Abstract
Radiation therapy (RT) remains a common treatment for cancer patients worldwide, despite the development of targeted biological compounds and immunotherapeutic drugs. The challenge in RT lies in delivering a lethal dose to the cancerous site while sparing the surrounding healthy tissues. Low linear energy transfer (low-LET) and high linear energy transfer (high-LET) radiations have distinct effects on cells. High-LET radiation, such as alpha particles, induces clustered DNA double-strand breaks (DSBs), potentially inducing cell death more effectively. However, due to limited range, alpha-particle therapies have been restricted. In human cancer, mutations in TP53 (encoding for the p53 tumor suppressor) are the most common genetic alteration. It was previously reported that cells carrying wild-type (WT) p53 exhibit accelerated senescence and significant rates of apoptosis in response to RT, whereas cells harboring mutant p53 (mutp53) do not. This study investigated the combination of the alpha-emitting atoms RT based on internal Radium-224 (224Ra) sources and systemic APR-246 (a p53 reactivating compound) to treat tumors with mutant p53. Cellular models of colorectal cancer (CRC) or pancreatic ductal adenocarcinoma (PDAC) harboring mutant p53, were exposed to alpha particles, and tumor xenografts with mutant p53 were treated using 224Ra source and APR-246. Effects on cell survival and tumor growth, were assessed. The spread of alpha emitters in tumors was also evaluated as well as the spatial distribution of apoptosis within the treated tumors. We show that mutant p53 cancer cells exhibit radio-sensitivity to alpha particles in vitro and to alpha-particles-based RT in vivo. APR-246 treatment enhanced sensitivity to alpha radiation, leading to reduced tumor growth and increased rates of tumor eradication. Combining alpha-particles-based RT with p53 restoration via APR-246 triggered cell death, resulting in improved therapeutic outcomes. Further preclinical and clinical studies are needed to provide a promising approach for improving treatment outcomes in patients with mutant p53 tumors.
Similar content being viewed by others
Introduction
Alongside many other commonly used anti-cancer strategies and despite recently developed modalities that include targeted biological compounds and immunotherapeutic drugs, most cancer patients worldwide are still treated with some form of radiation therapy (RT), either as a main treatment or as an adjuvant approach [1,2,3]. The major challenge in RT lies in the delicate balance between delivering a destructive, lethal dose into the cancerous tissue while limiting the damage to the surrounding healthy perimeters and the radiotoxicity affecting vital organs. To that end, the use of low versus high linear energy transfer (low-LET and high-LET) differs significantly [4,5,6]. While 1 Gray (Gy) dose of X-rays (low-LET) induces thousands of single-strand breaks (SSBs) to the DNA of a mammalian cell and approximately 40 double strand breaks (DSBs), as LET increases, so does cytotoxicity [7, 8]. Notably, only a few hits of alpha particles (high-LET) to the DNA can produce clustered DSBs that will drive the cell towards an apoptotic course, mainly due to their high ionization density. Clustered DSBs are repaired less efficiently than isolated damage, suggesting that high-LET radiation therapy should be more robustly used for the eradication of tumors [9, 10].
Nevertheless, the vast majority of cancer patients are subjected to low-LET (most often X-rays) RT due to the heavy mass of alpha particles leading to strong interactions with tissue and their slow movement [11, 12]. Hence, the limited range of alpha particles in tissues (less than 100μm) has traditionally been considered a limiting factor, restricting the development of alpha-particle-based therapies [13].
