Abstract
Kawasaki disease (KD), described as “mucocutaneous lymph node syndrome”, affects infants and toddlers. Patients with KD suffer from an inflammatory cascade leading to vasculitis with a predilection for coronary arteries. While the symptoms and pathogenesis of KD have received more and more attention, the precise mechanisms are still debated. Researches show that endothelial dysfunction process in KD leads to arterial damage and affect clinical outcome. In this study, we constructed a Candida albicans water soluble fraction (CAWS)-induced KD murine model and penetrated investigating the mechanisms behind endothelial dysfunction. CAWS-induced mice presented remarkably elevated vascular endothelial cell growth factor (VEGF) levels. Abundant expression of VEGF was documented in all vessels that showed edema from acute KD. It has been reported that Platelet-derived growth factor (PDGF) co-expression normalizes VEGF-induced aberrant angiogenesis. Hyperexpression of PDGFRβ was induced in the thickened medial layer and vascular endothelium of KD mice. Masitinib (Mas) is an oral tyrosine kinase inhibitor of numerous targets, which can selectively target PDGFR signaling. We set out to explore whether Mas could regulate coronary pathology in KD. Mas administration significantly reduced the VEGF-induced endothelial cells migration. NOX4 was activated in vascular endothelial cells to produce more ROS. Mitochondrial dysregulated fission and mitophagy caused by DRP-1 overexpression precipitated the arterial endothelial cells injury. Here, mitophagy seemed to work as the driving force of DRP-1/Bak/BNIP3-dependent endothelial cells apoptosis. In summary, how mitophagy is regulated by DRP-1 under pathologic status is critical and complex, which may contribute to the development of specific therapeutic interventions in cardiovascular diseases patients, for example Masatinib, the inhibitor of PDGFRβ.

Facts and questions
-
Kawasaki disease causing systemic vasculitis, affects infants and toddlers.
-
Coronary artery injury remains the major causes of morbidity and mortality.
-
DRP-1 overexpression induces DRP-1/Bak/BNIP3-dependent endothelial cells apoptosis.
-
PDGFRβ was high-expressed in the thickened medial layer of CAWS-induced KD mice.
-
Inhibition of PDGFRβ signaling alleviates arterial endothelial cells injury.
Similar content being viewed by others
Introduction
Kawasaki disease (KD), which was described as “mucocutaneous lymph node syndrome”, affects infants and toddlers, and causes systemic vasculitis [1, 2]. When initially described, it was considered as a benign disease with self-limiting course [3, 4] and the potential for coronary artery complications of KD was not appreciated. Autopsy studies later revealed the relevance between coronary artery complications and KD [2]. Over time, it has now been realized that KD may cause several other cardiac complications as well [5]. Coronary artery aneurysms may develop nearly one-quarter of all cases, to make matters worse, their development is clinically silent in most cases and may be recognized only years later at the time of sudden death or myocardial infarction [6, 7]. Coronary and peripheral artery injury remain the major causes of morbidity and mortality, despite current medical and surgical options.
While the symptoms and pathogenesis of KD have received more and more attention, the precise mechanisms are still debated. Activation of the immune system is a central feature of KD, and concentrations of many pro-inflammatory cytokines and chemokines, including tumor necrosis factor α (TNF-α), interleukins (IL) 1, 6, and 18, are higher than normal during the acute phase of the disease [2]. The leading hypothesis is a prevalent infectious trigger producing a clinically significant inflammatory disease within a genetically susceptible host [8]. Whatever the inciting factor, patients with KD suffer from an inflammatory cascade leading to vasculitis with a predilection for coronary arteries. Coronary dilatation and aneurysms then develop over weeks. This inflammatory insult produces endothelial dysfunction and increased vascular permeability. Endothelial dysfunction promotes vasoconstriction and increases susceptibility to thrombogenesis by accelerated platelet aggregation, hypercoagulability, and hypofibrinolysis. Beyond that, endothelial dysfunction is closely related to the risk factors for atherosclerosis, it is necessary to longitudinally evaluate systemic endothelial function in KD patients.
Activate monocytes/macrophages seem to have an important role in KD, which have been found in the vessel walls of patients who died and in skin biopsy samples from patients in the acute phase of the disease [9,10,11]. Skin biopsy samples in KD demonstrates gap formation and fenestration of endothelial cells, inducing perivascular edematous changes [12]. Vascular endothelial cell growth factor (VEGF) is the most potent angiogenic factor produced by endothelial cells, fibroblasts, T cells, and macrophages, plays an important role in exacerbating angiogenesis and inflammation [13]. It induces normal or aberrant angiogenesis depending on its dose in the microenvironment around each producing cell in vivo. As one candidate, high concentrations of VEGF increased vascular permeability, which could be the cause of the edema in the vessel wall [2, 12]. Abundant expression of VEGF was documented immunohistochemically in all vessels that showed edema from acute KD [14]. Another cytokine, platelet-derived growth factor (PDGF), which plays a critical role in blood vessel formation during embryonic life [15, 16]. PDGF is a major mitogen for many cell types of mesenchymal origin and is regulated by effectors in pathogenic pathways, such as thrombin, TNF-α, IL-6, and high glucose [17]. It has been reported that PDGF co-expression normalizes VEGF-induced aberrant angiogenesis [18]. The switch from normal to aberrant angiogenesis does not depend exclusively on VEGF dose, but rather on the balance between endothelial stimulation by VEGF and pericyte recruitment by PDGF, such that PDGF codelivery ensures normal and functional microvascular growth despite high or uncontrolled VEGF expression. VEGF promotes endothelial cell growth, while PDGF stabilizes blood vessels by recruiting pericytes [19].
