Abstract
Background
Desflurane during early reperfusion has been shown to postcondition human myocardium, in vitro. We investigated the role of adenosine and bradykinin receptors, and generation of radical oxygen species in desflurane-induced postconditioning in human myocardium.
Methods
We recorded isometric contraction of human right atrial trabeculae hanged in an oxygenated Tyrode's solution (34 degrees Celsius, stimulation frequency 1 Hz). After a 30-min hypoxic period, desflurane 6% was administered during the first 5 min of reoxygenation. Desflurane was administered alone or with pretreatment of N-mercaptopropionylglycine, a reactive oxygen species scavenger, 8-(p-Sulfophenyl)theophylline, an adenosine receptor antagonist, HOE140, a selective B2 bradykinin receptor antagonist. In separate groups, adenosine and bradykinin were administered during the first minutes of reoxygenation alone or in presence of N-mercaptopropionylglycine. The force of contraction of trabeculae was recorded continuously. Developed force at the end of a 60-min reoxygenation period was compared (mean ± standard deviation) between the groups by a variance analysis and post hoc test.
Results
Desflurane 6% (84 ± 6% of baseline) enhanced the recovery of force after 60-min of reoxygenation as compared to control group (51 ± 8% of baseline, P < 0.0001). N-mercaptopropionylglycine (54 ± 3% of baseline), 8-(p-Sulfophenyl)theophylline (62 ± 9% of baseline), HOE140 (58 ± 6% of baseline) abolished desflurane-induced postconditioning. Adenosine (80 ± 9% of baseline) and bradykinin (83 ± 4% of baseline) induced postconditioning (P < 0.0001 vs control), N-mercaptopropionylglycine abolished the beneficial effects of adenosine and bradykinin (54 ± 8 and 58 ± 5% of baseline, respectively).
Conclusions
In vitro, desflurane-induced postconditioning depends on reactive oxygen species production, activation of adenosine and bradykinin B2 receptors. And, the cardioprotective effect of adenosine and bradykinin administered at the beginning of reoxygenation, was mediated, at least in part, through ROS production.
Similar content being viewed by others
Background
Anesthetic-induced postconditioning (PostC) is a phenomenon whereby a brief exposure of the myocardium to a volatile halogenated anesthetic, at the very onset of reperfusion, markedly reduces myocardial injury following prolonged ischemia: anesthetic-induced PostC has been confirmed in several mammalian species including rat, mouse, rabbit, and human [1–8].
The mechanism of volatile anesthetic-induced decrease of reperfusion injury remains incompletely understood. Endogenous activation of opioids, bradykinin, and adenosine receptors can trigger the complex protective signalling pathway of ischemic PostC [9]. It has been shown that adenosine and bradykinin postconditioned isolated rabbit [10] and rat hearts [11], via stimulation of adenosine and B2 receptors. At present, the involvement of adenosine and bradykinin receptors in anesthetic-induced PostC remains unknown, whereas these receptors were shown to be involved in anesthetic-induced preconditioning [12]. On the other hand, several studies showed that volatile anesthetic triggered intracellular reactive oxygen species (ROS) production [13], and that ROS production may mediate and/or trigger the preconditioning signalling cascade. Thus, sevoflurane and desflurane-induced preconditioning were abolished by ROS scavengers [14]. However, only two studies suggested that ROS were involved in isoflurane-induced PostC in mouse myocardium in vivo [3], and in sevoflurane-induced PostC in isolated rat hearts [8].
The objectives of our study were to determine whether: 1) ROS generation, and adenosine and bradykinin receptor stimulation may be involved in desflurane-induced PostC, 2) adenosine and bradykinin given at the beginning of reoxygenation mimic PostC, 3) adenosine and bradykinin receptors' activation was followed by myocardial PostC via ROS production.
Methods
After the approval of local medical ethics committee (Comité de Protection des Personnes Nord Ouest III, Caen, France) and written informed consent, right atrial appendages were obtained during cannulation for cardiopulmonary bypass from patients scheduled for routine coronary artery bypass surgery or aortic valve replacement. All patients received total intravenous anesthesia with propofol, remifentanil, and pancuronium. Patients with chronic atrial arrhythmia and with diabetes mellitus treated with insulin or oral hypoglycemic agents were excluded from the study [7, 14].