Radiosensitizing agents (radiosensitizers) are substances and compounds which have the capacity to augment the effect produced by RT alone [14,15,RNA and real-time quantitative PCR RNA was isolated with a mini-RNeasy kit (Qiagen, Germany) and reverse transcribed using Moloney murine leukemia virus reverse transcriptase and random hexamer primers (Promega, USA). Real-time qPCR was performed using SYBR Green Master Mix (Thermo Fisher) in a StepOnePlus instrument (Applied Biosystems). All primers were purchased from Sigma-Aldrich. Each sample was analyzed in triplicate and data were analyzed based on the comparative Ct (2 − ΔΔCt) method. The expression of target genes was normalized to GAPDH expression. The primers used in this study are detailed here: NOXA: F: 5′-GAAGGGAGATGACCTGTGATTAG-3′/R:5′-TGCTGAGTTGGCACTGAAA-3′. PUMA: F: 5′-GGA GCA GCA CCT GGA GTC / R: 5′-TA CTG TGC GTT GAG GTC GTC-3′. GAPDH: F:5′-GGTGTGAACCATGAGAAGTATGA-3′/R:5′-GAGTCCTTCCACGATACCAAAG-3′. The study was approved by the Ben-Gurion University Institutional Animal Care and Use Committee and was conducted according to the Israeli Animal Welfare Act following the guidelines of the Guide for Care and Use of Laboratory Animals (National Research Council, 1996) [permit no. IL-47-07- 2019(E)]. Male nude mice (6–12 weeks old) were obtained from Envigo, Israel. Mice were inoculated subcutaneously with 5·106 cells (for all cell lines) in 100 μl Dulbecco’s phosphate-buffered saline (DPBS and DMEM) (Gibco, 14190144, Thermo Fisher Scientific, MA, USA) into the low lateral side of the back. At the day of source insertion and before the insertion, the mice were divided into treatment groups to create a similar as possible mean tumor volume for each group. Blinding was not conducted. No human subjects were used in this study, therefore ethics and consent are not applicable. Four to five days post the 224Ra treatment, the tumors were excised (as a whole). Each tumor was cut to two halves, in the estimated location of the seed center, perpendicular to the seed’s insertion axis. The seed was then pulled out using surgical tweezers and was placed in a 1.5 ml microcentrifuge tube filled with 1 ml of water. The tumor was placed for 1 h in −80 °C. The tumors were put in 20 ml santilation bottles on dry-ice and taken for a measurement with HIDEX gamma. Subsequently, both halves of the tumor were subjected to histological sectioning by LEICA CM 1520 cryostat (Buffalo Grove, IL, USA). The 10 µm-thick sections were then placed on positively charged glass slides (76 mm by 26 mm by 1–1.2 mm), with 250–300 µm intervals between each section, creating a series of sequential sections (between 5 and 15 per tumor). Following the sectioning, slides were fixed with 4% paraformaldehyde (sc-281692, Santa Cruz Biotechnology Inc., Dallas, TX, USA) for 10 min and rinsed twice with PBS for 10 min each time. Immediately after the fixation step, slides were taken to the autoradiography system. The same histological sections measured on the imaging plate, were later stained with hematoxylin-eosin (Surgipath, Richmond, IL). The pictures were taken using a Panoramic scanner (3D HISTECH Ltd, Budapest, Hungary). Stainless steel seeds (0.1 mm in diameter, cut to a length of 6.5 mm) were loaded with 224Ra atoms (half-life of 3.7 days). To prevent Radium dissolution in the tissue fluids, the atoms were embedded a few atomic layers into the seed surface through thermal treatment. Seeds, either loaded with 224Ra or inert, were placed near the tip of an 18-gauge needle attached to a 2.5 ml syringe (Picindolor, Rome, Italy) and inserted into the tumor by a plunger placed internally along the syringe axis. The radioactive and inert seeds were inserted into the primary tumor under anesthesia with Isoflurane. Seed location was verified using a Geiger counter (RAM GENE-1, Rotem industries, Israel) after insertion process was completed and before tumor removal. Local tumor growth was determined by measuring three mutually orthogonal tumor dimensions three times per week, according to the following formula: Tumor volume = length·weight·height·π/6. Mice were pre-excluded from the study based on tumor non-uniformity criteria (too big/small tumors before source insertion, double focal tumors, internal tumors) and if the source fell in first 5 days. Tumor volume over time was assessed and compared between the groups using repeated measures ANOVA analysis. The cubic root transformed volume was modeled as a function of group, day (categorical) and the day × group interaction with baseline volume entered as a covariate. Mean (least squares means) and confidence intervals were estimated from the interaction term for each day per group and were back transformed to the volume. Survival data was depicted by a Kaplan–Meier plot; two curves were compared with a Log-rank test with p-values adjusted for multiple comparisons using the FDR method. APR-246 was purchased from Cayman Chemicals was dissolved in DPBS on the same day of the experiment. The stock was stored at −20 °C in powder condition. For the in vivo studies, APR-246 was dissolved DPBS, and 100 µl of 50 mg/kg APR-246 was injected i.p. twice a day; DPBS was used as a sham control. Treatment started 1 day after 224Ra source insertion (day 0) for a total of fourteen doses (days 1–7). The DeadEnd™ Fluorometric TUNEL System (Promega) measures the fragmented DNA of apoptotic cells by catalytically incorporating fluorescein-12-dUTP at 3′-OH DNA ends using Terminal Deoxynucleotidyl Transferase (TdT), which forms a polymeric tail using the principle of the TUNEL (TdT-mediated dUTP Nick-End Labeling) assay. The fluorescein-12-dUTP-labeled DNA can then be visualized directly by fluorescence microscopy or quantitated by flow cytometry. Imaging was done on Zeiss Cell Discovery 7 system, equipped with a Plan-Apochromat 20×/0.95 objective lens and appropriate LED and filter configuration. Subsequent image analysis was conducted in QuPath software version 0.4.4. Initially, manual annotations, delineating the cancerous regions and the position of the capsules, were created for each slide. The cancer regions (ROIs) were subdivided into 100 μm2 tiles utilizing the built-in SLIC superpixel segmentation algorithm. The mean number of superpixels within each ROI was estimated at 500 ± 75, with a mean analyzed area of 0.5 ± 0.1 