Abstract
Background
This open-label, Phase 1b/2 study evaluated the highly selective MET inhibitor tepotinib in systemic anticancer treatment (SACT)-naive Asian patients with advanced hepatocellular carcinoma (aHCC) with MET overexpression.
Methods
In Phase 2b, tepotinib was orally administered once daily (300, 500 or 1,000 mg) to Asian adults with aHCC. The primary endpoints were dose-limiting toxicities (DLTs) and adverse events (AEs). Phase 2 randomised SACT-naive Asian adults with aHCC with MET overexpression to tepotinib (recommended Phase 2 dose [RP2D]) or sorafenib 400 mg twice daily. The primary endpoint was independently assessed time to progression (TTP).
Results
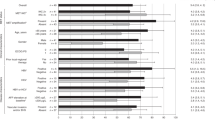
In Phase 1b (n = 27), no DLTs occurred; the RP2D was 500 mg. In Phase 2 (n = 90, 45 patients per arm), the primary endpoint was met: independently assessed TTP was significantly longer with tepotinib versus sorafenib (median 2.9 versus 1.4 months, HR = 0.42, 90% confidence interval: 0.26–0.70, P = 0.0043). Progression-free survival and objective response also favoured tepotinib. Treatment-related Grade ≥3 AE rates were 28.9% with tepotinib and 45.5% with sorafenib.
Conclusions
Tepotinib improved TTP versus sorafenib and was generally well tolerated in SACT-naive Asian patients with aHCC with MET overexpression.
Trial registration
ClinicalTrials.gov NCT01988493.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults.1 Its incidence is rising alongside increasing rates of chronic liver disease. For many years, the only approved targeted systemic therapy for advanced HCC was the non-selective multikinase inhibitor sorafenib.2,3 This agent provides only a modest improvement in overall survival (OS) and may not be as well tolerated by Asian patients compared with those of other ethnicities.4,5 Newer first-line treatment options include the multikinase inhibitor lenvatinib and the immunotherapy atezolizumab (in combination bevacizumab), which have been approved following positive data from randomised Phase 3 trials versus sorafenib.3,6,7,8
MET is the tyrosine kinase receptor for hepatocyte growth factor (HGF).9 Approximately 50% of patients with HCC may harbour MET alterations,9 and 28% of patients with advanced HCC show evidence of MET overexpression.10 These patients may derive therapeutic benefit from selective MET inhibition.9,11 In vitro, MET inhibitors can reduce the growth of MET-positive HCC cell line-derived xenograft models.11
Tepotinib is an orally available, potent and highly selective MET inhibitor that has shown pronounced antitumour activity in MET-dependent preclinical mouse models in vivo.12,14,15 Furthermore, in combination with gefitinib, tepotinib has demonstrated improved efficacy compared with chemotherapy in patients with advanced epidermal growth factor receptor-mutant non-small cell lung cancer and MET-driven resistance to epidermal growth factor receptor (EGFR) inhibitors16 and a Phase 2 study of tepotinib plus osimertinib in patients with acquired resistance to first-line osimertinib due to MET amplification is ongoing (INSIGHT 2, NCT03940703). A Phase 2 study is also underway investigating tepotinib in combination with cetuximab in patients with RAS/BRAF wild-type left-sided metastatic colorectal cancer and acquired resistance to anti-EGFR antibody-targeted therapy due to MET amplification (NCT04515394).
Following preclinical data demonstrating activity of tepotinib against primary liver cancer explants with MET overexpression,12 two Phase 1b/2 studies were designed to investigate tepotinib in patients with HCC with MET overexpression. In the first of these (NCT02115373), tepotinib demonstrated clinical activity and was generally well tolerated in US/European patients in whom prior sorafenib treatment had failed.17 Here, we present the second trial in HCC, which was conducted in Asian patients (NCT01988493). Since patients with hepatic impairment were excluded from the first-in-human trial,15,17,19 and no unexpected AEs were reported. Patients treated with tepotinib reported fewer overall and Grade ≥3 treatment-related AEs compared with sorafenib.
With the 500 mg dose in the Phase 1b study, tepotinib AUCτ was 61% and Cmax was 63% of that observed in the first-in-human trial.13 This is expected given findings from a population pharmacokinetic analysis showing a reduction in tepotinib exposure in patients with cirrhosis, as well as from a dedicated pharmacokinetic hepatic impairment trial.32 In the latter study, patients with moderate hepatic impairment (Child–Pugh B) had 12% lower AUC from time 0 to infinity and 29% lower Cmax compared with control subjects without hepatic impairment. Lower exposure relative to the first-in-human trial was also observed in the Phase 1b/2 study in sorafenib pre-treated advanced HCC with MET overexpression.33
The selection of sorafenib, as the control treatment, for the present study reflects the standard of care for first-line treatment at the time of study conception. Since then, both the multikinase inhibitor lenvatinib and the combination of atezolizumab (anti-programmed death-ligand 1 [PD-L1]) plus bevacizumab (anti-vascular endothelial growth factor [VEGF]) have been approved in the first-line setting.6,7 After sorafenib failure, approved options include the anti-VEGF receptor-2 agent ramucirumab (for patients with elevated serum alpha-fetoprotein), the multikinase inhibitors regorafenib and cabozantinib and the immune checkpoint inhibitors pembrolizumab and nivolumab (± ipilimumab).21,30,34,35,36,37,38 While durable responses to nivolumab were observed in both sorafenib-naive and sorafenib pre-treated patients in the Phase 1/2 CheckMate 040 study,37,39 first-line nivolumab did not show an OS benefit compared with sorafenib in the Phase 3 CheckMate 459 trial.40 Other immunotherapy-containing strategies currently undergoing Phase 3 evaluation in previously untreated disease include durvalumab (anti-PD-L1), alone or in combination with a second immunotherapy (tremelimumab, anti-cytotoxic T-lymphocyte-associated protein-4; NCT03298451), lenvatinib plus pembrolizumab (LEAP-002; NCT03713593) and cabozantinib plus atezolizumab (COSMIC-312;41 NCT03755791). Given the favourable safety profile of tepotinib and the immunosuppressive function of MET signalling,42 use of tepotinib in combination with immunotherapies could be an interesting area for future study.