Experimental conditions
Right atrial trabeculae (one or two per appendage) were dissected and suspended vertically between an isometric force transducer (MLT0202, ADInstruments, Sydney, Australia) and a stationary stainless clip in a 200 ml organ bath filled with daily prepared Tyrode's modified solution containing (mM) 120 NaCl, 3.5 KCl, 1.1 MgCl2, 1.8 NaH2PO4, 25.7 NaHCO3, 2.0 CaCl2, and 5.5 glucose. The organ bath was maintained at 34°C by a thermostatic water circulator (Polystat micropros, Bioblock, Illkirch, France). The bathing solution was insufflated with carbogen (95% O2-5% CO2), resulting in a pH of 7.40 and a partial pressure of oxygen of 600 mm Hg. Isolated muscles were field-stimulated at 1 Hz by two platinum electrodes with rectangular wave pulses of 5 ms duration 20% above threshold (CMS 95107, Bionic Instrument, Paris, France).
Trabeculae were equilibrated for 60 to 90 min to allow stabilization of their optimal mechanical performance at the apex of the length-active isometric tension curve (Lmax). At the end of the stabilization period, trabeculae were randomized to experimental groups detailed below. The force developed was measured continuously, digitized at a sampling frequency of 400 Hz, and stored on a Writable Compact Disc for analysis (MacLab, AD Instrument, Sydney, Australia).
At the end of each experiment, the length and the weight of the muscle were measured. The muscle cross-sectional area was calculated from its weight and length assuming a cylindrical shape and a density of 1. To avoid core hypoxia, trabeculae included in the study should have a cross-sectional area less than 1.0 mm2, a force of contraction normalized per cross-sectionnal area (FoC) > 5.0 mN/mm2 and a ratio of resting force/total force less than 0.45.
Experimental protocol
In all groups, hypoxia-reoxygenation was performed by replacing 95% O2-5% CO2 with 95% N2-5% CO2 in the buffer for 30-min, followed by a 60-min oxygenated recovery period.
In the Control group (Control; n = 8) muscles were exposed to the hypoxia-reoxygenation protocol alone. In the desflurane treatment groups, desflurane was delivered to the organ bath by the gas flow passing through a specific calibrated vaporizer. Desflurane concentration in the carrier gas phase was measured with an infrared calibrated analyzer (Capnomac, Datex, Helsinki, Finland). Desflurane was administered at 6% (Desflurane 6%; n = 6) during the first 5 min of reoxygenation (fig. 1).
Schematic diagram depicting the experimental protocol. In the Desflurane + inhibitor groups and Inhibitor groups, MPG was administered at 150 μM, SPT was administered at 100 μM, and HOE 140 was administered at 20 nM. In adenosine and adenosine + inhibitor groups, adenosine was administered at 100 μM. In bradykinin and bradykinin + inhibitor groups, bradykinin was administered at 1 μM. MPG: N-mercaptopropionylglycine; SPT: 8-(p-Sulfophenyl) théophylline.
Mechanisms involved in desflurane-induced PostC were studied in presence of desflurane 6%, because we have previously shown that 6% was effective to induce PostC in human myocardium, in vitro.7 In separate groups exposed to 6% desflurane during the first 5-min of reoxygenation in the presence of 150 μM N-mercaptopropionylglycine, a ROS scavenger (Des + MPG; n = 6), 100 μM 8-(p-Sulfophenyl)theophylline, an adenosine receptor antagonist (Des + SPT; n = 6), 20 nM HOE140, a selective B2 bradykinin receptor antagonist (Des + HOE; n = 6). Pharmacological agents were administered 5 min before, throughout, and 10 min after desflurane administration (fig. 1).
The effect of MPG, SPT, and HOE140 alone was studied in separate groups exposed to 150 μM N-mercaptopropionylglycine (MPG; n = 6), 100 μM 8-(p-Sulfophenyl)theophylline (SPT; n = 6), 20 nM HOE140 (HOE; n = 6), 5 min before and during the first 15 min of reoxygenation (fig. 1).
Sequence of activation of adenosine and bradykinin receptors and ROS generation
In separate experimental groups, trabeculae were randomly assigned to receive 1) 100 μM adenosine alone, in the 15 first min of reoxygenation (adenosine (ADO) group; n = 6), or 2) co-superfused with pre-treatment (5 min before and 15 min after reoxygenation) with 100 μM SPT (ADO + SPT; n = 6), or 3) with 150 μM MPG (ADO + MPG; n = 6) (fig. 1).
In 3 other separate experimental groups, trabeculae were randomly assigned to receive: 1) 1 μM bradykinin alone, in the 15 first min of reoxygenation (BK group; n = 6), or 2) co-superfused with pre-treatment (5 min before and 15 min after reoxygenation) with 20 nM HOE140 (BK + HOE; n = 6), or 3) with 150 μM MPG (BK + MPG; n = 6) (fig. 1).