PDGF acts on cells by binding to homo- or heterodimers of the two PDGF receptor (PDGFR) proteins, PDGFRα and PDGFRβ. Binding of ligand to PDGFRβ induces its dimerization and autophosphorylation, which initiate a number of signal transduction pathways [20]. PDGFRβ is expressed in mesenchyme, particularly in vascular smooth muscle cells (VSMCs) and pericytes. PDGFRβ and its downstream pathways play prominent role in multiple cellular functions, including proliferation, migration, matrix deposition, and immediate early gene induction [21]. In inflammatory microenvironment, PDGF /PDGFRβ and the downstream Src-Akt signal pathway control mesenchymal stem cells migration [22]. Human natural killer cells express high levels of PDGFRβ to elevate survival following IL-15 stimulation [23]. It has also been reported that PDGFRβ participated in KD vascular injury. Functional miR-223, which was delivered by hyperactive platelets isolated from patients with KD, promoted VSMC differentiation via downregulation of PDGFRβ [45]. The cytosolic GTPase dynamin-related protein 1 (DRP-1) is the main pro-fission protein with activity that is tightly controlled to ensure balanced mitochondrial dynamics according to cellular needs [45]. All these findings indicate a close relationship between mitochondrial dynamics in CVDs and DRP-1-induced mitochondrial fragmentation. Since mitochondrial fragmentation is often observed when cells are under stress or when they are dying, DRP-1 has been implicated in the pathogenesis of cell death [46]. In this study, we demonstrated the overexpression of DRP-1 in aorta of KD murine model (Fig. 5F, G). When the DRP-1 was hyperexpression in the LPS-induced endothelial injury model, Mas administration could restrain DRP-1 content (Fig. 5H–J). NOX4-related DRP-1 hyperexpression was demonstrated by the colocalization of NOX4 and DRP-1 in aorta (Fig. 5K). This DRP-1-dependent mitochondrial dysfunction caused by NOX4-mediated mitochondria dysregulated fission was described in a graphical representation (Fig. 5L).
Activation of HIF-1α/BNIP3 signaling pathway in artery of KD murine model
Mitochondria are maternally inherited multifunctional organelles that can rapidly adjust to meet the metabolic needs of the cell. They play a vital role in bioenergetic and biosynthetic pathways by an intricate balance between fission and fusion, mitochondrial biogenesis, and mitophagy. Mitochondrial damage can induce ROS production, and ROS oxidative stress can regulate mitochondrial autophagy by regulating hypoxia inducible factor 1α (HIF-1α). Bcl-2 19-kDa interacting protein 3 (BNIP3) localizes to mitochondria when overexpressed, thus, BNIP3 is a proapoptotic protein that may function through a mitochondrial pathway. It has been confirmed that BNIP3 is the target molecule of HIF-1α induced by hypoxia or ischemia, and subsequently induces mitochondrial autophagy. In this study, we demonstrated the high expression of HIF-1α in aorta (Fig. 6A) and coronary artery (Fig. 6B) of KD model mice. At the same time, the BNIP3 up-regulation was demonstrated in aorta (Fig. 6C) and coronary artery (Fig. 6D).
A Representative immumohistochemical images for HIF-1α expression in aorta (n = 4 per group). Enlarged images of area of interesting (AOI) were indicated with red block diagrams. Scale bar: 50 μm. B Representative immumohistochemical images for HIF-1α expression in coronary bifurcation arteritis (n = 4 per group). Scale bar: 50 μm. C Representative immumohistochemical images for BNIP3 expression in aorta (n = 4 per group). Enlarged images of area of interesting (AOI) were indicated with red block diagrams. Scale bar: 50 μm. D Representative immumohistochemical images for BNIP3 expression in coronary bifurcation arteritis (n = 4 per group). Scale bar: 50 μm.
DRP-1-dependent segregation of damaged mitochondria promotes mitophagy for degradation
It is generally believed that healthy mitochondria can restore mitochondrial membrane potential levels and participate in the fusion-fission cycle, whereas mitochondria that fail to do so are marked and eliminated by mitophagy. Elimination of damaged mitochondria by mitochondria-targeted selective autophagy, “mitophagy”. If damage accumulates in mitochondria, the mitochondria are aggregated and segregated by fission, followed by elimination of the damaged mitochondria via mitophagy. Considering the essential role of DRP-1 in mediating mitochondrial fission and the overexpression in the aorta of our KD murine model, we next examined the mitophagy level of artery. We confirmed the high expression of BNIP3 and colocalization with LC3B (Fig. 7A). DRP-1 promotes mitophagy in many cell types in response to different types of stress. It has been reported that inhibition of DRP-1-mediated mitochondrial fission prevents Parkin-induced mitophagy in HeLa cells [47]. The BNIP3 induces mitochondrial translocation of DRP-1, which in turn promotes translocation of Parkin to mitochondria in a DRP-1-dependent manner in adult cardiomyocytes [48]. It follows then that DRP-1 is required for BNIP3-induced mitophagy by inducing mitochondrial fission and recruitment of Parkin in a coordinated manner [49]. Double immunofluorescent staining revealed colocalization of LC3B and Parkin proteins in the aorta of KD model murine (Fig. 7B). The level of mitophagy was examined by double-labeled with LC3B and p62 (Fig. 7C), meanwhile LAMP1 and TOMM20 (Fig. 7D). The excessive mitophagy within the aorta of KD mice without suspense. The LPS-induced endothelial injury model was also applied to observed the mitophagy. In model group, the BNIP3L/NIX, PINK1 and Parkin were increased in varying degrees, and Mas could inhibit these upregulations remarkably (Fig. 7E–H). DRP-1-dependent segregation of damaged mitochondria promotes mitophagy for degradation was described in a graphical representation (Fig. 7I).
