Abstract
Salmonella Typhimurium establishes systemic infection by replicating in host macrophages. Here we show that macrophages infected with S. Typhimurium exhibit upregulated glycolysis and decreased serine synthesis, leading to accumulation of glycolytic intermediates. The effects on serine synthesis are mediated by bacterial protein SopE2, a type III secretion system (T3SS) effector encoded in pathogenicity island SPI-1. The changes in host metabolism promote intracellular replication of S. Typhimurium via two mechanisms: decreased glucose levels lead to upregulated bacterial uptake of 2- and 3-phosphoglycerate and phosphoenolpyruvate (carbon sources), while increased pyruvate and lactate levels induce upregulation of another pathogenicity island, SPI-2, known to encode virulence factors. Pharmacological or genetic inhibition of host glycolysis, activation of host serine synthesis, or deletion of either the bacterial transport or signal sensor systems for those host glycolytic intermediates impairs S. Typhimurium replication or virulence.
Similar content being viewed by others
Introduction
Salmonella enterica serovar Typhimurium (STM) is an important intracellular pathogen that causes gastroenteritis and life-threatening systemic disease in humans and animals1. It invades multiple cell types during infection, including dendritic cells, epithelial cells, and macrophages. Although macrophages generally represent the front-line host defense against invading bacterial pathogens, they are a crucial colonization niche during STM pathogenesis. The replication in macrophages enables STM to establish systemic disease in a susceptible host2,3. STM relies on the acquisition of nutrients from macrophages for rapid intracellular replication4,5. As the microenvironment inside the macrophages is nutrient limited, STM must adapt and assimilate available nutrients within the macrophages to meet its nutritional needs6. It has been indicated that STM need to simultaneously exploit multiple nutrients, including glucose, glycerol, fatty acids, N-acetylglucosamine (GlcNAc), and several other carbon substances, in macrophages to sustain intracellular growth and cause systemic infection4.
Recognition of microbial ligands by macrophages induces a shift in glucose metabolism from oxidative phosphorylation (OXPHOS) to aerobic glycolysis. This metabolic reprogramming in activated macrophages is referred to as the “Warburg effect”’, in which glucose is mainly converted to lactate via glycolysis and lactic acid fermentation even under normoxic conditions7. This increase in glycolysis is essential for the antibacterial functions of activated macrophages, as it evokes rapid ATP production to fuel inflammatory responses and cytokine production to control pathogen replication7,8. In addition, glycolysis supports the generation of reactive oxygen and nitrogen species, itaconate, and prostaglandins, all of which contribute to macrophage antimicrobial activities9,10. Furthermore, aerobic glycolysis in macrophages stimulated with bacterial lipopolysaccharide (LPS) is accompanied by upregulation of the serine synthesis pathway through the glycolytic intermediate 3-phosphoglycerate (3PG)11,12,13. The synthesis and downstream metabolism of serine is required for the optimal production of inflammatory cytokine interleukin (IL)-1β in activated macrophages13. IL-1β plays a major role in the induction and regulation of host defense14, underscoring the importance of increase in serine synthesis to combat bacterial infection. The effects of macrophage metabolic changes on STM replication and pathogenicity are unknown.
Several intracellular bacterial pathogens have been shown to induce metabolic alterations in macrophages in a targeted, specific manner that benefit the pathogen15. Legionella pneumophila promotes increased glycolysis and decreased OXPHOS in infected macrophages, which is essential for L. pneumophila growth16. Francisella tularensis prevents the shift of infected macrophages to aerobic glycolysis to promote bacterial survival17. However, the mechanisms about how the altered macrophage metabolism promote these pathogens growth and how STM reprograms macrophage metabolism are largely unclear.
The STM genome encodes two distinct type III secretion systems (T3SSs) within large regions termed Salmonella pathogenicity island (SPI)-1 and SPI-218, which are two major determinants of STM pathogenesis. SPI-1 genes are mainly expressed during STM invasion of nonphagocytic epithelial cells, and SPI-1 effectors are required for epithelial cell invasion via triggering actin-dependent membrane ruffling19. SPI-2 genes are mainly expressed when the bacterium is inside the macrophage phagosome, and SPI-2 effectors interfere with host signaling pathways to convert the antimicrobial phagosome into the Salmonella-containing vacuole (SCV), where STM resides and replicates20. SPI-2 effectors also enable STM to more efficiently acquire host nutrients by inducing formation of tubular structures that extend from the SCV5. Several SPI-1 effectors are also expressed during STM resides within the SCV and contribute to intracellular replication, including SopE2, which is a guanidine exchange factor with the Rho GTPase Cdc42 as its primary target21,22. However, the molecular mechanism by which SopE2 promotes STM intracellular growth is currently unknown.
Here, we show that STM increases macrophage glycolysis and uses the SPI-1 effector SopE2 to repress macrophage serine synthesis, leading to accumulation of the macrophage glycolytic intermediates 2-phosphoglycerate (2PG), 3PG, and phosphoenolpyruvate (PEP). We show that STM uses a sophisticated regulatory pathway to detect low-glucose levels in infected macrophages and to induce uptake of these three accumulated glycolytic intermediates as carbon sources, thus promoting replication and virulence. In addition, STM-infected macrophages accumulate pyruvate and lactate, and STM senses these intermediates and subsequently upregulates SPI-2 gene expression through the CreBC two-component system, which promotes STM intracellular replication and systemic infection. Collectively, our findings indicate that STM induces a specific metabolic program that promotes the accumulation of glycolytic intermediates in macrophages, and that STM uses the accumulated glycolytic intermediates as carbon sources and cues to support its intracellular replication and pathogenicity.
Results
STM infection enhances glycolysis and reduces serine synthesis in infected macrophages
Although STM has been previously shown to utilize glucose in macrophages23, the effects of STM infection on macrophage glucose metabolism remain unclear. To determine whether STM infection of host macrophages leads to changes in macrophage glucose metabolism, we infected mouse peritoneal macrophages (PMs) with STM and assessed changes in macrophage glycolytic capacity at 2, 8, and 20 h post infection (hpi) with a Seahorse extracellular flux analyzer. Glycolysis was increased, and OXPHOS was decreased following STM infection, as indicated by a significant increase in extracellular acidification rate (ECAR) (Fig. 1a, Supplementary Fig. 1a) and a significant decrease in basal oxygen consumption rate (OCR) (Fig. 1b, Supplementary Fig. 1b). STM-infected PMs showed a significantly increased lactate production at 2, 8, and 20 hpi (Supplementary Fig. 1c), confirming that glycolysis was increased. Moreover, STM-infected PMs exhibited a significantly increased glucose uptake rate at 2, 8, and 20 hpi compared with uninfected PMs (Supplementary Fig. 1d), as also noted in a previous study in which STM infection led to increased glucose uptake by macrophages at 5 hpi24, whereas the glucose uptake rate at 20 hpi is similar to that of 8 hpi, and both are higher compared with that of 2 hpi in STM-infected PMs (Supplementary Fig. 1d).
a, b, Extracellular acidification rate (ECAR) (a) and basal oxygen consumption rate (OCR) (b) in untreated (NT) peritoneal macrophages (PMs) or those infected with STM for 2, 8, or 20 h. c, d Fold changes in glucose metabolites (c) and schematic of glucose metabolism (d) in STM-infected (8 h) PMs versus untreated PMs. Metabolites that were significantly enriched (red), diminished (blue), or not significantly changed (green) are indicated (d). glucose 6-phosphate (G6P), fructose 6-phosphate (F6P), fructose-1,6-diphosphate (FBP), glyceraldehyde-3-phosphate (G3P), dihydroxyacetophenone (DHAP), 3-phosphoglycerate (3PG), 2-phosphoglycerate (2PG), phosphoenolpyruvate (PEP), acetyl-CoA (Ac-CoA), citratre (Cit), isocitrate (Ict), α-ketoglutarate(α-KG), succinate (Suc), succinyl coenzyme A (Suc-CoA), fumarate (Fum), malate (Mal), oxaloacetate (OAA), 6-phosphogluconate (6PG), Ribose 5-phosphate (R5P), erythrose 4-phosphate (E4P), xylulose 5-phosphate (X5P), glutathione (GSH). Data are presented as mean ± SD, n = 3 independent experiments (a–c). e Heatmap of the expression profiles of glucose metabolism genes in STM-infected (8 h) PMs versus untreated PMs. Z scores of the relative gene expression levels are displayed in the heatmaps (n = 3 independent experiments), with red representing higher and blue representing lower abundance. P values were determined using one-way ANOVA (a–c, e). *, **, *** P < 0.05, 0.01, 0.001, respectively e. Source data are included in Source Data file.