The concentrations of inhibitors MPG [14], SPT [10], HOE 140 [11], and activators adenosine [10], bradykinin [15] used here have been validated in previous experimental studies, in vitro.
Chemicals
MPG and adenosine were purchased from Calbiochem (VWR International, Fontenay sous Bois, France) and bradykinin, HOE 140, SPT were obtained from Sigma Aldrich (Saint Quentin Fallavier, France). Desflurane was purchased from GlaxoWellcome (Marly-le-Roi, France).
Statistical Analysis
The endpoint of the study was the recovery of FoC at 60 min of reoxygenation (FoC60, expressed as percent of baseline). All values were compared by ANOVA with application of a post hoc Bonferroni test. Power analysis calculated a group size of n = 5 to detect a difference of 40% in FoC (Control and inhibitors group: FoC60 = 50 ± 9% of baseline, and Desflurane 6% group: FoC60= 90 ± 9% of baseline) with a power of 0.8 at alpha-level of 0.05. The number of experiments per group was calculated based on an one-way analysis of variance (ANOVA) with 4 Control and inhibitors groups and 1 desflurane 6% group. Data are expressed as mean ± SD. Baseline values of main mechanical parameters, age, preoperative left ventricular ejection fraction, and FoC60 were compared by univariate analysis of variance with group factor as the independent variable. If the P value was less than 0.05, a Bonferroni post hoc analysis was performed. Within-group data were analyzed over time using two way analysis of variance for repeated measures and Bonferroni post hoc analysis with group factor and time (baseline, hypoxia 5, 10, 20, 30 min, and reoxygenation 5, 10, 20, 30, 40, 50, and 60 min) as independent variables.
Results
There were no differences between groups for patients' demographic data, preoperative treatments, and left ventricular ejection fraction (Table 1). Eighty six human right atrial trabeculae were studied. There were no differences in baseline values for Lmax, cross-sectionnal area, ratio of resting force to total force, and FoC between groups (Table 2).
Effects of desflurane on hypoxia reoxygenation on human atrial trabeculae
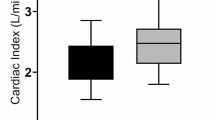
In the Control group, reoxygenation resulted in a partial recovery of FoC (FoC60: 51 ± 8% of baseline). Desflurane increased the FoC60 as compared to Control group (FoC60: 84 ± 6% of baseline vs. Control; P < 0.0001) (fig. 2).
Recovery of force of contraction of isolated human right atrial trabeculae at the end of the 60-min reoxygenation period after the 30-min hypoxic challenge in groups exposed to Desflurane 6% (Des) alone or in the presence of MPG, SPT, HOE. Data are mean ± SD. *P < 0.0001 vs. control, Des + MPG, Des + SPT, Des + HOE, MPG, SPT, HOE. Des: desflurane; HOE: HOE 140; MPG: N-mercaptopropionylglycine; SPT: 8-(p-Sulfophenyl) théophylline.
Effects of N-mercaptopropionylglycine, 8-(p-Sulfophenyl)theophylline and HOE 140 in desflurane treated preparations
Desflurane-induced enhanced recovery of FoC at the end of reoxygenation was abolished (P < 0.0001) in presence of MPG (FoC60: 54 ± 3% of baseline), SPT (FoC60: 62 ± 9% of baseline), HOE 140 (FoC60: 58 ± 6% of baseline).
As compared to the control group (control: 51 ± 8% of baseline), MPG alone (MPG: 56 ± 2% of baseline; P = 0.08), SPT alone (SPT: 59 ± 3% of baseline; P = 0.06), and HOE 140 alone (HOE 140: 54 ± 7% of baseline; P = 0.29) did not significantly modify FoC60 (fig. 2).
Effects of adenosine and bradykinin on hypoxia reoxygenation
Administration of adenosine and bradykinin, during the first 15 min of the reoxygenation period, significantly increased the recovery of FoC60 as compared to the control group (80 ± 9% of baseline in adenosine group and 83 ± 4% of baseline in bradykinin group; vs. Control group, P < 0.0001). Recovery of FoC60 measured in presence of adenosine or bradykinin were similar to that measured in Desflurane group (respectively P = 0.37 and P = 0.74 vs. desflurane group) (fig. 3).
Effects of 8-(p-Sulfophenyl)theophylline and N-mercaptopropionylglycine on adenosine administration
The effect of adenosine on FoC60 was abolished by pretreatment with SPT (FoC60: 53 ± 8% of baseline), and with MPG (FoC60: 54 ± 8% of baseline) (P < 0.0001 vs. adenosine group) (fig. 3).