mm2. Quantitative descriptors capturing the intensity of the green channel were calculated for every superpixel, followed by the visualization of the average intensities of these superpixels as a heat map superimposed onto the images. Statistical analysis was performed using GraphPad Prism 10. Preliminary assessment of normal distribution was carried out using the Shapiro-Wilk test. The Wilcoxon nonparametric test was employed to evaluate the statistical variance between the control and AFP groups. A single 224Ra seed (6.5 mm length, 0.7 mm outer diameter), carrying 3 μCi 224Ra, was inserted to the center of a mice-borne HCT116 or PANC-1 tumors. Four to five days later, the tumor was excised (as a whole) and cut in two halves, at the estimated location of the seed center, perpendicular to the seed axis. The seed was then pulled out using surgical tweezers and placed in a water-filled tube for subsequent measurement by a well-type NaI(Tl) detector (Hidex Automatic Gamma Counter). The tumor was kept for 1 h at −80 °C. It was then taken, in dry ice, for measurement in the same gamma counter to determine the 212Pb activity it contains, by focusing on the 212Pb 239 keV gamma line. The measurements of the seed and tumor activity were used to determine the 212Pb leakage probability from the tumor (i.e., the probability that a 212Pb atom released from the seeds leaks out from the tumor through the blood before its decay). Immediately after the gamma measurement, both halves of the tumor were subjected to histological sectioning using a LEICA CM 1520 cryostat (Buffalo Grove, IL, USA). Sections were cut at 250–300 μm intervals with a thickness of 10 μm, and were then placed on positively charged glass slides, fixed with 4% paraformaldehyde (sc-281692, Santa Cruz Biotechnology Inc., Dallas, TX, USA) and rinsed twice with PBS. Typically, there were 5–15 sections per tumor, spanning a length of 1.5–5 mm. Shortly after their preparation, the glass slides were placed, faced down, for a duration of 1 h, on a phosphor imaging plate (Fujifilm TR2040S) protected by a 12-μm Mylar foil and enclosed in a light-tight casing. Alpha particles emitted from the sections in the decays of 212Pb progeny atoms, 212Bi and 212Po, penetrate through the foil and deposit energy in the active layer of the phosphor imaging plate. Immediately after exposure, the plate was read out by a phosphor-imaging scanner (Fujifilm FLA-9000). The intensity (in units of photo-stimulated luminescence) was converted to 212Pb activity using suitable 212Pb calibration samples. By calculating the total area corresponding, in a given tumor section, to an asymptotic 212Bi/212Po alpha dose larger than 10 Gy, the effective diameter is defined by: deff = 2[A(DBiPo > 10 Gy)/π]1/2. The 10-Gy dose is chosen as a convenient reference for actual therapeutic alpha-particle doses that are expected to be in the range ~10–20 Gy. The same histological sections measured on the imaging plate were later stained with hematoxylin–eosin (H&E) (G-biosciences, St Louis MO, USA) for tissue damage detection. H&E staining was correlated with the activity distribution measurements. The pictures were taken using a Panoramic scanner (3D HISTECH Ltd., Budapest, Hungary). Cells were lysed with 30 µL of RIPA 1× buffer supplemented with Protease inhibitor cocktail (1:100, Thermo Fisher Scientific, Waltham, MA, USA). Protein concentration in the lysates were determined via the Pierce BCA protein assay kit (Thermo Fisher Scientific, Waltham, MA, USA). Lysates were mixed with sample buffer (5×) (Thermo Fisher Scientific, Waltham, MA, USA) and boiled at 95 °C for 10 min, loaded into gel (Invitrogen Novex WedgeWell 4 to 20%, Tris-Glycine, 1.0 mm, Mini Protein Gel, 10-well, Thermo Fisher Scientific, Waltham, MA, USA), and separated via PAGE. Proteins were then transferred into the nitrocellulose membrane (Greiner, 10-6000-02), blocked for 1 h at room temperature with 5% BSA in TBS and then followed by exposure to primary antibodies (dil 1:1000) overnight at 4 °C: anti-p53, anti-p21, and anti-GAPDH. The membranes were then washed and incubated with HRP-conjugated secondary antibody (dil 1:5000) for 1 h at room temperature, washed, and exposed to SuperSignal West Pico PLUS Chemiluminescent Substrate (Thermo Fisher Scientific, Waltham, MA, USA) as per manufacturer’s protocol before visualizing the membranes in iBrightCL1000 (Invitrogen, A32749, Carlsbad, CA, USA). Mouse Monoclonal anti-p53 (DO-1) was purchased from Santa Cruz Biotechnology, Santa Cruz, CA, USA. Mouse anti-GAPDH was purchased from Sigma-Aldrich, St. Louis, MO, USA. Anti-p21 antibody [EPR362] was purchased from abcam, Cambridge Biomedical Campus, Hills Road, Cambridge. Anti-Cleaved Caspase-3 antibody (Ab-2302) was purchased from abcam, Cambridge Biomedical Campus, Hills Road, Cambridge. All statistical tests were performed in GraphPad PRISM 8.0. and presented as the mean ± standard of measurement. Continuous variables were compared by using the Student’s t-test. Categorical variables were compared by using Chi-square (or the Fisher exact test when appropriate). No statistical methods were used to predetermine the sample size. The variance was similar between the groups that were being statistically compared. Tumor volume over time was assessed and compared between the groups using repeated measures Two-way ANOVA unless stated otherwise. Each experiment was analyzed until the time point at which the first animal died. Survival curves are depicted by a Kaplan–Meier plot and compared with a Log-rank test. A p-value < 0.05 was considered statistically significant.Tumor inoculation
Ethics approval and consent to participate
Frozen section preparation
224Radium‑loaded source preparation and insertion
Tumor volume measurements
Drug preparation, storage and administration
Spatial apoptosis assay
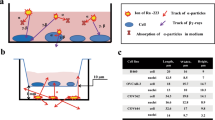
Autoradiography of 224Ra-treated tumors and 212Pb leakage probability measurements
Western blotting
Antibodies
Biostatistical analysis
Data availability
All materials described in the manuscript, including all relevant raw data, will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
Garibaldi C, Jereczek-Fossa BA, Marvaso G, Dicuonzo S, Rojas DP, Cattani F, et al. Recent advances in radiation oncology. Ecancermedicalscience. 2017;11. https://pubmed.ncbi.nlm.nih.gov/29225692/.