A Representative immunofluorescence images for colocalization of BNIP3 (green) and LC3B (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. B Representative immunofluorescence images for colocalization of Parkin (green) and LC3B (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. C Representative immunofluorescence images for double-labeling of p62 (green) and LC3B (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. D Representative immunofluorescence images for double-labeling of LAMP1 (green) and TOMM20 (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. E–H HUVECs were pre-treated with Mas (3 μM) for 2 h and then, LPS was applied to induce inflammatory injury together with Mas for another 48 h. Model group was treated with LPS only for 48 h. Representative western blot analysis to determine the proteins expression of BNIP3L/Nix, PINK1, and Parkin in HUVEC cells. One-way ANOVA was followed by post hoc Tukey’s test. #P < 0.05, ##P < 0.01, ###P < 0.001, vs model group. I DRP-1-dependent segregation of damaged mitochondria promoting mitophagy for degradation was described in a graphical representation.
DRP-1 associates with Bak at mitochondrial fission sites to induce cytochrome c release
Mitochondrial division creates small mitochondria, and mitochondrial fusion produces large mitochondria. Under pathological conditions, significantly larger or smaller mitochondria have been observed. It has been reported that mitophagy involves DRP-1, which generates small mitochondria and allows autophagosomes to efficiently engulf the organelle. Too much mitochondrial fission negatively affects mitochondrial function, stimulating mitochondrial biogenesis could compensate for the deleterious effects [50]. Comprehensive consideration of literature reports of the protective role of mitophagy, we presumed that the healthy mitochondrial fraction after mitochondrial fission then fused each other, allowing mitochondria to compensate for one another’s defects, maintain the membrane potential, complement protein components, and complete mtDNA repair. However, OPA1 (Fig. 8A, B) and mitochondrial fusion protein (Mfn1/2) expression (Fig. 8C), in LPS-induced endothelial injury model or aorta of KD murine model were free from influence, under Mas treatment or not. It has been reported that DRP-1 associated with Bax/Bak at mitochondrial fission sites during apoptosis in HeLa cells [51] and controlled cell death by acting downstream of Bax/Bak translocation but upstream of cytochrome c release [52]. The combination of Bak with DRP-1 was examined by double-labeling immunofluorescence (Fig. 8D), and downstream cytochrome c release (Fig. 8E). In LPS-induced endothelial injury model, the cytochrome c and cleaved caspase 3 were upregulated obviously and Mas could reverse this increasement (Fig. 8F–I).
A, B HUVECs were pre-treated with Mas (3 μM) for 2 h and then, LPS was applied to induce inflammatory injury together with Mas for another 48 h. Model group was treated with LPS only for 48 h. Representative western blot analysis to determine the proteins expression of OPA1 in HUVEC cells. C Representative immunofluorescence images for detecting Mfn1/2 (red), DAPI (blue) (n = 4 per group). Scale bar: 50 μm. D Representative immunofluorescence images for colocalization of DRP-1 (green) and Bak (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. E Representative immunofluorescence images for colocalization of TOMM20 (green) and cytochrome c (red) expressions of aorta, DAPI (blue) (n = 4 per group). Scale bar: 50 μm. F–I HUVECs were pre-treated with Mas (3 μM) for 2 h and then, LPS was applied to induce inflammatory injury together with Mas for another 48 h. Model group was treated with LPS only for 48 h. Representative western blot analysis to determine the proteins expression of Bax, cytochrome c and cleaved-caspase 3 in HUVEC cells. J Representative immumohistochemical images for E2F3 expression in aorta (n = 4 per group). Enlarged images of area of interesting (AOI) were indicated with red block diagrams. Scale bar: 50 μm. K Representative immumohistochemical images for E2F3 expression in coronary bifurcation arteritis (n = 4 per group). Scale bar: 50 μm. L Representative immumohistochemical images for p53 expression in aorta (n = 4 per group). Enlarged images of area of interesting (AOI) were indicated with red block diagrams. Scale bar: 50 μm. M Representative immumohistochemical images for p53 expression in coronary bifurcation arteritis (n = 4 per group). Scale bar: 50 μm. N The schematic diagram describes the mitophagy which seems to work as the driving force of DRP-1/Bak/BNIP3-dependent endothelial cells apoptosis. One-way ANOVA was followed by post hoc Tukey’s test. **P < 0.01, ***P < 0.001, vs ctrl group, #P < 0.05, ###P < 0.001, vs model group.