Recovery of force of contraction of isolated human right atrial trabeculae at the end of the 60-min reoxygenation period after the 30-min hypoxic challenge in groups exposed to Desflurane 6% (Des) alone, exposed to adenosine (ADO) alone or in presence of SPT, MPG; exposed to bradykinin (BK) alone or in presence of HOE, MPG. Control and Des groups are the same that presented in figure 2. Data are mean ± SD. *P < 0.0001 vs. control, ADO + SPT, ADO + MPG, BK + HOE, BK + MPG. ADO: adenosine, BK: bradykinin; Des: desflurane; HOE: HOE 140; MPG: N-mercaptopropionylglycine; SPT: 8-(p-Sulfophenyl) théophylline.
Effects of HOE 140 and N-mercaptopropionylglycine on bradykinin administration
The enhanced recovery of FoC60 induced by bradykinin was abolished by the pre-treatment with HOE140 (48 ± 8% of baseline), and with MPG (55 ± 3% of baseline) (P < 0.0001 vs. bradykinin group) (fig. 3).
Discussion
In the present study, we showed that the cardioprotection triggered by desflurane during early reoxygenation involved ROS generation, and stimulation of adenosine and bradykinin B2 receptors. Furthermore, adenosine and bradykinin-induced PostC involved at least in part, ROS production.
The present study shows that administration of MPG abolished desflurane-induced PostC in human myocardium, in vitro. These results strongly suggest that desflurane-induced PostC involved ROS production. At present, only two studies have shown, in mouse and rat heart, that isoflurane and sevoflurane-induced PostC was abolished by treatment with ROS scavengers [3, 8]. In contrast, numerous studies have shown that ROS play a fundamental role in anesthetic-induced preconditioning [14, 16]. Müllenheim et al. demonstrated that ROS scavengers, blocked the reduction in myocardial infarct size resulting from isoflurane-induced preconditioning [16]. Isoflurane-induced preconditioning was mediated by ROS generated from electron transport chain complex III, in rabbit heart [17]. Moreover, in ventricular myocytes volatile anesthetics inhibit complex I of the electron transport chain [18], and, ROS mediated the mitochondrial uncoupling induced by desflurane treatment [19]. Tanaka et al. reported that mitochondrial adenosine triphosphate-sensitive potassium (mitoKATP) channel opening triggered isoflurane-induced preconditioning via ROS generation, in rabbit in vivo [20]. We have previously shown that opening of mitoKATP was an essential step of desflurane-induced PostC in human myocardium [7]. Thus, it could be hypothesized that desflurane-induced PostC generates ROS via mitoKATP channels opening. Further studies are required to examine the exact relationship between mitoKATP channel opening and ROS generation during early reperfusion.
The role of adenosine and bradykinin receptors' stimulation in desflurane-induced PostC was studied here for the first time using human myocardium. The present results show that both adenosine and B2 bradykinin receptors' stimulation are involved in desflurane-induced PostC. Pre-treatment with adenosine receptors inhibitor (SPT) and specific B2 bradykinin receptor' inhibitor (HOE140) abolished desflurane-induced PostC. Similarly, the beneficial effects of ischemic PostC were abolished by SPT, in rat and rabbit hearts [10, 21, 22]. Penna et al. showed that HOE 140 infusion eliminated the cardioprotective effect induced by ischemic PostC, in isolated rat hearts [11]. Additionally, a growing body of evidence supports the concept that anesthetic PostC triggers a cardioprotective cascade of molecular signalling events similar to that of ischemic PostC [23]. Then, previous studies showed specific involvement of A2A and A3 adenosine receptors in ischemic PostC in mouse [10, 24], and A1, A2B adenosine receptors in rabbit heart, in vitro [25, 26]. Using gene knockout mice, it has been shown that ischemic PostC-induced decreased in infarct volume was triggered by activation of adenosine A1 and bradykinin B2 receptors [27]. In contrast, with anesthetic-induced PostC, the involvement of adenosine receptors (specifically the A1 adenosine receptors) stimulation in isoflurane-induced preconditioning has been established [28–30].