To define the specific changes in glycolytic flux that were induced by STM infection, we then conducted targeted quantitative metabolomics analysis, focusing specifically on STM-induced changes in central carbon metabolism. At 8 hpi, during active STM replication while the death of infected PMs is not evident (Supplementary Fig. 1e), STM-infected PMs showed significant increases of the flux through the glycolytic pathway (Fig. 1c, d, Supplementary Table 1). Following STM infection, we identified significant accumulations of glycolytic intermediates, including glucose 6-phosphate (G6P)/fructose 6-phosphate (F6P), fructose-1,6-bisphosphate (FBP), glyceraldehyde-3-phosphate (G3P), dihydroxyacetone phosphate (DHAP), phosphoglycerates (i.e., 2PG and 3PG), PEP, pyruvate, and lactate (Fig. 1c, d, Supplementary Table 1). The levels of some tricarboxylic acid (TCA) cycle intermediates, including citrate/isocitrate and malate were significantly decreased, while the levels of fumarate, succinate, and α-Ketoglutaric acid (α-KG) were significantly increased (Fig. 1c, d, Supplementary Table 1). The levels of the tested PPP intermediates, 6-phosphogluconate (6PG), ribose 5-phosphate (R5P), and erythrose 4-phosphate (E4P), were not significantly changed (Fig. 1c, d, Supplementary Table 1). The levels of serine and its downstream metabolites glycine and glutathione (GSH) were significantly decreased in STM-infected PMs (Fig. 1c, d, Supplementary Table 1). These observed metabolic changes were dominated by host metabolites, as each STM cells accounted for 0.01 to 0.02% of the total metabolite concentrations (Supplementary Table 1) and ~94% of the infected PMs contained no more than ten bacteria at 8 hpi (Supplementary Fig. 1e). Together, the metabolomics data indicate that STM infection enhances glycolysis and reduces the synthesis and downstream metabolism of serine in infected macrophages.
Transcriptome analysis was conducted to extend the metabolomics findings, revealing that the gene expression profiles of STM-infected PMs were consistent with the observed metabolomic changes (Fig. 1e). The mRNA levels of key glycolytic enzymes, including hexokinase (Hk), 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 3 (Pfkfb3), and dominant glucose transporter Slc2a1, were significantly upregulated in infected PMs relative to untreated PMs (Fig. 1e), which are consistent with the observed increase in the levels of glycolysis and glucose uptake of STM-infected PMs. The observed decreases in the levels of some TCA cycle intermediates can be explained by decreased mRNA expression of ATP citrate synthase (Acly), isocitrate dehydrogenase (Idh), α-KG dehydrogenase (Ogdh), and succinate dehydrogenase (Sdh) (Fig. 1e). The observed increases in the levels of α-KG, succinate, and fumarate could be attributed to the glutamine-dependent anerplerosis, which is activated during macrophages shift to a Warburg metabolism25,26. In this process, glutamine is utilized as an anaplerotic carbon source to replenish TCA cycle intermediates, and α-KG is converted from glutamine to enter into the TCA cycle, resulting in the increase in the levels of succinate and fumarate25. Corresponding to the unchanged PPP metabolite levels, the mRNA levels of key PPP enzymes were not significantly changed (Fig. 1e). Furthermore, in accordance with the diminished serine synthesis pathway metabolite levels, the mRNA level of 3-phosphoglycerate dehydrogenase (Phgdh), the key enzyme in the serine synthesis pathway27, and those of serine hydroxymethyltransferase 1 (Shmt1) and glutamate–cysteine ligase (Gclc), the key enzymes involved in glycine and GSH synthesis from serine28,29, respectively, were significantly decreased (Fig. 1e). Collectively, these findings suggest that glycolytic metabolism is increased, and serine synthesis and downstream metabolic pathways were downregulated in STM-infected macrophages.
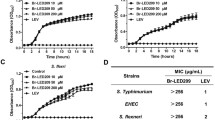
Increased glycolysis in macrophages promotes STM intracellular replication
We then investigated whether the observed increase in macrophage glycolysis is associated with STM intracellular replication. To inhibit macrophage glycolytic activities, we used a small interfering RNA (siRNA) to decrease the expression of the key glycolytic enzyme Pfkfb3 in the murine RAW264.7 macrophage cell line (48% reduction; Supplementary Fig. 2a). The knockdown significantly decreased STM replication in RAW264.7 cells (Fig. 2a), whereas pyruvate and lactate production was significantly decreased confirming that the glycolysis was inhibited in RAW264.7 cells owing to the knockdown (Supplementary Fig. 2b). Moreover, treatment of PMs with the glycolysis inhibitor PFK-15, which specifically inhibits Pfkfb3 and did not affect STM growth in LB medium and PRMI medium (Supplementary Fig. 2c), significantly decreased STM replication in PMs (Fig. 2b). These data indicate that increased glycolysis in macrophages during STM infection creates an intracellular environment conducive to STM replication.
a Replication of STM in Pfkfb3 siRNA-treated or control siRNA-treated RAW264.7 cells. b Replication of STM in PFK-15-treated or untreated PMs. c Serine and 3-phosphoglycerate (3PG) levels in PMs infected with live or heat-killed STM for 8 h in serine-depleted RPMI medium. d phgdh mRNA levels in PMs infected with live or heat-killed STM for 8 h in serine-depleted RPMI medium. e Serine and 3PG levels in phgdh-overexpressing (OE:+) or control (OE:−) RAW264.7 cells cultured in serine-depleted RPMI medium. f Serine and 3PG levels in Phgdh siRNA-treated or control siRNA-treated RAW264.7 cells cultured in serine-depleted RPMI medium. g Replication of STM in phgdh-overexpressing or control RAW264.7 cells. h Replication of STM in Phgdh siRNA-treated or control siRNA-treated RAW264.7 cells. i Replication of STM in 5 μM NCT-503-treated or untreated PMs. Data are presented as mean ± SD, n = 3 independent experiments; P values were determined using two-tailed unpaired Student’s t test (a, b, d–i) or one-way ANOVA (c). Source data are included in Source Data file.
STM actively suppresses serine synthesis and increases 3PG levels in macrophages
As STM infection reduced serine synthesis and downstream metabolism in PMs, we hypothesized that STM specifically represses serine synthesis to induce accumulation of the glycolytic intermediate 3PG, the precursor for de novo serine synthesis. To test this hypothesis, we infected PMs with live or heat-killed STM for 8 h in serine-depleted medium and measured the intracellular serine and 3PG concentrations in PMs. Compared with uninfected PMs, live STM-infected PMs showed significantly decreased serine levels, whereas heat-killed STM-infected PMs showed significantly increased serine levels (Fig. 2c, Supplementary Table 2). Notably, heat-killed STM induced significantly less 3PG accumulation in PMs than did live STM (Fig. 2c, Supplementary Table 2). In accordance with their differing serine levels, real-time quantitative PCR (RT-qPCR) analysis showed that phgdh transcription was significantly higher in PMs exposed to heat-killed STM than in those exposed to live STM (Fig. 2d).