Many studies have demonstrated that E2F family transcription factors play important regulatory roles in the cardiovascular system. It is closely related to the function of vascular endothelial cells and cardiomyocytes, whose dysfunction may be associated with the pathogenesis of various cardiovascular diseases. Among this factors, E2F3 knockout mice have dysplasia or congestive heart failure, indicating that E2F3 plays an important role in the development of the cardiovascular system or maintenance of its normal functions. In addition to inducing cellular proliferation, the overexpression of E2F can also trigger cells to undergo apoptosis. There is considerable evidence to suggest that this can occur through both p53-dependent and p53-independent mechanisms [53, 54]. E2F3 is a mediator of DNA damage-induced apoptosis [55]. In this study, we examined the E2F3 expression in aorta and small coronary artery. In comparison to vehicle mice, CAWS-induced mice presented elevated E2F3 levels in VECs. Mas administration significantly reduced the E2F3 expression in CAWS-triggered murine models of KD (Fig. 8J, K). The high expression of E2F3 induced p53 activation of endothelial cells (Fig. 8L, M). Here, the mitophagy seems to work as the driving force of DRP-1/Bak/BNIP3-dependent endothelial cells apoptosis, shown in the schematic diagram (Fig. 8N).
Discussion
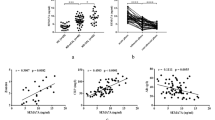
Kawasaki disease (KD) is an acute inflammatory syndrome of unknown etiology that is now a common cause of acquired heart disease in children. Chronic inflammation (vasculitis) due to KD might cause vascular cellular senescence and vascular endothelial cell damage, and is a potential cause of myocardial ischemia in young adults in young adults [56]. Coronary artery involvement is considered a specific criterion supportive of the diagnosis of KD, particularly for those patients who do not meet the full clinical criteria for a diagnosis of complete KD. The coronary artery abnormalities associated with KD can be differentiated from lesser degrees of dilation that may be rarely present with other febrile illnesses. Furthermore, several non-coronary complications have also been identified in this condition [7]. Pathological outcomes of coronary artery damage depend on the severity of the lesions. During KD coronary vasculopathy, the microenvironment of the damaged area is changed and inflammatory response is activated. Compared with the vehicle group, the spleen of our CAWS-induced KD model mice was enlarged and black in color (Fig. 1B). We examined the serum levels of pro-inflammatory cytokines, CAWS-induced mice presented remarkably elevated IL-1β, IL-6, IL-18 and TNF-α levels (Fig. 1C–F). In our CAWS-induced KD mice model, the typical pathological changes of KD vasculitis and cardiac injury were successfully induced (Fig. 1I–M). Considering the vital role of PDGF in pathogenesis of vascular damage in KD, in this experiment, the expression of its receptor, PDGFRβ was examined. Hyperexpression of PDGFRβ was induced in the thickened medial layer of CAWS-induced KD mice (Fig. 1G, H). Furthermore, VSMCs dedifferentiated to macrophage-like cells, with the reduced expression of the VSMCs differentiation markers (α-SMA) (Fig. 2A, B), and the increased expression of VSMC dedifferentiation markers (OPN) co-expressed with PDGFRβ (Fig. 2C, D), and expressed macrophage foam cell markers, such as MOMA-2 (Fig. 2E, F), F4/80 (Fig. 2G, H). Mas, the inhibitor of PDGFRβ, could ameliorate these cardiac and vascular inflammation.
When the vascular structure is damaged, the inner cortex is destroyed firstly. KD-like vasculitis impaired vascular endothelial cells that produce eNOS, which maintains vascular homeostasis, and promoted macrophage infiltration into the tissue [57]. eNOS, which is expressed specifically in vascular endothelial cells, is primarily associated with the production of the vasoactive substance NO, and is an important factor when assessing endothelial cell function. CAWS vasculitis has also been speculated to induce cellular senescence of vascular endothelial cells, leading to suppression of eNOS. Previous studies have shown that eNOS is activated via the Rho/ROCK pathway. Inhibition of Rho/ROCK pathway can restrain eNOS expression. The induction processes that stimulate expression of the inducible NOS (iNOS) have also been shown to downregulate the expression of the eNOS [34]. As a major mediator of inflammation, iNOS plays an important role in cardiovascular pathophysiology through its elevated activity and inducement of excess NO production. We examined endothelial function after the onset of KD, the dysfunction represented by the decrement of eNOS and CD31 in KD model group, furthermore, the increasement of iNOS at the same time (Fig. 3A–D). It has been reported that VEGF is an important factor in mediating the inflammation of KD. The literature regarded the relationship between VEGF and KD very exhaustively. KD patients with acute coronary artery lesions (CALs) had higher median VEGF levels than those without acute CALs from acute to convalescent phases. In the subacute phase, KD patients with acute CALs had significantly higher VEGF levels than those without acute CALs. VEGF did not decrease after IVIG treatment, and increased significantly after IVIG treatment in KD patients with acute CALs in acute phase. VEGF might be related to the complications of CALs in KD patients [13]. However, VEGF delivery alone may act as a negative