Then, we showed that activation of adenosine and bradykinin receptors (via administration of adenosine or bradykinin), at the onset of reoxygenation, enhanced the recovery of FoC60 as compared to the control group. Lu et al, in rat ventricular myocytes, showed that adenosine-induced PostC was mediated by stimulation of adenosine A1 receptors as suggested by abolition of cardioprotective effect of adenosine in presence of 1,3-dipropyl-8-cyclopentylxanthine (DPCPX) as A1 adenosine receptor antagonist [31]. Nevertheless, Penna et al. showed that a 3-min administration of adenosine at the beginning of reperfusion did not decrease infarct volume in isolated rat hearts [21]. This discrepancy may result from differences in adenosine concentration between studies (i.e. 30 μM in Penna's study vs 100 μM in Lu's study and our own) and from the brief administration which may be ineffective to stimulate adenosine receptors. Thus, Penna et al showed that a 40 min administration of adenosine during reperfusion was necessary to decrease infarct size [21]. In another study, Penna et al have shown, in isolated rat hearts, that brief repetitive administration of bradykinin during early reperfusion could trigger PostC, whereas continuous administration in the same period wasn't cardioprotective [11].
Our data showed that pretreatment by HOE 140 abolished bradykinin effects, suggesting that bradykinin effects at the beginning of reoxygenation were mediated by the specific stimulation of B2 receptors, in accordance with Penna' s data [11]. Although the exact mechanism by which adenosine and bradykinin protect human myocardium in vitro is still unknown, studies based on animal models have suggested that ROS may mediate PostC [11]. Our data show that MPG abolished adenosine- and bradykinin-induced postC, suggesting that adenosine and bradykinin receptors' activation triggered PostC, at least in part, via ROS generation during early reoxygenation. In addition to ROS production, it has been shown that activation of adenosine and bradykinin receptors during reperfusion may promote mitoKATP channels opening [11, 31], activation of the RISK pathway including pro survival PI3K/Akt and MEK/ERK 1/2 pathways, p70s6K activation [15, 32, 33], and phosphorylation of GSK-3β, and prevent the mPTP opening, in rat ventricular myocytes and in isolated rat heart [34, 35] These signalling steps have been shown to be involved in ischemic and anesthetic induced PostC. Nevertheless, one study showed that preconditioning triggered by adenosine did not include ROS signaling in isolated rabbit heart [36].
Finally, enhanced recovery of force of human atrial trabeculae after exposure to desflurane, adenosine and bradykinin may suggest an anti-stunning effect of PostC. Whereas PostC reduced infarct size, it does not protect against myocardial stunning in dogs and rabbits [37], moreover post-ischemic systolic function was not modify by ischemic PostC and adenosine as compared to control group in isolated rat heart [21]. Definitely, our results cannot be extrapolated to myocardial stunning which is defined as a completely reversible myocardial dysfunction, because in the present experimental model the contractile dysfunction was not reversible even after 2 hours of reoxygenation [38].
Several limitations must be considered when interpreting our results. First the effects of anesthetic drugs, diseases, or medical treatments received by the patients before obtaining atrial appendages cannot be ruled out. Furthermore, although our experimental groups showed comparable demographic data (table 1), age has been shown to impair ischemic PostC in senescent mouse hearts [39–41], and should also be considered in patients. Second, our experiments were performed under moderate hypothermia (34°C) to ensure stability of trabeculae over time. However, during surgical procedures moderate hypothermia may occur. Third, blockade of adenosine receptors with SPT was not isoform specific, and we have investigated the role of ROS production using MPG. We did not directly measure ROS production nor the particular species of ROS. Fourth, as described in myocardial preconditioning, the beneficial effects of PostC have also been described on reperfusion-induced arrhythmias [42] and myocardial conctractility [43]. Fifth, we measured recovery of post hypoxic contractile function but not the infarct volume. However, it is not possible to precisely quantify the volume of necrosis in isolated trabeculae. Furthermore, it has been shown that the improved recovery of contractile function produced by preconditioning was proportional to reduced infarct size [44]. Finally, previous studies from our laboratories clearly showed that contractile dysfunction is a reliable parameter.
Conclusion
We have shown that stimulation of adenosine and bradykinin B2 receptors and ROS generation, during early reoxygenation, were involved in desflurane-induced PostC in human myocardium, in vitro. Additionally, the cardioprotective effect of adenosine and bradykinin administered at the beginning of reoxygenation, was mediated, at least in part, through ROS production.
References
Obal D, Dettwiler S, Favoccia C, Scharbatke H, Preckel B, Schlack W: The influence of mitochondrial KATP-channels in the cardioprotection of preconditioning and postconditioning by sevoflurane in the rat in vivo. Anesth Analg. 2005, 101: 1252-60. 10.1213/01.ANE.0000181336.96511.32.
Deyhimy DI, Fleming NW, Brodkin IG, Liu H: Anesthetic preconditioning combined with postconditioning offers no additional benefit over preconditioning or postconditioning alone. Anesth Analg. 2007, 105: 316-24. 10.1213/01.ane.0000267524.71445.e7.