Gottumukkala S, Salamekh S, Sanford NN. Current state and future directions of radiation therapy for pancreas adenocarcinoma. Surg Oncol Clin N Am. 2023;32:399–414. https://pubmed.ncbi.nlm.nih.gov/37182984/.
Kumar A, Gautam V, Sandhu A, Rawat K, Sharma A, Saha L. Current and emerging therapeutic approaches for colorectal cancer: A comprehensive review. World J Gastrointest Surg. 2023;15:495–519. https://pubmed.ncbi.nlm.nih.gov/37182984/.
Nickoloff JA, Sharma N, Taylor L. Clustered DNA double-strand breaks: biological effects and relevance to cancer radiotherapy. Genes. 2020;11. https://pubmed.ncbi.nlm.nih.gov/31952359/.
Roobol SJ, van den Bent I, van Cappellen WA, Abraham TE, Paul MW, Kanaar R, et al. Comparison of high- and low-LET radiation-induced DNA double-strand break processing in living cells. Int J Mol Sci. 2020;21:1–19. https://pubmed.ncbi.nlm.nih.gov/32917044/.
Franken NAP, ten Cate R, Krawczyk PM, Stap J, Haveman J, Aten J, et al. Comparison of RBE values of high-LET α-particles for the induction of DNA-DSBs, chromosome aberrations and cell reproductive death. Radiat Oncol. 2011;6. https://pubmed.ncbi.nlm.nih.gov/21651780/.
C. Newman, K. M. Prise, B. D. Gray H. The role of higher-order chromatin structure in the yield and distribution of DNA double-strand breaks in cells irradiated with X-rays or alpha-particles. Int J Radiat Biol. 2000;76:1085–93. https://pubmed.ncbi.nlm.nih.gov/10947121/.
Claesson K, Magnander K, Kahu H, Lindegren S, Hultborn R, Elmroth K. RBE of α-particles from (211)At for complex DNA damage and cell survival in relation to cell cycle position. Int J Radiat Biol. 2011;87:372–84. https://pubmed.ncbi.nlm.nih.gov/21171940/.
Abramenkovs A, Hariri M, Spiegelberg D, Nilsson S, Stenerlöw B. Ra-223 induces clustered DNA damage and inhibits cell survival in several prostate cancer cell lines. Transl Oncol. 2022;26. https://pubmed.ncbi.nlm.nih.gov/36126563/.
Mladenova V, Mladenov E, Scholz M, Stuschke M, Iliakis G. Strong shift to ATR-dependent regulation of the G2-checkpoint after exposure to high-LET radiation. Life. 2021;11. https://pubmed.ncbi.nlm.nih.gov/34198619/.
Gianfaldoni S, Gianfaldoni R, Wollina U, Lotti J, Tchernev G, Lotti T. An overview on radiotherapy: from its history to its current applications in dermatology. Open Access Maced J Med Sci. 2017;5:521–5. https://pubmed.ncbi.nlm.nih.gov/28785349/.
Elgqvist J, Frost S, Pouget JP, Albertsson P. The potential and hurdles of targeted alpha therapy - clinical trials and beyond. Front Oncol. 2014;3. https://pubmed.ncbi.nlm.nih.gov/24459634/.
Bruland ØS, Larsen RH, Baum RP, Juzeniene A. Editorial: targeted alpha particle therapy in oncology. Front Med. 2023;10:1165747 https://pubmed.ncbi.nlm.nih.gov/36960341/.