regulator of vessel maturation [58], which is determined by pericyte recruitment mainly controlled by PDGF-BB [59]. Moreover, a recent clinical study shows a greater therapeutic efficacy by dual antagonism of PDGF and VEGF in treating age-related macular degeneration. PDGF in the tumor microenvironment activates PDGF receptor in ECs, which in turn induces NF-κB-dependent Snail expression, thereby inducing endothelial-mesenchymal transformation [60]. The roles of VEGF in acute KD may also involve promotion of vascular permeability and macrophage activation. VEGF also enhances proliferation and migration of endothelial cells in collaboration with NO and may contribute to later vascular remodeling after the acute phase of KD [14, 61]. In this study, VEGF levels in aorta and coronary artery were examined. In comparison to vehicle mice, CAWS-induced mice presented remarkably elevated VEGF levels. Mas administration significantly reduced the VEGF expression in CAWS-triggered murine models of KD (Fig. 3E, F). Furthermore, we demonstrated that treatment with different concentrations of Mas inhibited the migration of VECs (Fig. 4A–C), and VEGF-induced VECs migration (Fig. 4D–F) by inhibiting the activation of RhoA/ROCK1 pathway (Fig. 4G–M). The source of ROS in phagocytes is the NOX, an enzyme complex composed of membrane-bound and cytosolic subunits. NOX is a key source of oxidative stress in human arteries, for example, NOX1 is responsible for angiotensin II- and PDGF-stimulated ROS- production in rat aortic VSMCs [62]. The NOX4-dependent effects that induced vascular dysfunction may not mirror the role of this homolog in heart failure [42]. Here, we explored that NOX4 were upregulated in CAWS-triggered KD murine models and Mas reversed this increase (Fig. 5A, B). Microscopic analysis demonstrated a significant increase of ROS by LPS in HUVECs. Mas or NOX4 inhibitor GKT137831 can inhibit this production of ROS (Fig. 5C). JC-10 dye indicated a lower mitochondrial membrane potential by LPS (Fig. 5D) and mitochondrial morphological change examined by TEM (Fig. 5E).
Mitochondria exist as a dynamic coordinated network. In addition to ATP production, mitochondria regulate cell death and survival by integrating a range of cellular signals are also the primary source of ROS, which can trigger oxidative stress, thereby affecting cell survival and death. They maintain a healthy pool by constant fusion and fission [63], repair, sequestration or degradation via mitophagy or mitophagy-independent mechanisms [64], and biogenesis. DRP-1-mediated mitochondrial dynamics play crucial roles in mitochondrial quality control in the heart. It has been reported that the detrimental effects of excessive mitochondrial fission can be reversed by drugs targeting DRP-1 [43]. In this study, the DRP-1 was excessively expressed in the aorta of KD murine model and in the LPS-induced endothelial injury model. Mas administration could target DRP-1 to inhibit mitochondrial fragmentation (Fig. 5F–J). NOX4-related DRP-1 hyperexpression was demonstrated by the colocalization of NOX4 and DRP-1 in aorta (Fig. 5K). Mitochondrial damage can induce ROS production, and ROS oxidative stress can regulate mitochondrial autophagy by regulating HIF-1α. The activation of ROS-HIF-1α pathway promotes pulmonary artery smooth muscle cells proliferation, ultimately leads to pulmonary vascular remodeling [65]. It has been confirmed that BNIP3 is the target molecule of HIF-1α induced by hypoxia or ischemia, and subsequently induces mitochondrial autophagy [66]. Within the aorta and coronary artery of KD model mice exhibited upregulated levels of HIF-1α (Fig. 6A, B), downstream BNIP3 (Fig. 6C, D), and LC3B, as well as enhanced colocalization of LC3B with BNIP3 (Fig. 7A) and the activation of Parkin/LC3B pathway (Fig. 7B). The colocalization of LC3B with p62 (Fig. 7C), mitochondria with lysosomes (Fig. 7D), came down to hyper-mitophagy. Mitophagy, the selective engulfment of dysfunctional mitochondria by autophagasomes, is important for cellular homeostasis and can be induced by mitochondrial oxidative stress. As reported in the literature, DRP-1-dependent mitophagy can be triggered secondary to mitochondrial dysfunction to remove damaged mitochondria. The frequency of division and fusion is balanced to maintain mitochondrial size in healthy cells. Increased demand is met by mitochondrial biogenesis and fusion of individual mitochondria into dynamic networks, whereas a decrease in demand results in the removal of superfluous mitochondria through fission and mitophagy [67, 68]. However, mitochondrial fusion protein (Mfn1/2) and OPA1 expression, in aorta of KD murine model or LPS-induced endothelial injury model were free from influence, under Mas treatment or not (Fig. 8A–C). Since mitochondrial fragmentation is often observed when cells are under stress or when they are dying, DRP-1 has been implicated in the pathogenesis of cell death [46]. DRP-1 is involved in Bax/Bak- or BNIP3-dependent apoptosis by controlling outer mitochondrial membrane permeabilization [49]. Here, DRP-1 contacted with Bak in the fission site to induce cytochrome c release, then cell apoptosis (Fig. 8D–F). In addition, the high expression of E2F3 (Fig. 8J, K) induced p53 activation of endothelial cells (Fig. 8L, M). Surprisingly, the mitophagy seems to work as the driving force of DRP-1/Bak/cytochrome c-dependent endothelial cells apoptosis. DRP-1 overexpressing cell, split mitochondrial network by forced division.