Tsutsumi YM, Yokoyama T, Horikawa Y, Roth DM, Patel HH: Reactive oxygen species trigger ischemic and pharmacological postconditioning: in vivo and in vitro characterization. Life Sci. 2007, 81: 1223-7. 10.1016/j.lfs.2007.08.031.
Chiari PC, Bienengraeber MW, Pagel PS, Krolikowski JG, Kersten JR, Warltier DC: Isoflurane protects against myocardial infarction during early reperfusion by activation of phosphatidylinositol-3-kinase signal transduction: evidence for anesthetic-induced postconditioning in rabbits. Anesthesiology. 2005, 102: 102-9. 10.1097/00000542-200501000-00018.
Krolikowski JG, Bienengraeber M, Weihrauch D, Warltier DC, Kersten JR, Pagel PS: Inhibition of mitochondrial permeability transition enhances isoflurane-induced cardioprotection during early reperfusion: the role of mitochondrial KATP channels. Anesth Analg. 2005, 101: 1590-6. 10.1213/01.ANE.0000181288.13549.28.
Lange M, Redel A, Lotz C, Smul TM, Blomeyer C, Frank A, Stumpner J, Roewer N, Kehl F: Desflurane-induced postconditioning is mediated by beta-adrenergic signaling: role of beta 1- and beta 2-adrenergic receptors, protein kinase A, and calcium/calmodulin-dependent protein kinase II. Anesthesiology. 2009, 110: 516-28. 10.1097/ALN.0b013e318197ff62.
Lemoine S, Beauchef G, Zhu L, Renard E, Lepage O, Massetti M, Khayat A, Galera P, Gérard JL, Hanouz JL: Signaling pathways involved in desflurane-induced postconditioning in human atrial myocardium in vitro. Anesthesiology. 2008, 109: 1036-44. 10.1097/ALN.0b013e31818d6b09.
Yao YT, Li LH, Chen L, Wang WP, Li LB, Gao CQ: Sevoflurane postconditioning protects isolated rat hearts against ischemia-reperfusion injury: the role of radical oxygen species, extracellular signal-related kinases 1/2 and mitochondrial permeability transition pore. Mol Biol Rep. 2010, 37: 2439-46. 10.1007/s11033-009-9755-4.
Burley DS, Baxter GF: Pharmacological targets revealed by myocardial postconditioning. Curr Opin Pharmacol. 2009, 9: 177-88. 10.1016/j.coph.2008.11.009.
Kin H, Zatta AJ, Lofye MT, Amerson BS, Halkos ME, Kerendi F, Zhao ZQ, Guyton RA, Headrick JP, Vinten-Johansen J: Postconditioning reduces infarct size via adenosine receptor activation by endogenous adenosine. Cardiovasc Res. 2005, 67: 124-33. 10.1016/j.cardiores.2005.02.015.
Penna C, Mancardi D, Rastaldo R, Losano G, Pagliaro P: Intermittent activation of bradykinin B2 receptors and mitochondrial KATP channels trigger cardiac postconditioning through redox signaling. Cardiovascular Research. 2007, 75: 168-77. 10.1016/j.cardiores.2007.03.001.
Roscoe AK, Christensen JD, Lynch C: Isoflurane, but not halothane, induces protection of human myocardium via adenosine A1 receptors and adenosine triphosphate-sensitive potassium channels. Anesthesiology. 2000, 92: 692-701. 10.1097/00000542-200006000-00029.
Kevin LG, Novalija E, Riess ML, Camara AK, Rhodes SS, Stowe DF: Sevoflurane exposure generates superoxide but leads to decreased superoxide during ischemia and reperfusion in isolated hearts. Anesth Analg. 2003, 96: 949-55. 10.1213/01.ANE.0000052515.25465.35.
Hanouz JL, Zhu L, Lemoine S, Durand C, Lepage O, Massetti M, Khayat A, Plaud B, Gérard JL: Reactive oxygen species mediate sevoflurane- and desflurane-induced preconditioning in isolated human right atria in vitro. Anesth Analg. 2007, 105: 1534-9. 10.1213/01.ane.0000286170.22307.1a.
Bell RM, Yellon DM: Bradykinin limits infarction when administered as an adjunct to reperfusion in mouse heart: the role of PI3K, Akt and eNOS. J Mol Cell Cardiol. 2003, 35: 185-93. 10.1016/S0022-2828(02)00310-3.
Müllenheim J, Ebel D, Frossdorf J, Preckel B, Thomer V, Schlack W: Isoflurane preconditions myocardium against infarction via release of free radicals. Anesthesiology. 2002, 96: 934-40. 10.1097/00000542-200204000-00022.