Yang S, Han G, Chen Q, Yu L, Wang P, Zhang Q, et al. Au-Pt nanoparticle formulation as a radiosensitizer for radiotherapy with dual effects. Int J Nanomed. 2021;16:239–48. https://pubmed.ncbi.nlm.nih.gov/33469284/.
Martinel Lamas DJ, Cortina JE, Ventura C, Sterle HA, Valli E, Balestrasse KB, et al. Enhancement of ionizing radiation response by histamine in vitro and in vivo in human breast cancer. Cancer Biol Ther. 2015;16:137–48. https://pubmed.ncbi.nlm.nih.gov/25482934/.
Su M, Ren X, Du D, He H, Zhang D, **e R, et al. Curcumol β-cyclodextrin inclusion complex enhances radiosensitivity of esophageal cancer under hypoxic and normoxic condition. Jpn J Radiol. 2023. https://pubmed.ncbi.nlm.nih.gov/37227584/.
Sabbah M, Najem A, Vanderkerkhove C, Kert F, Jourani Y, Journe F, et al. The benefit of co-targeting PARP-1 and c-Met on the efficacy of radiotherapy in wild type BRAF melanoma. Front Med. 2023;10. https://pubmed.ncbi.nlm.nih.gov/37215708/
Miles X, Vandevoorde C, Hunter A, Bolcaen J. MDM2/X inhibitors as radiosensitizers for glioblastoma targeted therapy. Front Oncol. 2021;11:703442 https://pubmed.ncbi.nlm.nih.gov/34307171/.
Skinner HD, Sandulache VC, Ow TJ, Meyn RE, Yordy JS, Beadle BM, et al. TP53 disruptive mutations lead to head and neck cancer treatment failure through inhibition of radiation-induced senescence. Clin Cancer Res. 2012;18:290–300. https://pubmed.ncbi.nlm.nih.gov/22090360/.
Fernández-Aroca DM, Roche O, Sabater S, Pascual-Serra R, Ortega-Muelas M, Sánchez Pérez I, et al. P53 pathway is a major determinant in the radiosensitizing effect of Palbociclib: Implication in cancer therapy. Cancer Lett. 2019;451:23–33. https://pubmed.ncbi.nlm.nih.gov/30872077/.
Fei P, El-Deiry WS. P53 and radiation responses. Oncogene. 2003;22:5774–83. https://pubmed.ncbi.nlm.nih.gov/12947385/.
Levine AJ, Oren M. The first 30 years of p53: growing ever more complex. Nat Rev Cancer. 2009;9:749–58. https://pubmed.ncbi.nlm.nih.gov/19776744/.
Cheok CF, Verma CS, Baselga J, Lane DP. Translating p53 into the clinic. Nat Rev Clin Oncol. 2011;8:25–37. https://pubmed.ncbi.nlm.nih.gov/20975744/.
Tonnessen-Murray CA, Lozano G, Jackson JG. The regulation of cellular functions by the p53 protein: cellular senescence. Cold Spring Harb Perspect Med. 2017;7. https://pubmed.ncbi.nlm.nih.gov/27881444/.
Quick QA, Gewirtz DA. An accelerated senescence response to radiation in wild-type p53 glioblastoma multiforme cells. J Neurosurg. 2006;105:111–8. https://pubmed.ncbi.nlm.nih.gov/16871885/.
Concin N, Zeillinger C, Stimpfel M, Schiebel I, Tong D, Wolff U, et al. p53-dependent radioresistance in ovarian carcinoma cell lines. Cancer Lett. 2000;150:191–9. https://pubmed.ncbi.nlm.nih.gov/10704742/.
Lee JM, Bernstein A. p53 mutations increase resistance to ionizing radiation. Proc Natl Acad Sci USA]. 1993;90:5742–6. https://pubmed.ncbi.nlm.nih.gov/8516323/.
Okaichi K, Ide-Kanematsu M, Izumi N, Morita N, Okumura Y, Ihara M. Variations in Sensitivity to Ionizing Radiation in Relation to p53 Mutation Point. Anticancer Res [Internet]. 2008;28:2687–90. https://ar.iiarjournals.org/content/28/5A/2687.
Chen X, Zhang T, Su W, Dou Z, Zhao D, ** X, et al. Mutant p53 in cancer: from molecular mechanism to therapeutic modulation. Cell Death Dis. 2022;13. https://pubmed.ncbi.nlm.nih.gov/36400749/.
Hassin O, Oren M. Drugging p53 in cancer: one protein, many targets. Nat Rev Drug Discov. 2023;22:127–44. https://pubmed.ncbi.nlm.nih.gov/36216888/.
Bykov VJN, Eriksson SE, Bianchi J, Wiman KG. Targeting mutant p53 for efficient cancer therapy. Nat Rev Cancer. 2018;18:89–102. https://pubmed.ncbi.nlm.nih.gov/29242642/.