Intact mitochondrial dynamics are critical for the maintenance of normal vascular function, and pharmacological modulation of mitochondrial dynamic proteins may emerge as novel therapeutic targets for a number of cardiovascular diseases resulting from excessive fission. However, targeting mitochondrial fission is a double-edged sword, since physiological mitochondrial fission under stress is necessary for the adaptation to increased energy demands, and repression of mitochondrial fission is not always beneficial. In this scenario, the process of mitochondrial fusion/fission emerges as an important regulator of mitochondrial signaling properties and of the broadly different intracellular effects of physiological and pathological stimuli. Mitochondrial homeostasis should be maintained when targeting mitochondrial dynamics under pathological conditions. Take a comprehensive view of the whole text, how mitophagy is regulated by DRP-1 under pathologic status is critical and complex, which may contribute to the development of specific therapeutic interventions in cardiovascular diseases patients, for example Masatinib, the inhibitor of PDGFRβ.
Data availability
The data are available from the corresponding authors upon reasonable request.
References
Shulman ST, Rowley AH. Advances in Kawasaki disease. Eur J Pediatr. 2004;163:285–91.
Burns JC, Glodé MP. Kawasaki syndrome. Lancet. 2004;364:533–44.
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–99.
Singh S, **dal AK, Pilania RK. Diagnosis of Kawasaki disease. Int J Rheum Dis. 2018;21:36–44.
Pilania RK, **dal AK, Bhattarai D, Naganur SH, Singh S. Cardiovascular involvement in Kawasaki disease is much more than mere coronary arteritis. Front Pediatr. 2020;8:526969.
Mueller F, Knirsch W, Harpes P, Prêtre R, Valsangiacomo Buechel E, Kretschmar O. Long-term follow-up of acute changes in coronary artery diameter caused by Kawasaki disease: risk factors for development of stenotic lesions. Clin Res Cardiol. 2009;98:501–7.
Tsujioka Y, Handa A, Nishimura G, Miura M, Yokoyama K, Sato K, et al. Multisystem imaging manifestations of Kawasaki disease. Radiographics. 2022;42:268–88.
JCS Joint Working Group.Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Digest version. Circ J. 2014;78:2521–62.
Ariga S, Koga M, Takahashi M, Ishihara T, Matsubara T, Furukawa S. Maturation of macrophages from peripheral blood monocytes in Kawasaki disease: immunocytochemical and immunoelectron microscopic study. Pathol Int. 2001;51:257–63.
Katayama K, Matsubara T, Fujiwara M, Koga M, Furukawa S. CD14+CD16+ monocyte subpopulation in Kawasaki disease. Clin Exp Immunol. 2000;121:566–70.
Kobayashi M, Matsumoto Y, Ohya M, Harada K, Kanno H. Histologic and immunohistochemical evaluation of infiltrating inflammatory cells in Kawasaki disease arteritis lesions. Appl Immunohistochem Mol Morphol. 2021;29:62–7.
Yasukawa K, Terai M, Shulman ST, Toyozaki T, Yajima S, Kohno Y, et al. Systemic production of vascular endothelial growth factor and fms-like tyrosine kinase-1 receptor in acute Kawasaki disease. Circulation. 2002;105:766–9.
Chen C-Y, Huang S-H, Chien K-J, Lai T-J, Chang W-H, Hsieh K-S, et al. Reappraisal of VEGF in the pathogenesis of Kawasaki disease. Children. 2022;9:1343.
Kariyazono H, Ohno T, Khajoee V, Ihara K, Kusuhara K, Kinukawa N, et al. Association of vascular endothelial growth factor (VEGF) and VEGF receptor gene polymorphisms with coronary artery lesions of Kawasaki disease. Pediatr Res. 2004;56:953–9.
Van den Akker NM, Winkel LC, Nisancioglu MH, Maas S, Wisse LJ, Armulik A, et al. PDGF-B signaling is important for murine cardiac development: its role in develo** atrioventricular valves, coronaries, and cardiac innervation. Dev Dyn. 2008;237:494–503.
Lindblom P, Gerhardt H, Liebner S, Abramsson A, Enge M, Hellstrom M, et al. Endothelial PDGF-B retention is required for proper investment of pericytes in the microvessel wall. Genes Dev. 2003;17:1835–40.
Raines EW. PDGF and cardiovascular disease. Cytokine Growth Factor Rev. 2004;15:237–54.
Banfi A, von Degenfeld G, Gianni-Barrera R, Reginato S, Merchant MJ, McDonald DM, et al. Therapeutic angiogenesis due to balanced single-vector delivery of VEGF and PDGF-BB. FASEB J. 2012;26:2486–97.
Gaengel K, Genové G, Armulik A, Betsholtz C. Endothelial-mural cell signaling in vascular development and angiogenesis. Arterioscler Thromb Vasc Biol. 2009;29:630–8.
Williams LT. Signal transduction by the platelet-derived growth factor receptor. Science. 1989;243:1564–70.
Betsholtz C, Karlsson L, Lindahl P. Developmental roles of platelet-derived growth factors. BioEssays. 2001;23:494–507.
He S, Hou T, Zhou J, Ai Q, Dou C, Luo F, et al. Endothelial cells promote migration of mesenchymal stem cells via PDGF-BB/PDGFRβ-Src-Akt in the context of inflammatory microenvironment upon bone defect. Stem Cells Int. 2022;2022:2401693.
Ma S, Tang T, Wu X, Mansour AG, Lu T, Zhang J, et al. PDGF-D-PDGFRβ signaling enhances IL-15-mediated human natural killer cell survival. Proc Natl Acad Sci USA. 2022;119:e2114134119.