Next, we overexpressed phgdh gene in RAW264.7 cells using the eukaryotic expression vector pcDNA3.1. Phgdh overexpression (2.0-fold increase; Supplementary Fig. 2d, left) resulted in significantly increased serine levels but decreased 3PG levels in live STM-infected RAW264.7 cells (Fig. 2e). In contrast, siRNA knockdown of Phgdh (39% reduction; Supplementary Fig. 2e, left) resulted in significantly decreased serine levels but increased 3PG levels in live STM-infected RAW264.7 cells (Fig. 2f). These data confirm that STM actively repressed macrophage serine synthesis, resulting in increased 3PG levels in infected macrophages.
Suppressed serine synthesis in macrophages promotes STM intracellular replication
We then investigated whether the reduction in serine synthesis in infected macrophages promotes intracellular STM replication. First, overexpression of phgdh in RAW264.7 cells (2.2-fold increase; Supplementary Fig. 2d, middle) significantly decreased STM intracellular replication (Fig. 2g). Second, siRNA-mediated Phgdh knockdown (44% reduction; Supplementary Fig. 2e, right) significantly increased STM replication in RAW264.7 cells (Fig. 2h). Finally, treatment with NCT-503, a phgdh inhibitor, significantly increased STM replication in PMs (Fig. 2i). Together, these results indicate that STM requires suppressed macrophage serine synthesis for maximal replication in macrophages.
Uptake of macrophage-derived 3PG is essential for STM intracellular replication and systemic virulence
We then investigated the mechanism by which macrophage glucose metabolism reprogramming promotes STM intracellular replication. Although glucose is an important carbon source during STM growth in macrophages23, the availability of individual nutrients, including glucose, is limited in macrophages4,30, leading us to hypothesize that STM can use the glycolytic intermediates that accumulate in macrophages as a carbon source. To test this hypothesis, we first confirmed that STM can utilize each of the accumulated intermediates as a sole carbon source for growth in vitro (Supplementary Fig. 3a). We then separately knocked out the bacterial transport systems for 2PG/3PG/PEP (referred to as 3PG hereafter, as these three intermediates can be easily interconverted and are imported through the same transporter in STM), G6P/F6P/G3P, pyruvate, and lactate, namely, PgtP31,32, Uhpt33, CstA-YbdD34, and LldP35, respectively. As expected, the mutant strains were unable to use the corresponding intermediates as a carbon source in vitro (Supplementary Fig. 3a). Although no specific transporters for FBP and DHAP have been reported, we showed that when FBP or DHAP were used as the sole carbon sources, in vitro growth of the uhpt mutant was inhibited (Supplementary Fig. 3a), indicating that Uhpt can transport both FBP and DHAP.
Next, as a previously published transcriptomic study showed that STM pgtP, cstA, ybdD, and lldP gene transcription was significantly upregulated in macrophages at 24 hpi but uhpt transcription was not significantly changed36, we evaluated the influence of pgtP, cstA-ybdD, or lldP knockout on STM intracellular replication and pathogenicity. pgtP mutation significantly decreased STM replication in PMs, as revealed by the results of gentamicin protection assays (Fig. 3a) and immunofluorescence (Supplementary Fig. 3b, c). The 3PG and lactate levels showed no significant difference between pgtP mutant- and wild-type (wt)-infected PMs (Supplementary Fig. 3d), indicating PgtP does not influence macrophage 3PG accumulation and thus indicating the replication defect of the pgtP mutant in macrophages is owing to its inability to utilize 3PG. Furthermore, mice infected with the pgtP mutant exhibited a significantly increased survival rate and decreased bacterial burdens in the liver and spleen compared with mice infected with wt STM (Fig. 3b, c). pgtP mutant complementation with the pgtP gene restored intracellular replication and virulence in mice to wt levels (Fig. 3a–c). However, the intracellular growth and virulence in mice of the cstA-ybdD mutant, lldP mutant, and cstA-ybdD lldP double mutant did not differ from those of wt STM (Supplementary Fig. 3e–g), revealing the utilization of host pyruvate and lactate is not essential for STM intracellular replication and pathogenicity. These data indicate that PgtP is required for STM intracellular replication and systemic virulence and that, of the accumulated host glycolytic intermediates, 3PG uptake is essential for STM intracellular replication and systemic virulence in mice.
a Replication of the wild-type (wt), pgtP mutant, or pgtP complemented STM strains in PMs. b Survival curves of mice infected i.p. with the wt (n = 16 mice), pgtP mutant (n = 14 mice), or pgtP complemented strains (n = 14 mice). c Liver and spleen bacterial burdens in mice infected with the wt, pgtP mutant, or pgtP complemented strains. d Replication of the wt or pgtP mutant STM strains in PMs cultured in RPMI medium containing 10 or 20 mM glucose. e Survival curves of mice infected i.p. with the wt or pgtP mutant STM strain and then injected i.p. with PBS or 20 mg of glucose every two days until 20 dpi or death (n = 8 mice per group). f Liver and spleen bacterial burdens in mice infected with the wt or pgtP mutant STM strain. Mice were infected as described in e. g Replication of wt STM in phgdh-overexpressing (OE:+) or control (OE:−) RAW264.7 cells in the presence or absence of 1 mM 3PG. h Replication of the wt, pgtP mutant, and ptsG manXYZ glk triple mutant STM strains in PMs. i Competitive index of the STM pgtP mutant versus the ptsG manXYZ glk triple mutant in the liver and spleen of infected mice. Data are presented as mean ± SD, n = 3 independent experiments a, d, g, h, n = 7 c, f or n = 9 i mice per group. P values were determined using two-tailed unpaired Student’s t test (a, g, h), log-rank Mantel–Cox test (b, e), Mann–Whitney U test (c, f, i) or one-way ANOVA (d). P = 0.0002 and 0.0012 for liver and spleen, respectively, based on raw CFU values of the pgtP mutant vs. ptsG manXYZ glk triple mutant (i). Source data are included in Source Data file.
Macrophage-derived 3PG is an important carbon source for STM intracellular replication
Next, we considered that if STM exploits 3PG as a carbon source, the impaired replication and virulence of the pgtP mutant may be relieved by the addition of another carbon source during infection. Supporting this hypothesis, we observed that glucose supplementation resulted in a significant increase in pgtP mutant replication in PMs (Fig. 3d), and that pgtP mutant infection resulted in significant higher mortality and greater bacterial burdens in the liver and spleen of glucose-treated mice than those of PBS-treated mice (Fig. 3e, f), demonstrating that 3PG was used by STM as a carbon source for intracellular growth. Furthermore, the reduced STM intracellular replication caused by macrophage serine synthesis upregulation was rescued by 3PG supplementation. When 3PG was added to the cell culture medium, STM intracellular replication in PMs and in phgdh-overexpressing RAW264.7 cells (2.7-fold increase in phgdh expression; Supplementary Fig. 2d, right) was significantly increased (Fig. 3g).
As glucose is thought to be required for the replication of STM in macrophages23,30, next we compared the roles of glucose and 3PG in STM intracellular replication and systemic virulence. Compared with that of a ptsG manXYZ glk triple mutant, which can neither take up nor utilize glucose23, the replication of the pgtP mutant in PMs was significantly decreased (Fig. 3h). We then performed in vivo competition assays to measure the difference in systemic tissue colonization between pgtP mutant and ptsG manXYZ glk triple mutant. The result showed that pgtP mutant was significantly outcompeted by the ptsG manXYZ glk triple mutant in spleen and liver of the infected mice (Fig. 3i), implying the virulence of the pgtP mutant is more attenuated than that of the ptsG manXYZ glk triple mutant. These data indicate that host-accumulated 3PG might play a more important role in STM intracellular replication and virulence than glucose.