Hanley PJ, Ray J, Brandt U, Daut J: Halothane, isoflurane and sevoflurane inhibit NADH: ubiquinone oxidoreductase (complex I) of cardiac mitochondria. J Physiol. 2002, 544: 687-93. 10.1113/jphysiol.2002.025015.
Ludwig LM, Tanaka K, Eells JT, Weihrauch D, Pagel PS, Kersten JR, Warltier DC: Preconditioning by isoflurane is mediated by reactive oxygen species generated from mitochondrial electron transport chain complex III. Anesth Analg. 2004, 99: 1308-15. 10.1213/01.ANE.0000134804.09484.5D.
Sedlic F, Pravdic D, Ljubkovic M, Marinovic J, Stadnicka A, Bosnjak ZJ: Differences in production of reactive oxygen species and mitochondrial uncoupling as events in the preconditioning signaling cascade between desflurane and sevoflurane. Anesth Analg. 2009, 109: 405-11. 10.1213/ane.0b013e3181a93ad9.
Tanaka K, Weihrauch D, Ludwig LM, Kersten JR, Pagel PS, Warltier DC: Mitochondrial adenosine triphosphate-regulated potassium channel opening acts as a trigger for isoflurane-induced preconditioning by generating reactive oxygen species. Anesthesiology. 2003, 98: 935-43. 10.1097/00000542-200304000-00021.
Penna C, Mancardi D, Tullio F, Pagliaro P: Intermittent adenosine at the beginning of reperfusion does not trigger cardioprotection. J Surg Res. 2009, 153: 231-8. 10.1016/j.jss.2008.02.070.
Yang X, Philipp S, Downey J, Cohen M: Postconditioning's protection is not dependent on circulating blood factors or cells but involves adenosine receptors and requires PI3-kinase and guanylyl cyclase activation. Basic Res Cardiol. 2005, 100: 57-63. 10.1007/s00395-004-0498-4.
Pagel PS: Postconditioning by volatile anesthetics: salvaging ischemic myocardium at reperfusion by activation of prosurvival signaling. J Cardiothorac Vasc Anesth. 2008, 22: 753-65. 10.1053/j.jvca.2008.03.005.
Morrison RR, Tan XL, Ledent C, Mustafa SJ, Hofmann PA: Targeted deletion of A2A adenosine receptors attenuates the protective effects of myocardial postconditioning. Am J Physiol Heart Circ Physiol. 2007, 293: H2523-9. 10.1152/ajpheart.00612.2007.
Donato M, D'Annunzio V, Berg G, Gonzalez G, Schreier L, Morales C, Wikinski RL, Gelpi RJ: Ischemic postconditioning reduces infarct size by activation of A1 receptors and K+(ATP) channels in both normal and hypercholesterolemic rabbits. J Cardiovasc Pharmacol. 2007, 49: 287-92. 10.1097/FJC.0b013e31803c55fe.
Philipp S, Yang XM, Cui L, Davis AM, Downey JM, Cohen MV: Postconditioning protects rabbit hearts through a protein kinase C-adenosine A2b receptor cascade. Cardiovasc Res. 2006, 70: 308-14. 10.1016/j.cardiores.2006.02.014.
** L, Das A, Zhao ZQ, Merino VF, Bader M, Kukreja RC: Loss of myocardial ischemic postconditioning in adenosine A1 and bradykinin B2 receptors gene knockout mice. Circulation. 2008, 118: S32-7. 10.1161/CIRCULATIONAHA.107.752865.
Cope DK, Impastato WK, Cohen MV, Downey JM: Volatile anesthetics protect the ischemic rabbit myocardium from infarction. Anesthesiology. 1997, 86: 699-709. 10.1097/00000542-199703000-00023.
Ismaeil MS, Tkachenko I, Gamperl AK, Hickey RF, Cason BA: Mechanisms of isoflurane-induced myocardial preconditioning in rabbits. Anesthesiology. 1999, 90: 812-21. 10.1097/00000542-199903000-00024.
Kersten JR, Orth KG, Pagel PS, Mei DA, Gross GJ, Warltier DC: Role of adenosine in isoflurane-induced cardioprotection. Anesthesiology. 1997, 86: 1128-39. 10.1097/00000542-199705000-00017.
Lu J, Zang WJ, Yu XJ, Jia B, Chorvatova A, Sun L: Effects of postconditioning of adenosine and acetylcholine on the ischemic isolated rat ventricular myocytes. Eur J Pharmacol. 2006, 549: 133-9. 10.1016/j.ejphar.2006.08.030.