Zhang Y, Wang Y, Zhang L, **a L, Zheng M, Zeng Z, et al. Reduced platelet miR-223 induction in Kawasaki disease leads to severe coronary artery pathology through a miR-223/PDGFRβ vascular smooth muscle cell axis. Circ Res. 2020;127:855–73.
** J, Wang J, Lu Y, Fan Z, Huang N, Ma L, et al. Platelet-derived microparticles: a new index of monitoring platelet activation and inflammation in Kawasaki disease. Indian J Pediatr. 2019;86:250–5.
Nomura S. Function and clinical significance of platelet-derived microparticles. Int J Hematol. 2001;74:397–404.
Yahata T, Suzuki C, Yoshioka A, Hamaoka A, Ikeda K. Platelet activation dynamics evaluated using platelet-derived microparticles in Kawasaki disease. Circ J. 2014;78:188–93.
Wyler von Ballmoos M, Yang Z, Völzmann J, Baumgartner I, Kalka C, Di Santo S. Endothelial progenitor cells induce a phenotype shift in differentiated endothelial cells towards PDGF/PDGFRβ axis-mediated angiogenesis. PLoS ONE. 2010;5:e14107.
Chitnis T, Weiner HL. CNS inflammation and neurodegeneration. J Clin Invest. 2017;127:3577–87.
Ochi M. Review: surgical treatment of giant coronary aneurysms in pediatric patients with Kawasaki disease. Gen Thorac Cardiovasc Surg. 2018;66:121–9.
Takahashi K, Oharaseki T, Naoe S, Wakayama M, Yokouchi Y. Neutrophilic involvement in the damage to coronary arteries in acute stage of Kawasaki disease. Pediatr Int. 2005;47:305–10.
Jia C, Zhang J, Chen H, Zhuge Y, Chen H, Qian F, et al. Endothelial cell pyroptosis plays an important role in Kawasaki disease via HMGB1/RAGE/cathespin B signaling pathway and NLRP3 inflammasome activation. Cell Death Dis. 2019;10:778.
Liu M, Gomez D. Smooth muscle cell phenotypic diversity. Arterioscler Thromb Vasc Biol. 2019;39:1715–23.
Alderton WK, Cooper CE, Knowles RG. Nitric oxide synthases: structure, function and inhibition. Biochem J. 2001;357:593–615.
Park-Windhol C, D’Amore PA. Disorders of vascular permeability. Annu Rev Pathol. 2016;11:251–81.
Ohno T, Igarashi H, Inoue K, Akazawa K, Joho K, Hara T. Serum vascular endothelial growth factor: a new predictive indicator for the occurrence of coronary artery lesions in Kawasaki disease. Eur J Pediatr. 2000;159:424–9.
Takeshita S, Kawamura Y, Takabayashi H, Yoshida N, Nonoyama S. Imbalance in the production between vascular endothelial growth factor and endostatin in Kawasaki disease. Clin Exp Immunol. 2005;139:575–9.
Hamamichi Y, Ichida F, Yu X, Hirono KI, Uese KI, Hashimoto I, et al. Neutrophils and mononuclear cells express vascular endothelial growth factor in acute Kawasaki disease: its possible role in progression of coronary artery lesions. Pediatr Res. 2001;49:74–80.
Kimura H, Esumi H. Reciprocal regulation between nitric oxide and vascular endothelial growth factor in angiogenesis. Acta Biochim Pol. 2003;50:49–59.
Peoples JN, Saraf A, Ghazal N, Pham TT, Kwong JQ. Mitochondrial dysfunction and oxidative stress in heart disease. Exp Mol Med. 2019;51:1–13.
Lambeth JD. Nox/Duox family of nicotinamide adenine dinucleotide (phosphate) oxidases. Curr Opin Hematol. 2002;9:11–17.
Kuroda J, Ago T, Matsushima S, Zhai P, Schneider MD, Sadoshima J. NADPH oxidase 4 (Nox4) is a major source of oxidative stress in the failing heart. Proc Natl Acad Sci USA. 2010;107:15565–70.
** JY, Wei XX, Zhi XL, Wang XH, Meng D. Drp1-dependent mitochondrial fission in cardiovascular disease. Acta Pharmacol Sin. 2021;42:655–64.
Cho B, Choi SY, Cho HM, Kim HJ, Sun W. Physiological and pathological significance of dynamin-related protein 1 (drp1)-dependent mitochondrial fission in the nervous system. Exp Neurobiol. 2013;22:149–57.
Simula L, Campanella M, Campello S. Targeting Drp1 and mitochondrial fission for therapeutic immune modulation. Pharmacol Res. 2019;146:104317.
Frank S, Gaume B, Bergmann-Leitner ES, Leitner WW, Robert EG, Catez F, et al. The role of dynamin-related protein 1, a mediator of mitochondrial fission, in apoptosis. Dev Cell. 2001;1:515–25.
Tanaka A, Cleland MM, Xu S, Narendra DP, Suen DF, Karbowski M, et al. Proteasome and p97 mediate mitophagy and degradation of mitofusins induced by Parkin. J Cell Biol. 2010;191:1367–80.
Lee Y, Lee HY, Hanna RA, Gustafsson ÅB. Mitochondrial autophagy by Bnip3 involves Drp1-mediated mitochondrial fission and recruitment of Parkin in cardiac myocytes. Am J Physiol Heart Circ Physiol. 2011;301:H1924–31.