STM uses the SPI-1 effector SopE2 to repress macrophage serine synthesis
The above results show that STM represses macrophage serine synthesis to trigger 3PG accumulation in macrophages, and that 3PG is used by intracellular STM as a major carbon source; thus, we next investigated the mechanisms by which STM represses macrophage serine synthesis. We first examined whether the effectors encoded by SPI-1 or SPI-2 influence phgdh gene expression. PMs infected with an SPI-1 mutant, but not those infected with an SPI-2 mutant, exhibited upregulated phgdh gene transcription compared with PMs infected with wt STM (Fig. 4a). The sopE2 mutant did not repress phgdh transcription in PMs, but other SPI-1 effector gene mutants did (Fig. 4b), and complementing the sopE2 mutant with sopE2 repressed phgdh transcription and expression in PMs to a level comparable to that in wt STM-infected PMs (Fig. 4b, c). In addition, transcription of the two key glycolytic genes, pfkfb3 and slc2a1, was unaffected by the mutation of sopE2 (Supplementary Fig. 4a). sopE2 overexpression in RAW264.7 cells decreased phgdh transcription and expression (Fig. 4d, e), whereas PMs infected with the sopE2 mutant exhibited decreased intracellular 3PG levels and increased intracellular serine levels compared with PMs infected with wt STM (Fig. 4f). Finally, sopE2 mutant replication in PMs was significantly reduced compared with wt STM replication in PMs (Fig. 4g), but was increased by exogenous 3PG addition (Fig. 4h). Together, these results indicate that SopE2 is the factor responsible for suppression of macrophage serine synthesis.
a Quantitative PCR (RT-qPCR) analysis of phgdh mRNA levels in untreated (NT) PMs or PMs infected with wt STM, SPI-1 mutant, or SPI-2 mutant for 8 h. b RT-qPCR analysis of phgdh mRNA levels in untreated PMs or those infected with wt STM, the indicated mutant or complemented strain for 8 h. c Immunoblot analysis of Phgdh protein levels in untreated PMs or those infected with the wt, sopE2 mutant, or sopE2-complemented strain for 8 h. d RT-qPCR analysis of phgdh mRNA levels in sopE2-overexpressing (SopE2 OE) or control RAW264.7 cells. e Immunoblot analysis of Phgdh protein levels in sopE2-overexpressing or control RAW264.7 cells. f Serine and 3PG levels in PMs infected with wt STM or sopE2 mutant for 8 h. g Replication assays of the wt, sopE2 mutant, or sopE2-complemented strains in PMs in the presence or absence of 1 mM 3PG. h Replication assays of the wt or sopE2 mutant in PMs in the presence or absence of 1 mM 3PG. i Immunoblot analysis of Cdc42 protein levels, j RT-qPCR analysis of phgdh mRNA levels, k 3PG levels, l replication of wt STM, and m replication of wt STM in the presence or absence of 1 mM 3PG, in Cdc42 siRNA-treated or control siRNA-treated HeLa cells. Data are presented as mean ± SD, n = 3 independent experiments; P values were determined using two-tailed unpaired Student’s t test (a, b, d, f–h, j–m). Immunoblots are representative of three independent experiments (c, e, i). Source data are included in Source Data file.
SopE2 is a guanine nucleotide exchange factor whose primary target is the host Rho GTPase Cdc4237. We thus sought to determine whether SopE2 represses phgdh expression through Cdc42. siRNA knockdown of Cdc42 (70% reduction; Fig. 4i) significantly increased phgdh gene transcription in HeLa cells (Fig. 4j), whereas both the intracellular 3PG level and intracellular bacterial replication were significantly reduced in Cdc42 siRNA-treated cells (Fig. 4k, l). Furthermore, addition of exogenous 3PG increased bacterial replication in Cdc42 siRNA-treated cells (Fig. 4m). These results indicate that STM represses the macrophage serine synthesis pathway through a SopE2-mediated Cdc42 mechanism.
We next tested the involvement of SopE2 in STM systemic infection. SopE2 is known to be required for STM to enter and cross the intestinal epithelium38. To bypass intestinal invasion and test the systemic infection of STM, mice were infected by the intraperitoneal route. Compared with mice infected with wt STM, mice infected with the sopE2 mutant exhibited a significantly increased survival rate and reduced bacterial burdens in the liver and spleen (Supplementary Fig. 4b, c), indicating that SopE2 contributes to STM systemic infection. Because SopE2 and PgtP are involved in the macrophage accumulation and STM utilization of 3PG, respectively, we then compared the roles of SopE2 and PgtP in STM intracellular replication and systemic infection. We observed that the replication of the pgtP mutant in PMs was significantly decreased compared to that of the sopE2 mutant, whereas comparable to that of the sopE2 pgtP double mutant (Supplementary Fig. 4d). The in vivo competition assays showed that the pgtP mutant was significantly outcompeted by the sopE2 mutant, whereas competed equally with the sopE2 pgtP double mutant in liver and spleen of the infected mice (Supplementary Fig. 4e). Together, these data suggest that the contribution of SopE2 to STM systemic virulence is entirely dependent on PgtP, and the suppression of macrophage serine synthesis by SopE2 is necessary for STM systemic infection.
STM senses decreased glucose levels in macrophages to upregulate bacterial 3PG uptake
To reveal how STM takes advantage of the elevated 3PG levels in infected macrophages, we investigated the regulatory system involved in STM pgtP upregulation inside macrophages. Upon investigating the regulatory functions of 18 putative regulatory proteins that present in STM but absent in Escherichia coli (Supplementary Table 3) by transcriptome analysis, we identified STM2748 (named VrpA, virulence-related regulatory protein A) as a potential positive regulator of pgtP, as the transcription of pgtP and the other three genes in the pgt gene cluster was downregulated in the vrpA mutant (NCBI SRA accession: PRJNA561041). RT-qPCR analysis further confirmed the positive regulation of pgtP by VrpA when STM grown in N-minimal medium (Fig. 5a), which has a mildly acidic pH and low magnesium and phosphorus concentrations that recapitulate the conditions inside host macrophages. Consistent with the role of pgtP in STM intracellular replication, vrpA mutation significantly decreased STM replication in PMs (Fig. 5b).
a RT-qPCR analysis of pgtP mRNA levels in the wt, vrpA mutant, and vrpA-complemented STM strains. Bacteria were grown in N-minimal medium for 6 h before collection. b Replication of the wt, vrpA mutant, and vrpA-complemented strains in PMs. c Survival curves of mice infected i.p. with the wt, vrpA mutant, or complemented strains. Left: n = 21 mice for wt, n = 15 mice for vrpA mutant. Right: n = 14 mice per group. d Liver and spleen bacterial burdens in mice infected with the wt, vrpA mutant, or complemented strains. e Electrophoretic mobility shift assay (EMSA) of the pgtA promoter with purified VrpA protein. f Fold enrichment of the pgtA promoter in VrpA-chromatin immunoprecipitation (ChIP) samples. g RT-qPCR analysis of vrpA and pgtP mRNA levels in the wt, crp mutant, and crp-complemented strains. Bacteria were grown in N-minimal medium for 6 h before collection. h EMSA of the vrpA promoter with purified CRP protein in the presence or absence of 0.1 mM cAMP. i Fold enrichment of the vrpA promoter in CRP-ChIP samples. j cAMP levels in STM collected from infected PMs at 2, 8, and 20 h post infection (hpi). k RT-qPCR analysis of crp, vrpA, and pgtP mRNA levels in intracellular STM. Fold changes in intracellular gene expression level at 2, 8, and 20 hpi relative to the expression of the corresponding genes in RPMI medium (0 hpi) are presented. Data are presented as mean ± SD, n = 3 (a, b, f, g, i, k) or n = 5 independent experiments (j), n = 7 mice per group (d). Images are representative of three independent experiments (e, h). P values were determined using two-tailed unpaired Student’s t test (a, b, j), log-rank Mantel–Cox test (c), Mann–Whitney U test (d) or one-way ANOVA (f, g, i). Source data are included in Source Data file.