Foster BA, Coffey HA, Morin MJ, Rastinejad F. Pharmacological rescue of mutant p53 conformation and function. Science. 1999;286:2507–10. https://pubmed.ncbi.nlm.nih.gov/10617466/.
Bykov VJN, Issaeva N, Zache N, Shilov A, Hultcrantz M, Bergman J, et al. Reactivation of mutant p53 and induction of apoptosis in human tumor cells by maleimide analogs. J Biol Chem. 2005;280:30384–91. https://pubmed.ncbi.nlm.nih.gov/15998635/.
Bauer MR, Joerger AC, Fersht AR. 2-Sulfonylpyrimidines: Mild alkylating agents with anticancer activity toward p53-compromised cells. Proc Natl Acad Sci USA. 2016;113:5271–80. https://pubmed.ncbi.nlm.nih.gov/27551077/.
Bykov VJN, Wiman KG. Mutant p53 reactivation by small molecules makes its way to the clinic. FEBS Lett. 2014;588:2622–7. https://pubmed.ncbi.nlm.nih.gov/24768524/.
Zawacka‐Pankau J, Selivanova G. Pharmacological reactivation of p53 as a strategy to treat cancer. J Intern Med. 2015;277:248–59. https://pubmed.ncbi.nlm.nih.gov/25495071/.
Ceder S, Eriksson SE, Cheteh EH, Dawar S, Corrales Benitez M, Bykov VJN, et al. A thiol-bound drug reservoir enhances APR-246-induced mutant p53 tumor cell death. EMBO Mol Med. 2021;13. https://pubmed.ncbi.nlm.nih.gov/33314700/.
Rökaeus N, Shen J, Eckhardt I, Bykov VJN, Wiman KG, Wilhelm MT. PRIMA-1(MET)/APR-246 targets mutant forms of p53 family members p63 and p73. Oncogene. 2010;29:6442–51. https://pubmed.ncbi.nlm.nih.gov/20818419/.
Maslah N, Salomao N, Drevon L, Verger E, Partouche N, Ly P, et al. Synergistic effects of PRIMA-1Met (APR-246) and 5-azacitidine in TP53-mutated myelodysplastic syndromes and acute myeloid leukemia. Haematologica. 2020;105:1539–51. https://pubmed.ncbi.nlm.nih.gov/31488557/.
Liu DSH, Read M, Cullinane C, Azar WJ, Fennell CM, Montgomery KG, et al. APR-246 potently inhibits tumour growth and overcomes chemoresistance in preclinical models of oesophageal adenocarcinoma. Gut. 2015;64:1506–16. https://pubmed.ncbi.nlm.nih.gov/26187504/.
Liang Y, Besch-Williford C, Cook MT, Belenchia A, Brekken RA, Hyder SM. APR-246 alone and in combination with a phosphatidylserine-targeting antibody inhibits lung metastasis of human triple-negative. breast cancer cells in nude mice. Breast Cancer. 2019;11:249–59. https://pubmed.ncbi.nlm.nih.gov/31534364/.
**e X, Fan C, Luo B, Zhang J, Jensen LD, Burman J, et al. APR-246 Enhances Colorectal Cancer Sensitivity to Radiotherapy. Mol Cancer Ther. 2023;22. https://pubmed.ncbi.nlm.nih.gov/37216282/.
Cooks T, Pateras IS, Jenkins LM, Patel KM, Robles AI, Morris J, et al. Mutant p53 cancers reprogram macrophages to tumor supporting macrophages via exosomal miR-1246. Nat Commun. 2018;9:771. https://pubmed.ncbi.nlm.nih.gov/29472616/.
Sur S, Pagliarini R, Bunz F, Rago C, Diaz LA, Kinzler KW, et al. A panel of isogenic human cancer cells suggests a therapeutic approach for cancers with inactivated p53. Proc Natl Acad Sci USA. 2009;106:3964–9. https://pubmed.ncbi.nlm.nih.gov/19225112/.
Nishri Y, Vatarescu M, Luz I, Epstein L, Dumančić M, Del Mare S, et al. Diffusing alpha-emitters radiation therapy in combination with temozolomide or bevacizumab in human glioblastoma multiforme xenografts. Front Oncol. 2022;12:888100 https://pubmed.ncbi.nlm.nih.gov/36237307/.
Trencsényi G, Csikos C, Képes Z. Targeted radium alpha therapy in the era of nanomedicine: in vivo results. Int J Mol Sci. 2024;25:664.
Arazi L, Cooks T, Schmidt M, Keisari Y, Kelson I. Treatment of solid tumors by interstitial release of recoiling short-lived alpha emitters. Phys Med Biol. 2007;52:5025–5042. https://iopscience.iop.org/article/10.1088/0031-9155/52/16/021.
Cooks T, Arazi L, Schmidt M, Marshak G, Kelson I, Keisari Y. Growth retardation and destruction of experimental squamous cell carcinoma by interstitial radioactive wires releasing diffusing alpha-emitting atoms. Int J Cancer. 2008;122:1657–64. https://pubmed.ncbi.nlm.nih.gov/18059026/.