Förster K, Paul I, Solenkova N, Staudt A, Cohen MV, Downey JM, Felix SB, Krieg T: NECA at reperfusion limits infarction and inhibits formation of the mitochondrial permeability transition pore by activating p70S6 kinase. Basic Res Cardiol. 2006, 101: 319-26. 10.1007/s00395-006-0593-4.
Li Y, Sato T: Dual signaling via protein kinase C and phosphatidylinositol 3'-kinase/Akt contributes to bradykinin B2 receptor-induced cardioprotection in guinea pig hearts. J Mol Cell Cardiol. 2001, 33: 2047-53. 10.1006/jmcc.2001.1455.
Park SS, Zhao H, Mueller RA, Xu Z: Bradykinin prevents reperfusion injury by targeting mitochondrial permeability transition pore through glycogen synthase kinase 3beta. J Mol Cell Cardiol. 2006, 40: 708-16. 10.1016/j.yjmcc.2006.01.024.
Xu Z, Park SS, Mueller RA, Bagnell RC, Patterson C, Boysen PG: Adenosine produces nitric oxide and prevents mitochondrial oxidant damage in rat cardiomyocytes. Cardiovasc Res. 2005, 65: 803-12. 10.1016/j.cardiores.2004.12.004.
Cohen MV, Yang XM, Liu GS, Heusch G, Downey JM: Acetylcholine, bradykinin, opioids, and phenylephrine, but not adenosine, trigger preconditioning by generating free radicals and opening mitochondrial K(ATP) channels. Circ Res. 2001, 89: 273-8. 10.1161/hh1501.094266.
Couvreur N, Lucats L, Tissier R, Bize A, Berdeaux A, Ghaleh B: Differential effects of postconditioning on myocardial stunning and infarction: a study in conscious dogs and anesthetized rabbits. Am J Physiol Heart Circ Physiol. 2006, 291: H1345-50. 10.1152/ajpheart.00124.2006.
Walker DM, Walker JM, Pugsley WB, Pattison CW, Yellon DM: Preconditioning in isolated superfused human muscle. J Mol Cell Cardiol. 1995, 27: 1349-57. 10.1016/S0022-2828(05)82397-1.
Lauzier B, Delemasure S, Debin R, Collin B, Sicard P, Acar N, Bretillon L, Joffre C, Bron A, Creuzot-Garcher C, Vergely C, Rochette L: Beneficial effects of myocardial postconditioning are associated with reduced oxidative stress in a senescent mouse model. Transplantation. 2008, 85: 1802-8. 10.1097/TP.0b013e3181775367.
Przyklenk K, Maynard M, Darling CE, Whittaker P: Aging mouse hearts are refractory to infarct size reduction with post-conditioning. J Am Coll Cardiol. 2008, 51: 1393-8. 10.1016/j.jacc.2007.11.070.
Boengler K, Buechert A, Heinen Y, Roeskes C, Hilfiker-Kleiner D, Heusch G, Schulz R: Cardioprotection by ischemic postconditioning is lost in aged and STAT3-deficient mice. Circ Res. 2008, 102: 131-5. 10.1161/CIRCRESAHA.107.164699.
Dow J, Bhandari A, Kloner RA: Ischemic Postconditioning's Benefit on Reperfusion Ventricular Arrhythmias Is Maintained in the Senescent Heart. J Cardiovasc Pharmacol Ther. 2008, 13: 141-8. 10.1177/1074248408317705.
Sivaraman V, Mudalagiri NR, Di Salvo C, Kolvekar S, Hayward M, Yap J, Keogh B, Hausenloy DJ, Yellon DM: Postconditioning protects human atrial muscle through the activation of the RISK pathway. Basic Res Cardiol. 2007, 102: 453-9. 10.1007/s00395-007-0664-1.
Lasley RD, Anderson GM, Mentzer RM: Ischemic and hypoxic preconditioning enhance postischemic recovery of function in the rat heart. Cardiovasc Res. 1993, 27: 565-70. 10.1093/cvr/27.4.565.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2253/10/12/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
This work was supported by the Université de Caen Basse Normandie and Centre Hospitalier Universitaire de Caen.
Authors' contributions
SL and JLH designed the investigation, reviewed the literature and drafted the manuscript. SL, GB, CI, MM conducted the experiments. JLG, CB and RR contributed to the interpretation of the data.
All authors read and approved the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lemoine, S., Buléon, C., Rouet, R. et al. Bradykinin and adenosine receptors mediate desflurane induced postconditioning in human myocardium: role of reactive oxygen species. BMC Anesthesiol 10, 12 (2010). https://doi.org/10.1186/1471-2253-10-12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2253-10-12