Next, we tested the influence of vrpA mutation on STM virulence in mice. Compared with mice infected with wt STM, mice infected with the vrpA mutant exhibited a significantly increased survival rate and reduced bacterial burdens in the liver and spleen (Fig. 5c, d). Moreover, complementation of the vrpA mutant with vrpA restored bacterial replication in PMs and virulence in mice, whereas complementation of the vrpA mutant with pgtP partially restored bacterial replication in PMs and virulence in mice (Fig. 5b–d), further confirming that pgtP is controlled by vrpA. The above data indicate that the contribution of VrpA to STM virulence is partially dependent on PgtP, and this was further confirmed by the facts that the replication of the vrpA pgtP double mutant was significantly decreased in PMs compared with that of the pgtP mutant (Supplementary Fig. 5a) and vrpA pgtP double mutant was significantly outcompeted by the pgtP mutant in liver and spleen of the infected mice (Supplementary Fig. 5b).
We then investigated whether VrpA directly regulates pgtP. Electrophoretic mobility shift assays (EMSAs) and chromatin immunoprecipitation and quantitative PCR (ChIP-qPCR) assays revealed that VrpA binds to the pgtP promoter both in vitro and in vivo (Fig. 5e, f), indicating that VrpA activates pgtP directly.
To determine how VrpA is induced when STM inside macrophages, the upstream regulatory system(s) were then investigated. Using program BPROM39, we identified a putative CRP-binding site in the vrpA promoter region, indicating CRP might be a potential regulator of VrpA. crp mutation significantly decreased vrpA and pgtP transcription levels (Fig. 5g), implying that CRP positively regulates vrpA and pgtP expression. Consistent with the roles of vrpA and pgtP in STM intracellular replication and systemic infection, crp mutation significantly decreased STM replication in PMs (Supplementary Fig. 5c); mice infected with a crp mutant exhibited a markedly increased survival rate and reduced bacterial burdens in the liver and spleen (Supplementary Fig. 5d, e).
The results of EMSA and ChIP-qPCR analyses showed that CRP binds to the vrpA promoter both in vitro and in vivo (Fig. 5h, i), confirming that CRP directly regulates vrpA. In addition, CRP regulates its target genes upon complexation with cyclic adenosine monophosphate (cAMP), and its regulatory activity is determined by the cAMP level;40,41 we found that cAMP was also required for CRP binding to the vrpA promoter in vitro (Fig. 5h). Together, these results indicate that CRP is a direct regulator of VrpA in STM, which regulates pgtP during intracellular replication.
As the availability of glucose inside macrophages is limited during bacterial infection4, we hypothesized that decreased glucose uptake by the STM phosphotransferase (PTS) system increases cAMP levels and leads to crp upregulation in STM. We next investigated cAMP levels and crp expression in intracellular STM during infection, and found both to increase (Fig. 5j, k). Consistent with these increases, vrpA and pgtP transcription levels in intracellular STM also increased (Fig. 5k).
We then investigated whether vrpA, pgtP, and crp expression was negatively regulated by glucose availability inside macrophages. To this end, we cultured PMs with Roswell Park Memorial Institute Medium (RPMI) medium containing 0.25, 0.5, or 2 g/L glucose for 16 h before infection with STM. Intracellular vrpA, pgtP, and crp transcription was induced earlier and at a higher level in PMs cultured in RPMI medium containing low-glucose concentrations (0.5 g/L or 0.25 g/L) than in PMs cultured with RPMI medium containing a high glucose concentration (2 g/L) (Supplementary Fig. 5f). It is highly likely that lower glucose concentration in the medium resulted in its lower concentration within macrophages, and thus bacterial vrpA, pgtP, and crp transcription was induced earlier and at a higher level. Moreover, when STM was cultured in RPMI medium containing different glucose concentrations (0–4 g/L), the transcription of these genes was more highly induced in bacteria cultured with no-glucose or low-glucose concentrations than in those cultured with high glucose concentrations (Supplementary Fig. 5g). We also repressed cellular glycolysis via Pfkfb3 knockdown in RAW264.7 cells before STM infection, and found that crp, vrpA, and pgtP transcription of the intracellular STM was significantly decreased upon Pfkfb3 knockdown (Supplementary Fig. 5h), further confirmed the induction of vrpA, pgtP, and crp expression in response to glucose limitation. Collectively, these data indicate that during STM infection of macrophages, the bacterial cAMP-CRP content increases owing to decreased glucose levels in macrophages, and that cAMP-CRP activates pgtP expression through VrpA, facilitating 3GP uptake.
STM senses macrophage-accumulated pyruvate and lactate by the two-component system CreBC to activate SPI-2 genes
Although our results indicate that the accumulated macrophage pyruvate and lactate were not utilized by STM as nutrients for intracellular replication, it is possible that they act as cues to control STM gene expression. Consistent with this hypothesis, the transcription of STM creB and creC genes, which encode the two-component system CreBC that is responsive to pyruvate and lactate42, was upregulated in macrophages at 24 hpi36. To determine whether the protein levels of CreB and CreC are increased inside macrophages, we constructed a creBC promoter-lux fusion (creBC-lux) and then compared its luminescence intensity inside PMs at 2, 8, and 20 hpi to that in RPMI medium. The results showed that the luminescence intensity of creBC-lux inside PMs was significantly increased at each time point post infection (Supplementary Fig. 6a), confirming the increased expression of CreBC during STM growth in macrophages. The upregulation of STM creBC inside macrophages indicates that CreBC might contribute to STM intracellular replication. Therefore, we knocked out the regulator creB and then tested the influence of creB knockout on STM intracellular replication and pathogenicity. We found that creB mutation significantly decreased STM replication in PMs, as revealed by the gentamicin protection assays (Fig. 6a) and immunofluorescence (Supplementary Fig. 3b, c). Moreover, mice infected with the creB mutant exhibited a significantly increased survival rate and decreased bacterial burdens in the liver and spleen (Fig. 6b, c). creB mutant complementation with the creB gene restored bacterial intracellular replication and virulence to WT levels both in vitro and in vivo (Fig. 6a–c). Together, these data suggest that CreBC is essential for STM intracellular replication and infection in mice.
a Replication of the wt, creB mutant, and complemented STM strains in PMs. b Survival curves of mice infected i.p. with the wt, creB mutant, or complemented strain (n = 12 mice per group). c Liver and spleen bacterial burdens in mice infected with the wt, creB mutant, or complemented strain. d RT-qPCR analysis of creB, creC, vrpB, and ssaG mRNA levels in response to 1 mM pyruvate or lactate. e SPI-2 gene expression patterns in the wt and creB mutant strains profiled using RNA-seq (n = 3 independent experiments), with red representing higher and blue representing lower abundance. f EMSA of the vrpB promoter with purified CreB protein. g Fold enrichment of the vrpB promoter in CreB-ChIP samples. h EMSA of the ssrA and ssrB promoters with purified VrpB protein. i Fold enrichment of the ssrA and ssrB promoters in VrpB-ChIP samples. j Replication of the wt, vrpB mutant, and complemented strains in PMs. k Survival curves of mice infected i.p. with the wt, vrpB mutant, or complemented strain (n = 12 mice per group). l Liver and spleen bacterial burdens in mice infected with the wt, vrpB mutant, or complemented strain. m RT-qPCR analysis of creB, vrpB, and ssaG mRNA levels in intracellular STM. n RT-qPCR analysis of ssaG mRNA levels in the wt, creB mutant, or vrpB mutant strains in the presence or absence of 1 mM pyruvate or lactate. Data are presented as mean ± SD, n = 3 independent experiments (a, d, g, i, j, m, n), n = 7 mice per group (c, l). Images are representative of three independent experiments (f, h). P values were determined using two-tailed unpaired Student’s t test (a, j), log-rank Mantel–Cox test (b, k), Mann–Whitney U test (c, l) or one-way ANOVA (d, e, g, i, n). *, **, *** P < 0.05, 0.01, 0.001, respectively (e). Source data are included in Source Data file.