Lazarov E, Arazi L, Efrati M, Cooks T, Schmidt M, Keisari Y, et al. Comparative in vitro microdosimetric study of murine- and human-derived cancer cells exposed to alpha particles. Radiat Res. 2012;177:280–7. https://pubmed.ncbi.nlm.nih.gov/22077335/.
Cooks T, Arazi L, Efrati M, Schmidt M, Marshak G, Kelson I, et al. Interstitial wires releasing diffusing alpha emitters combined with chemotherapy improved local tumor control and survival in squamous cell carcinoma-bearing mice. Cancer. 2009;115:1791–801. https://pubmed.ncbi.nlm.nih.gov/19197995/.
Cooks T, Schmidt M, Bittan H, Lazarov E, Arazi L, Kelson I, et al. Local control of lung derived tumors by diffusing alpha-emitting atoms released from intratumoral wires loaded with radium-224. Int J Radiat Oncol Biol Phys. 2009;74:966–73. https://pubmed.ncbi.nlm.nih.gov/19480976/.
Popovtzer A, Rosenfeld E, Mizrachi A, Bellia SR, Ben-Hur R, Feliciani G, et al. Initial safety and tumor control results from a “first-in-human” multicenter prospective trial evaluating a novel alpha-emitting radionuclide for the treatment of locally advanced recurrent squamous cell carcinomas of the skin and head and neck. Int J Radiat Oncol Biol Phys. 2020;106:571–8. https://doi.org/10.1016/j.ijrobp.2019.10.048.
Bhatta B, Luz I, Krueger C, Teo FX, Lane DP, Sabapathy K, et al. Cancer cells shuttle extracellular vesicles containing oncogenic mutant p53 proteins to the tumor microenvironment. Cancers. 2021;13. https://pubmed.ncbi.nlm.nih.gov/34203762/.
Mukherjee S, Maddalena M, Lü Y, Martinez S, Nataraj NB, Noronha A, et al. Cross-talk between mutant p53 and p62/SQSTM1 augments cancer cell migration by promoting the degradation of cell adhesion proteins. Proc Natl Acad Sci USA. 2022;119:2119644119 https://pubmed.ncbi.nlm.nih.gov/35439056/.
Abrams SL, Duda P, Akula SM, Steelman LS, Follo ML, Cocco L, et al. Effects of the mutant TP53 reactivator APR-246 on therapeutic sensitivity of pancreatic cancer cells in the presence and absence of WT-TP53. Cells. 2022;11. https://pubmed.ncbi.nlm.nih.gov/35269416/.
Heger G, Roy A, Dumančić M, Arazi L. Alpha dose modeling in diffusing alpha-emitters radiation therapy-Part I: single-seed calculations in one and two dimensions. Med Phys. 2023;50:1793–811. https://pubmed.ncbi.nlm.nih.gov/36464914/.
Heger G, Dumančić M, Roy A, Arazi L. Alpha dose modeling in diffusing alpha-emitters radiation therapy. Part II: Lattice studies. Med Phys. 2023;50:1812–23. https://pubmed.ncbi.nlm.nih.gov/36517936/.
Tada M, Matsumoto R, Iggo RD, Onimaru R, Shirato H, Sawamura Y, et al. Selective sensitivity to radiation of cerebral glioblastomas harboring p53 mutations. http://aacrjournals.org/cancerres/article-pdf/58/9/1793/2469488/cr0580091793.pdf.
Cheng G, Kong D, Hou X, Liang B, He M, Liang N, et al. The tumor suppressor, p53, contributes to radiosensitivity of lung cancer cells by regulating autophagy and apoptosis. Cancer Biother Radiopharm. 2013;28:153–9. https://pubmed.ncbi.nlm.nih.gov/23268708/.
Morita A, Wang B, Tanaka K, Katsube T, Murakami M, Shimokawa T, et al. Protective effects of p53 regulatory agents against high-LET radiation-induced injury in mice. Front Public Health. 2020;8. https://pubmed.ncbi.nlm.nih.gov/33344403/.
Anbalagan S, Ström C, Downs JA, Jeggo PA, McBay D, Wilkins A, et al. TP53 modulates radiotherapy fraction size sensitivity in normal and malignant cells. Sci Rep. 2021;11. https://pubmed.ncbi.nlm.nih.gov/33782505/.
Birsen R, Larrue C, Decroocq J, Johnson N, Guiraud N, Gotanegre M, et al. APR-246 induces early cell death by ferroptosis in acute myeloid leukemia. Haematologica. 2022;107:403–16. https://pubmed.ncbi.nlm.nih.gov/33406814/.
Tessoulin B, Descamps G, Moreau P, Maïga S, Lodé L, Godon C, et al. PRIMA-1Met induces myeloma cell death independent of p53 by impairing the GSH/ROS balance. Blood. 2014;124:1626–36. https://pubmed.ncbi.nlm.nih.gov/25006124/.
