummings HW, Sings HL, Ferris DG: Development and psychometric properties of the HPV Impact Profile (HIP) to assess the psychosocial burden of HPV. Curr Med Res Opin. 2009, 25 (11): 2609-2619.
Bullinger M, Alonso J, Apolone G, Leplege A, Sullivan M, Wood-Dauphinee S, Gandek B, Wagner A, Aaronson N, Bech P, Fukuhara S, Kaasa S, Ware JE: Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998, 51 (11): 913-923. 10.1016/S0895-4356(98)00082-1.
Woodhall SC, Jit M, Soldan K, Kinghorn G, Gilson R, Nathan M, Ross JD, Lacey CJ: The impact of genital warts: loss of quality of life and cost of treatment in eight sexual health clinics in the UK. Sex Transm Infect. 2011, 87 (6): 458-463. 10.1136/sextrans-2011-050073.
Senecal M, Brisson M, Maunsell E, Ferenczy A, Franco EL, Ratnam S, Coutlee F, Palefsky JM, Mansi JA: Loss of quality of life associated with genital warts: baseline analyses from a prospective study. Sex Transm Infect. 2011, 87 (3): 209-215. 10.1136/sti.2009.039982.
Drolet M, Brisson M, Maunsell E, Franco EL, Coutlee F, Ferenczy A, Ratnam S, Fisher W, Mansi JA: The impact of anogenital warts on health-related quality of life: a 6-month prospective study. Sex Transm Dis. 2011, 38 (10): 949-956. 10.1097/OLQ.0b013e3182215512.
Dominiak-Felden G, Cohet C, Atrux-Tallau S, Gilet H, Tristram A, Fiander A: Impact of human papillomavirus-related genital diseases on quality of life and psychosocial wellbeing: results of an observational, health-related quality of life study in the UK. BMC Public Health. 2013, 13 (1): 1065-10.1186/1471-2458-13-1065.
Ge Q, Wu JL: Study on situation of mental health personnel in the clinics of general hospitals of Wuhan. Master Degree thesis of HUST. 2008, 1 (1): 5-7.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/14/739/prepub
Acknowledgments
This study was funded by Merck Sharp & Dohme Ltd (China). We thank the all the doctors and the patients who participated in our study, as well as the colleagues of Cancer Institute/Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College and STD Clinic department of Chinese Academy of Medical Sciences of Peking Union Medical College for their generous support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All author’s declare that they have no competing interests.
Authors’ contributions
SZ Qi and SM Wang analyzed the data, generated the tables, figures and wrote the manuscript. JF Shi made important contributions on the result explanation sections and field work. QQ Wang and XS Chen made substantial contributions to the result interpretation. LJ Sun, A Liu and XL Xu made important contributions to the field work and data collection. Ning Jiang contributed to the data analysis and helped interpret the data in a meaningful way. N Zhang and P Sivasubramaniam helped review and revise the manuscript. YL Qiao helped design the study and made comments regarding the intellectual content. All authors read and approved the final manuscript.
Shu-Zhen Qi, Shao-Ming Wang contributed equally to this work.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Qi, SZ., Wang, SM., Shi, JF. et al. Human papillomavirus-related psychosocial impact of patients with genital warts in China: a hospital-based cross-sectional study. BMC Public Health 14, 739 (2014). https://doi.org/10.1186/1471-2458-14-739
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-14-739