We then confirmed that pyruvate and lactate accumulation in macrophages induces creBC expression in STM. First, creB and creC transcription levels were significantly increased by the addition of lactate and pyruvate in vitro (Fig. 6d). Second, creB and creC transcription levels were significantly increased in bacteria cultured with lysate from STM-infected cells compared with bacteria cultured with lysate from mock-infected cells (Supplementary Fig. 6b). Third, we inhibited glycolysis and cellular pyruvate and lactate production via Pfkfb3 knockdown in RAW264.7 cells before STM infection, and found that creB transcription of the intracellular STM was significantly decreased upon Pfkfb3 knockdown (Supplementary Fig. 6c).
We next investigated the means by which pyruvate and lactate promote STM intracellular replication and virulence through CreB. RNA-seq data show that loss of creB reduced the transcription of all 33 SPI-2 genes in STMs cultured in N-minimal medium (Fig. 6e), and RT-qPCR analysis confirmed the positive regulation of SPI-2 gene expression by CreB in N-minimal medium (Supplementary Fig. 6d). In addition, creB mutation significantly decreased the transcription levels of the representative SPI-2 gene ssaG inside PMs at 2, 8, and 20 hpi, respectively (Supplementary Fig. 6e). Moreover, both pyruvate and lactate induced ssaG transcription in STM cultured in N-minimal medium, and creB mutation abolished this effect (Supplementary Fig. 6f), indicating that pyruvate and lactate induce SPI-2 gene expression in a CreB-dependent manner. However, lldp and cstA-ybdD double mutation did not influence ssaG transcription when STM grown in N-minimal medium supplied with pyruvate or lactate (Supplementary Fig. 6g), revealing that the utilization of pyruvate and lactate is not related with SPI-2 gene expression. Taken together, these data suggest that STM uses host-accumulated pyruvate and lactate as cues to activate SPI-2 gene expression via CreB.
CreB activates SPI-2 genes through the regulator VrpB
To further delineate the mechanism by which CreB contributes to STM intracellular replication and pathogenesis, we next investigated the pathway associated with SPI-2 regulation by CreB. Most previously identified SPI-2 regulators have been shown to activate SPI-2 gene expression through the regulators SsrA and/or SsrB43. However, our EMSA results showed that CreB did not bind to the promoter of either ssrA or ssrB (Supplementary Fig. 6h), suggesting that CreB may activate SPI-2 indirectly. ChIP-seq analysis showed that the promoter region of STM2180 (named vrpB), which encodes a LysR family transcriptional regulator, was significantly enriched in the CreB-ChIP sample compared with that in the control sample (NCBI SRA accession: PRJNA561041), suggesting that vrpB might be a direct CreB target. CreB binds a conserved cre tag sequence to regulate downstream genes in Escherichia coli44, but the upstream region of the vrpB gene does not contain a typical cre tag sequence. Through EMSA and ChIP-qPCR, we found that CreB bound to the vrpB promoter both in vitro and in vivo (Fig. 6f, g), confirming the direct regulation of vrpB by CreB. creB mutation significantly decreased vrpB gene transcription in STM cultured in N-minimal medium (Supplementary Fig. 6i). Together, these results reveal that CreB directly and positively regulates vrpB.
We then examined the regulatory mechanisms between VrpB and SPI-2 genes. Therefore, we knocked out vrpB and tested the influence of vrpB knockout on the expression of SPI-2 genes. vrpB mutation significantly decreased ssaG gene transcription in STM cultured in N-minimal medium (Supplementary Fig. 6j). EMSA and ChIP-qPCR results revealed that VrpB binds to the ssrA and ssrB promoters, indicating that VrpB activates SPI-2 gene expression directly (Fig. 6h, i). Consistent with the roles of CreB and SPI-2 in intracellular replication and systemic infection, vrpB mutation significantly decreased STM replication in PMs (Fig. 6j). In addition, mice infected with the vrpB mutant exhibited a significantly increased survival rate and decreased bacterial burdens in the liver and spleen (Fig. 6k, l). The replication of the creB vrpB double mutant in PMs was significantly decreased compared to that of the vrpB mutant (Supplementary Fig. 6k) and creB vrpB double mutant was significantly outcompeted by the vrpB mutant in liver and spleen of the infected mice (Supplementary Fig. 6l), indicating that the contribution of CreB to STM virulence is partially dependent on VrpB. In contrast, the intracellular replication of the vrpB ssrB double mutant is comparable to that of the ssrB mutant (Supplementary Fig. 6m) and the vrpB ssrB double mutant competed equally with the ssrB mutant in liver and spleen of the infected mice (Supplementary Fig. 6n), indicating that the contribution of VrpB to STM virulence are entirely dependent on SPI-2. This was further confirmed by the fact that complementation of the vrpB mutant with ssrB restored STM intracellular replication and virulence (Fig. 6j–l). Collectively, these results confirm VrpB as a positive regulator of SPI-2 genes and indicate that CreB activates SPI-2 gene expression by directly activating VrpB.
Consistent with these suggested functions, creB, vrpB, and ssaG transcript levels increased during STM growth in PMs (Fig. 6m). In addition, the creB, vrpB, and ssaG transcript levels were upregulated by the addition of lactate and pyruvate in vitro, and either creB or vrpB mutation abolished ssaG upregulation by lactate and pyruvate (Fig. 6n), further confirming the creB–vrpB–SPI-2 regulatory pathway. Also, the transcription of vrpB and ssaG was significantly decreased when STM replicated in Pfkfb3 knockdown RAW264.7 cells (Supplementary Fig. 6c). Collectively, these results indicate that during STM infection, CreBC activates SPI-2 genes through VrpB in response to increased pyruvate and lactate levels in macrophages, thus promoting STM intracellular replication and virulence.
Discussion
STM replication inside macrophages is a crucial step in the induction of systemic infection2,3, and requires large amounts of nutrients4,45. We studied the metabolic reprogramming of macrophages during STM infection and revealed the mechanisms by which this active reprogramming supports STM intracellular replication and systemic virulence; notably, this STM-driven macrophage metabolic reprogramming differs from the host-driven reprogramming that occurs when macrophages are activated by heat-killed STM or LPS. We also showed that STM uses the glycolytic intermediates that accumulate in macrophages as carbon sources and cues to establish successful intracellular replication, thus enabling systemic infection (see Fig. 7 for a schematic of our proposed mechanism).
STM translocates the effector SopE2 through the SPI-1 type III secretion system (T3SS), which represses macrophage serine synthesis and leads to the accumulation of glycolytic intermediates in macrophages. The decreased glucose level in macrophages induces the import of macrophage-derived 3PG as a main carbon source in order to support growth via VrpA in STM and senses increased pyruvate or lactate levels in macrophages to activate SPI-2 T3SS expression, thus promoting its intracellular replication and systemic infection.
Previously, although several reports indicated that STM blocks host OXPHOS during infection of the mouse colon mucosaChIP-qPCR ChIP experiments were performed as described above. Quantification of vrpA-, creB-, and crp-bound DNA was carried out by RT-qPCR using Power SYBR Green PCR Master Mix in an ABI QuantStudio 5 Real-Time PCR system. The relative enrichment of DNA regions of interest was calculated using the 2−ΔΔCt method. RAW264.7 cells were infected with the STM wt strain as described above. At 2, 4, 8, and 20 hpi, the infected cells were lysed with 1% Triton X-100, and intracellular bacteria were pelleted by centrifugation. The cAMP concentration in intracellular bacteria was measured by a Direct cAMP ELISA Kit (Abcam #ab133051) following the manufacturer protocol. Cell lysates were also plated, and cAMP concentrations were normalized to intracellular bacterial CFUs. Statistical significance was analyzed with GraphPad Prism 8.0.1 software (GraphPad Inc., San Diego, CA) using the two-tailed unpaired Student’s t test, one-way analysis of variance, log-rank (Mantel–Cox) test, or Mann–Whitney U test according to the test requirements (as stated in the figure legends). A P value of < 0.05 was considered statistically significant. Further information on research design is available in the Nature Research Reporting Summary linked to this article.Measurement of bacterial cAMP concentration
Statistical analysis
Reporting summary
Data availability
The RNA-seq and ChIP-seq data acquired in this study are available in the NCBI Sequence Read Archive (SRA, PRJNA561041). The metabolomic data have been deposited in MetaboLights (MTBLS2347). Source data are provided with this paper.