Duffy MJ, Tang M, Rajaram S, O'grady S, Crown J. Targeting mutant p53 for cancer treatment: moving closer to clinical use? Cancers. 2022;14. https://pubmed.ncbi.nlm.nih.gov/36139658/.
Kobayashi T, Makino T, Yamashita K, Saito T, Tanaka K, Takahashi T, et al. APR-246 induces apoptosis and enhances chemo-sensitivity via activation of ROS and TAp73-Noxa signal in oesophageal squamous cell cancer with TP53 missense mutation. Br J Cancer. 2021;125:1523–32. https://pubmed.ncbi.nlm.nih.gov/34599296/.
Sobhani M, Abdi J, Manujendra SN, Chen C, Chang H. PRIMA-1Met induces apoptosis in Waldenström’s Macroglobulinemia cells independent of p53. Cancer Biol Ther. 2015;16:799–806. https://pubmed.ncbi.nlm.nih.gov/25803193/.
Saha MN, Jiang H, Yang Y, Reece D, Chang H. PRIMA-1Met/APR-246 displays high antitumor activity in multiple myeloma by induction of p73 and noxa. Mol Cancer Ther. 2013;12:2331–41. https://mct.aacrjournals.org/content/12/11/2331.
Lim B, Greer Y, Lipkowitz S, Takebe N. Novel Apoptosis-inducing agents for the treatment of cancer, a new arsenal in the toolbox. Cancers. 2019;11. https://pubmed.ncbi.nlm.nih.gov/31370269/.
Baig S, Seevasant I, Mohamad J, Mukheem A, Huri HZ, Kamarul T. Potential of apoptotic pathway-targeted cancer therapeutic research: Where do we stand? Cell Death Dis. 2016;7:e2058. https://pubmed.ncbi.nlm.nih.gov/26775709/.
Pratz KW, Jonas BA, Pullarkat V, Recher C, Schuh AC, Thirman MJ, et al. Measurable residual disease response and prognosis in treatment-naïve acute myeloid leukemia with venetoclax and azacitidine. J Clin Oncol. 2022;40:855–65. https://pubmed.ncbi.nlm.nih.gov/34910556/.
Pemmaraju N, Garcia JS, Potluri J, Harb JG, Sun Y, Jung P, et al. Addition of navitoclax to ongoing ruxolitinib treatment in patients with myelofibrosis (REFINE): a post-hoc analysis of molecular biomarkers in a phase 2 study. Lancet Haematol. 2022;9:e434–44. https://pubmed.ncbi.nlm.nih.gov/35576960/.
Morita S, Minami H, Mitsuma A, Toyoda M, Kiyota N, Ando Y. A phase I study of LCL161, a novel oral pan-inhibitor of apoptosis protein (IAP) antagonist, in Japanese patients with advanced solid tumors. Asia Pac J Clin Oncol. 2022;18:427 https://pubmed.ncbi.nlm.nih.gov/35098674/.
Hassin O, Nataraj NB, Shreberk-Shaked M, Aylon Y, Yaeger R, Fontemaggi G, et al. Different hotspot p53 mutants exert distinct phenotypes and predict outcome of colorectal cancer patients. Nat Commun. 2022;13:2800 https://pubmed.ncbi.nlm.nih.gov/35589715/.
Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–5. https://pubmed.ncbi.nlm.nih.gov/22930834/.
Acknowledgements
This work was partially supported by the Cooperation Program in Cancer Research of the Deutsches Krebsforschungszentrum (DKFZ) and Israel’s Ministry of Science and Technology (MOST), # 17802 (CA 201). This work was also partially supported by the Israeli Cancer Association (ICA), grant # 20231134.
Author information
Authors and Affiliations
Contributions
OM conducted most of the experiments and helped with structuring and writing the manuscript. IL, MV and TM assisted in the in vitro irradiation experiments and in vivo inoculations of tumors, measurements, and processing of tissues. NW analyzed the results in Fig. 5, YK analyzed the results in Fig. 1, AT processed and helped analyze the results in Fig. 6, AB consulted and help conducting apoptosis assays in the manuscript, LA helped designing the experimental set-up from a physics perspective, supervised the analysis in Figs. 1 and 5 and helped writing the manuscript, TC conceived the study, constructed the experimental set-up, helped and various analyses and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
MV is an employee of Alpha Tau Medical. TC and LA are minor shareholders in Alpha Tau Medical and hold stock options. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Ivano Amelio
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Michaeli, O., Luz, I., Vatarescu, M. et al. APR-246 as a radiosensitization strategy for mutant p53 cancers treated with alpha-particles-based radiotherapy. Cell Death Dis 15, 426 (2024). https://doi.org/10.1038/s41419-024-06830-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41419-024-06830-3
- Springer Nature Limited