Tong M, Zablocki D, Sadoshima J. The role of Drp1 in mitophagy and cell death in the heart. J Mol Cell Cardiol. 2020;142:138–45.
Knott AB, Perkins G, Schwarzenbacher R, Bossy-Wetzel E. Mitochondrial fragmentation in neurodegeneration. Nat Rev Neurosci. 2008;9:505–18.
Szabadkai G, Simoni AM, Chami M, Wieckowski MR, Youle RJ, Rizzuto R. Drp-1-dependent division of the mitochondrial network blocks intraorganellar Ca2+ waves and protects against Ca2+-mediated apoptosis. Mol Cell. 2004;16:59–68.
Lee YJ, Jeong SY, Karbowski M, Smith CL, Youle RJ. Roles of the mammalian mitochondrial fission and fusion mediators Fis1, Drp1, and Opa1 in apoptosis. Mol Biol Cell. 2004;15:5001–11.
Ziebold U, Reza T, Caron A, Lees JA. E2F3 contributes both to the inappropriate proliferation and to the apoptosis arising in Rb mutant embryos. Genes Dev. 2001;15:386–91.
Lazzerini Denchi E, Helin K. E2F1 is crucial for E2F-dependent apoptosis. EMBO Rep. 2005;6:661–8.
Martinez LA, Goluszko E, Chen HZ, Leone G, Post S, Lozano G, et al. E2F3 is a mediator of DNA damage-induced apoptosis. Mol Cell Biol. 2010;30:524–36.
Denby KJ, Clark DE, Markham LW. Management of Kawasaki disease in adults. Heart. 2017;103:1760–9.
Motoji Y, Fukazawa R, Matsui R, Abe Y, Uehara I, Watanabe M, et al. Statins show anti-atherosclerotic effects by improving endothelial cell function in a Kawasaki disease-like vasculitis mouse model. Int J Mol Sci. 2022;23:16108.
Greenberg JI, Shields DJ, Barillas SG, Acevedo LM, Murphy E, Huang J, et al. A role for VEGF as a negative regulator of pericyte function and vessel maturation. Nature. 2008;456:809–13.
Marushima A, Nieminen M, Kremenetskaia I, Gianni-Barrera R, Woitzik J, von Degenfeld G, et al. Balanced single-vector co-delivery of VEGF/PDGF-BB improves functional collateralization in chronic cerebral ischemia. J Cereb Blood Flow Metab. 2020;40:404–19.
Liu T, Ma W, Xu H, Huang M, Zhang D, He Z, et al. PDGF-mediated mesenchymal transformation renders endothelial resistance to anti-VEGF treatment in glioblastoma. Nat Commun. 2018;9:3439.
Pellet-Many C. VEGF-A(165)-induced endothelial cells chemotactic migration and invasion assays. Methods Mol Biol. 2022;2475:205–14.
Lassègue B, Sorescu D, Szöcs K, Yin Q, Akers M, Zhang Y, et al. Novel gp91(phox) homologues in vascular smooth muscle cells : nox1 mediates angiotensin II-induced superoxide formation and redox-sensitive signaling pathways. Circ Res. 2001;88:888–94.
Chan DC. Mitochondrial fusion and fission in mammals. Annu Rev Cell Dev Biol. 2006;22:79–99.
Pickles S, Vigié P, Youle RJ. Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr Biol. 2018;28:R170–r185.
Liu R, Xu C, Zhang W, Cao Y, Ye J, Li B, et al. FUNDC1-mediated mitophagy and HIF1α activation drives pulmonary hypertension during hypoxia. Cell Death Dis. 2022;13:634.
Fu ZJ, Wang ZY, Xu L, Chen XH, Li XX, Liao WT, et al. HIF-1α-BNIP3-mediated mitophagy in tubular cells protects against renal ischemia/reperfusion injury. Redox Biol. 2020;36:101671.
Hoitzing H, Johnston IG, Jones NS. What is the function of mitochondrial networks? A theoretical assessment of hypotheses and proposal for future research. BioEssays. 2015;37:687–700.
Chan DC. Fusion and fission: interlinked processes critical for mitochondrial health. Annu Rev Genet. 2012;46:265–87.
Acknowledgements
Financial support by the National Natural Science Foundation of China (No. 81973410, No. 82003808), the independent research fund of Yunnan Characteristic Plant Extraction Laboratory (2022YKZY006).
Author information
Authors and Affiliations
Contributions
The study was conceived and planned by JZ, HYL and XM. The manuscript was written and revised by XHA, HL and JZ. XHA, HL and JS participated in the experiment design, collection and analysis of data. The partial experiments were performed by TGW, RZZ, XZ and XM. All other authors approved the manuscript prior to submission. All authors have seen the manuscript and approved to submit to your journal.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures and assessments were approved by the Animal Ethics Committee of the School of Chinese Materia Medica, China Pharmaceutical University.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Professor Gian Maria Fimia
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
An, X., Ma, X., Liu, H. et al. Inhibition of PDGFRβ alleviates endothelial cell apoptotic injury caused by DRP-1 overexpression and mitochondria fusion failure after mitophagy. Cell Death Dis 14, 756 (2023). https://doi.org/10.1038/s41419-023-06272-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41419-023-06272-3
- Springer Nature Limited