References
Fabrega, A. & Vila, J. Salmonella enterica serovar Typhimurium skills to succeed in the host: virulence and regulation. Clin. Microbiol. Rev. 26, 308–341 (2013).
Fields, P. I., Swanson, R. V., Haidaris, C. G. & Heffron, F. Mutants of Salmonella typhimurium that cannot survive within the macrophage are avirulent. Proc. Natl Acad. Sci. USA 83, 5189–5193 (1986).
Leung, K. Y. & Finlay, B. B. Intracellular replication is essential for the virulence of Salmonella typhimurium. Proc. Natl. Acad. Sci. USA 88, 11470–11474 (1991).
Steeb, B. et al. Parallel exploitation of diverse host nutrients enhances Salmonella virulence. PLoS Pathog. 9, e1003301 (2013).
Liss, V. et al. Salmonella enterica remodels the host cell endosomal system for efficient intravacuolar nutrition. Cell Host Microbe 21, 390–402 (2017).
Thompson, A., Fulde, M. & Tedin, K. The metabolic pathways utilized by Salmonella Typhimurium during infection of host cells. Environ. Microbiol. Rep. 10, 140–154 (2018).
Escoll, P. & Buchrieser, C. Metabolic reprogramming of host cells upon bacterial infection: why shift to a Warburg-like metabolism? FEBS J. 285, 2146–2160 (2018).
Freemerman, A. J. et al. Metabolic reprogramming of macrophages: glucose transporter 1 (GLUT1)-mediated glucose metabolism drives a proinflammatory phenotype. J. Biol. Chem. 289, 7884–7896 (2014).
Curi, R. et al. A past and present overview of macrophage metabolism and functional outcomes. Clin. Sci. 131, 1329–1342 (2017).
Nonnenmacher, Y. & Hiller, K. Biochemistry of proinflammatory macrophage activation. Cell Mol. life Sci. 75, 2093–2109 (2018).
Sullivan, M. R. et al. Increased serine synthesis provides an advantage for tumors arising in tissues where serine levels are limiting. Cell Metab. 29, 1410–1421 e1414 (2019).
Vander Heiden, M. G. & DeBerardinis, R. J. Understanding the intersections between metabolism and cancer biology. Cell 168, 657–669 (2017).
Rodriguez, A. E. et al. Serine metabolism supports macrophage IL-1β production. Cell Metab. 29, 1003–1011 e1004 (2019).
Gabay, C., Lamacchia, C. & Palmer, G. IL-1 pathways in inflammation and human diseases. Nat. Rev. Rheumatol. 6, 232–241 (2010).
Escoll, P. & Buchrieser, C. Metabolic reprogramming: an innate cellular defence mechanism against intracellular bacteria? Curr. Opin. Immunol. 60, 117–123 (2019).
Escoll, P. et al. Legionella pneumophila modulates mitochondrial dynamics to trigger metabolic repurposing of infected macrophages. Cell Host Microbe 22, 302–316 e307 (2017).
Wyatt, E. V. et al. Metabolic peprogramming of host cells by virulent Francisella tularensis for optimal replication and modulation of inflammation. J. Immunol. 196, 4227–4236 (2016).
Srikanth, C. V., Mercado-Lubo, R., Hallstrom, K. & McCormick, B. A. Salmonella effector proteins and host-cell responses. Cell. Mol. life Sci.: CMLS 68, 3687–3697 (2011).
Lou, L., Zhang, P., Piao, R. & Wang, Y. Salmonella pathogenicity island 1 (SPI-1) and its complex regulatory network. Front. Cell Infect. Microbiol. 9, 270 (2019).
Jennings, E., Thurston, T. L. M. & Holden, D. W. Salmonella SPI-2 type III secretion system effectors: molecular mechanisms and physiological consequences. Cell Host Microbe 22, 217–231 (2017).
Zhou, D. & Galan, J. Salmonella entry into host cells: the work in concert of type III secreted effector proteins. Microbes Infect. 3, 1293–1298 (2001).
Vonaesch, P. et al. The Salmonella Typhimurium effector protein SopE transiently localizes to the early SCV and contributes to intracellular replication. Cell Microbiol. 16, 1723–1735 (2014).
Bowden, S. D., Rowley, G., Hinton, J. C. & Thompson, A. Glucose and glycolysis are required for the successful infection of macrophages and mice by Salmonella enterica serovar typhimurium. Infect. Immun. 77, 3117–3126 (2009).
Sanman, L. E. et al. Disruption of glycolytic flux is a signal for inflammasome signaling and pyroptotic cell death. eLife 5, e13663 (2016).
Tannahill, G. M. et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature 496, 238–242 (2013).
DeBerardinis, R. J., Lum, J. J., Hatzivassiliou, G. & Thompson, C. B. The biology of cancer: metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 7, 11–20 (2008).
Vandekeere, S. et al. Serine synthesis via PHGDH is essential for heme production in endothelial cells. Cell Metab. 28, 573–587 e513 (2018).
Paone, A. et al. SHMT1 knockdown induces apoptosis in lung cancer cells by causing uracil misincorporation. Cell Death Dis. 5, e1525 (2014).
Lu, S. C. Glutathione synthesis. Biochim. biophys. Acta 1830, 3143–3153 (2013).
Eisele, N. A. et al. Salmonella require the fatty acid regulator PPARδfor the establishment of a metabolic environment essential for long-term persistence. Cell Host Microbe 14, 171–182 (2013).
Goldrick, D., Yu, G. Q., Jiang, S. Q. & Hong, J. S. Nucleotide sequence and transcription start point of the phosphoglycerate transporter gene of Salmonella typhimurium. J. Bacteriol. 170, 3421–3426 (1988).
Jiang, S. Q., Yu, G. Q., Li, Z. G. & Hong, J. S. Genetic evidence for modulation of the activator by two regulatory proteins involved in the exogenous induction of phosphoglycerate transport in Salmonella typhimurium. J. Bacteriol. 170, 4304–4308 (1988).
Hall, J. A. & Maloney, P. C. Altered oxyanion selectivity in mutants of UhpT, the Pi-linked sugar phosphate carrier of Escherichia coli. J. Biol. Chem. 280, 3376–3381 (2005).
Hwang S., et al. Peptide transporter CstA imports pyruvate in Escherichia coli K-12. J. Bacteriol. 200, e00771-17 (2018).
Nunez, M. F. et al. Transport of L-Lactate, D-Lactate, and glycolate by the LldP and GlcA membrane carriers of Escherichia coli. Biochem. Biophys. Res. Commun. 290, 824–829 (2002).
Stapels, D. A. C. et al. Salmonella persisters undermine host immune defenses during antibiotic treatment. Science 362, 1156–1160 (2018).
Stender, S. et al. Identification of SopE2 from Salmonella typhimurium, a conserved guanine nucleotide exchange factor for Cdc42 of the host cell. Mol. Microbiol. 36, 1206–1221 (2000).
Zhang, K. et al. Minimal SPI1-T3SS effector requirement for Salmonella enterocyte invasion and intracellular proliferation in vivo. PLoS Pathog. 14, e1006925 (2018).
Eppenhof, E. J. J. & Pena-Castillo, L. Prioritizing bona fide bacterial small RNAs with machine learning classifiers. PeerJ 7, e6304 (2019).
Kolb, A., Busby, S., Buc, H., Garges, S. & Adhya, S. Transcriptional regulation by cAMP and its receptor protein. Annu. Rev. Biochem. 62, 749–795 (1993).
Hanamura, A. & Aiba, H. A new aspect of transcriptional control of the Escherichia coli crp gene: positive autoregulation. Mol. Microbiol. 6, 2489–2497 (1992).
Cariss, S. J., Tayler, A. E. & Avison, M. B. Defining the growth conditions and promoter-proximal DNA sequences required for activation of gene expression by CreBC in Escherichia coli. J. Bacteriol. 190, 3930–3939 (2008).
Fass, E. & Groisman, E. A. Control of Salmonella pathogenicity island-2 gene expression. Curr. Opin. Microbiol. 12, 199–204 (2009).
Avison, M. B., Horton, R. E., Walsh, T. R. & Bennett, P. M. Escherichia coli CreBC is a global regulator of gene expression that responds to growth in minimal media. J. Biol. Chem. 276, 26955–26961 (2001).
Abu Kwaik, Y. & Bumann, D. Host delivery of favorite meals for intracellular pathogens. PLoS Pathog. 11, e1004866 (2015).
Liu, X., Lu, R., **a, Y. & Sun, J. Global analysis of the eukaryotic pathways and networks regulated by Salmonella typhimurium in mouse intestinal infection in vivo. BMC Genomics 11, 722 (2010).
Mattaini, K. R., Sullivan, M. R. & Vander Heiden, M. G. The importance of serine metabolism in cancer. J. Cell Biol. 214, 249–257 (2016).
Reid, M. A. et al. Serine synthesis through PHGDH coordinates nucleotide levels by maintaining central carbon metabolism. Nat. Commun. 9, 5442 (2018).
Martinez-Reyes, I. & Chandel, N. S. Mitochondrial TCA cycle metabolites control physiology and disease. Nat. Commun. 11, 102 (2020).
Coso, O. A. et al. The small GTP-binding proteins Rac1 and Cdc42 regulate the activity of the JNK/SAPK signaling pathway. Cell 81, 1137–1146 (1995).
Arozarena, I. et al. The Rho family GTPase Cdc42 regulates the activation of Ras/MAP kinase by the exchange factor Ras-GRF. J. Biol. Chem. 275, 26441–26448 (2000).
Figueira, R. & Holden, D. W. Functions of the Salmonella pathogenicity island 2 (SPI-2) type III secretion system effectors. Microbiology 158, 1147–1161 (2012).
Jiang, L. et al. PagR mediates the precise regulation of Salmonella pathogenicity island 2 gene expression in response to magnesium and phosphate signals in Salmonella Typhimurium. Cell Microbiol. 22, e13125 (2020).
Coombes, B. K., Wickham, M. E., Lowden, M. J., Brown, N. F. & Finlay, B. B. Negative regulation of Salmonella pathogenicity island 2 is required for contextual control of virulence during typhoid. Proc. Natl Acad. Sci. USA 102, 17460–17465 (2005).
Silphaduang, U., Mascarenhas, M., Karmali, M. & Coombes, B. K. Repression of intracellular virulence factors in Salmonella by the Hha and YdgT nucleoid-associated proteins. J. Bacteriol. 189, 3669–3673 (2007).
Vance, R. E., Isberg, R. R. & Portnoy, D. A. Patterns of pathogenesis: discrimination of pathogenic and nonpathogenic microbes by the innate immune system. Cell Host Microbe 6, 10–21 (2009).
Miao, E. A. & Warren, S. E. Innate immune detection of bacterial virulence factors via the NLRC4 inflammasome. J. Clin. Immunol. 30, 502–506 (2010).
Bijlsma, J. J. & Groisman, E. A. The PhoP/PhoQ system controls the intramacrophage type three secretion system of Salmonella enterica. Mol. Microbiol. 57, 85–96 (2005).
Linehan, S. A., Rytkonen, A., Yu, X. J., Liu, M. & Holden, D. W. SlyA regulates function of Salmonella pathogenicity island 2 (SPI-2) and expression of SPI-2-associated genes. Infect. Immun. 73, 4354–4362 (2005).
Lee, A. K., Detweiler, C. S. & Falkow, S. OmpR regulates the two-component system SsrA-ssrB in Salmonella pathogenicity island 2. J. Bacteriol. 182, 771–781 (2000).
Yoon, H., McDermott, J. E., Porwollik, S., McClelland, M. & Heffron, F. Coordinated regulation of virulence during systemic infection of Salmonella enterica serovar Typhimurium. PLoS Pathog. 5, e1000306 (2009).
Choi, J. & Groisman, E. A. The lipopolysaccharide modification regulator PmrA limits Salmonella virulence by repressing the type three-secretion system Spi/Ssa. Proc. Natl. Acad. Sci. USA 110, 9499–9504 (2013).
Czyz D. M., Willett J. W., Crosson S. Brucella abortus induces a Warburg shift in host metabolism that is linked to enhanced intracellular survival of the pathogen. J. Bacteriol. 199, e00227-17 (2017).
Kentner, D. et al. Shigella reroutes host cell central metabolism to obtain high-flux nutrient supply for vigorous intracellular growth. Proc. Natl Acad. Sci. USA 111, 9929–9934 (2014).
Westermann, A. J. et al. Dual RNA-seq unveils noncoding RNA functions in host-pathogen interactions. Nature 529, 496–501 (2016).
Jiang, L. et al. Signal transduction pathway mediated by the novel regulator LoiA for low oxygen tension induced Salmonella Typhimurium invasion. PLoS Pathog. 13, e1006429 (2017).
Liang, H., Li, L., Dong, Z., Surette, M. G. & Duan, K. The YebC family protein PA0964 negatively regulates the Pseudomonas aeruginosa quinolone signal system and pyocyanin production. J. Bacteriol. 190, 6217–6227 (2008).
Lim, S. et al. Mlc regulation of Salmonella pathogenicity island I gene expression via hilE repression. Nucleic Acids Res. 35, 1822–1832 (2007).
Lachmandas, E. et al. Microbial stimulation of different Toll-like receptor signalling pathways induces diverse metabolic programmes in human monocytes. Nat. Microbiol. 2, 16246 (2016).
Acknowledgements
This work was funded by the National Key Programs for Infectious Diseases of China, grant no. 2017ZX10303405 (to L.W.); the National Natural Science Foundation of China, grant no. 31820103002 (to L.W.), 31530083 (to L.W.), 31770144 (to L.W.), 32070133 (to L.F.), 81871624 (to L.F.), 31800126 (to L.J.), 31970084 (to D.H.), and 31970179 (to Z.C.); and the National Key R&D Program of China, grant no. 2018YFA0901000 (to L.F.).
Author information
Authors and Affiliations
Contributions
L.W. and L.F. designed the research; L.J., P.W., X.S., H.Z., S.M., J.W., R.L., S.M., W.L., J.Y., and X.L. performed the research; Z.C., C.Y., and D.H. provided technical support and insights; H.Z. and C.Y. assisted with the metabolomic study; L.J., P.W., X.S., and H.Z. analyzed the data; and L.W., L.F., and L.J. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Communications thanks Victor Bustamante, Nirmal Robinson, and the other, anonymous, reviewer for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, L., Wang, P., Song, X. et al. Salmonella Typhimurium reprograms macrophage metabolism via T3SS effector SopE2 to promote intracellular replication and virulence. Nat Commun 12, 879 (2021). https://doi.org/10.1038/s41467-021-21186-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-021-21186-4
- Springer Nature Limited
This article is cited by
-
Camouflaging attenuated Salmonella by cryo-shocked macrophages for tumor-targeted therapy
Signal Transduction and Targeted Therapy (2024)
-
3-Hydroxykynurenine targets kainate receptors to promote defense against infection
Nature Chemical Biology (2024)
-
Metabolism of l-arabinose converges with virulence regulation to promote enteric pathogen fitness
Nature Communications (2024)
-
Nitric oxide is a host cue for Salmonella Typhimurium systemic infection in mice
Communications Biology (2023)
-
c-di-GMP inhibits the DNA binding activity of H-NS in Salmonella
Nature Communications (2023)