Strengths of the current study include the randomised design, which permitted evaluation of tepotinib efficacy relative to an established standard of care in this setting. Limitations include the non-blinded treatment assignment and the low proportions of patients with MET amplification or MET IHC 3+ status, which limited explorations of the impact of MET-based biomarkers on efficacy. The study was also underpowered following early termination of enrolment due to slow accrual, but nonetheless demonstrated significant improvements in activity endpoints with tepotinib versus sorafenib. As has been discussed for other studies in HCC with biomarker-driven patient selection,23,24 one challenge in this setting is the potential for patients with the most aggressive forms of disease to be excluded, due to rapid progression and/or clinical deterioration, while central biomarker assessments are ongoing, which could have contributed to ineligibility at screening. Finally, it is not known to what extent these results obtained in Asian patients, who were predominantly male with BCLC stage B, can be generalised to other populations.
In the Phase 1b part of this study, no DLTs were reported and the RP2D was established as 500 mg QD. Evidence of antitumour activity was seen at the 500 mg and 1,000 mg dose levels. In Phase 2, first-line tepotinib (500 mg QD) demonstrated clinical activity in Asian patients with advanced HCC with MET overexpression (IHC 2+/3+), with a significant improvement versus sorafenib in the primary endpoint of TTP, as well as PFS and ORR. Tepotinib was generally well tolerated and no new safety signals were observed.
References
Sayiner, M., Golabi, P. & Younossi, Z. M. Disease burden of hepatocellular carcinoma: a global perspective. Dig. Dis. Sci. 64, 910–917 (2019).
Raoul, J. L., Kudo, M., Finn, R. S., Edeline, J., Reig, M. & Galle, P. R. Systemic therapy for intermediate and advanced hepatocellular carcinoma: Sorafenib and beyond. Cancer Treat. Rev. 68, 16–24 (2018).
Bruix, J., da Fonseca, L. G. & Reig, M. Insights into the success and failure of systemic therapy for hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 16, 617–630 (2019).
Cheng, A. L., Kang, Y. K., Chen, Z., Tsao, C. J., Qin, S., Kim, J. S. et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 10, 25–34 (2009).
Llovet, J. M., Ricci, S., Mazzaferro, V., Hilgard, P., Gane, E., Blanc, J. F. et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 359, 378–390 (2008).
Kudo, M., Finn, R. S., Qin, S., Han, K.-H., Ikeda, K., Piscaglia, F. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391, 1163–1173 (2018).
Finn, R. S., Qin, S., Ikeda, M., Galle, P. R., Ducreux, M., Kim, T. Y. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905 (2020).
Tecentriq (atezolizumab) US Prescribing Information (2020).
Bouattour, M., Raymond, E., Qin, S., Cheng, A.-L., Stammberger, U., Locatelli, G. et al. Recent developments of c-Met as a therapeutic target in hepatocellular carcinoma. Hepatology 67, 1132–1149 (2018).
Lee, S. J., Lee, J., Sohn, I., Mao, M., Kai, W., Park, C.-K. et al. A survey of c-MET expression and amplification in 287 patients with hepatocellular carcinoma. Anticancer Res. 33, 5179–5186 (2013).
You, H., Ding, W., Dang, H., Jiang, Y. & Rountree, C. B. c-Met represents a potential therapeutic target for personalized treatment in hepatocellular carcinoma. Hepatology 54, 879–889 (2011).
Bladt, F., Friese-Hamim, M., Ihling, C., Wilm, C. & Blaukat, A. The c-Met inhibitor MSC2156119J effectively inhibits tumor growth in liver cancer models. Cancers (Basel). 6, 1736–1752 (2014).
Falchook, G. S., Kurzrock, R., Amin, H. M., **ong, W., Fu, S., Piha-Paul, S. A. et al. First-in-man phase I trial of the selective MET inhibitor tepotinib in patients with advanced solid tumors. Clin. Cancer Res. 26, 1237–1246 (2020).
Park, K., Felip, E., Veillon, R., Cortot, A., Mazieres, J., Sakai, H. et al. Tepotinib in NSCLC patients harboring METex14 skip**: Cohort A of phase II VISION study. Ann. Oncol. 30, ix22–ix29 (2019).
Paik, P. K., Felip, E., Veillon, R., Sakai, H., Cortot, A. B., Garassino, M. C. et al. Tepotinib in non-small-cell lung cancer with MET exon 14 skip** mutations. N. Engl. J. Med. 383, 931–943 (2020).
Wu, Y. L., Cheng, Y., Zhou, J., Lu, S., Zhang, Y., Zhao, J. et al. Tepotinib plus gefitinib in patients with EGFR-mutant non-small-cell lung cancer with MET overexpression or MET amplification and acquired resistance to previous EGFR inhibitor (INSIGHT study): an open-label, phase 1b/2, multicentre, randomised trial. Lancet Res. Med. 8, 1132–1143 (2020).
Decaens, T., Barone, C., Assenat, E., Wermke, M., Fasolo, A., Merle, P. et al. Efficacy and safety of the Met inhibitor tepotinib in patients (pts) with advanced Met+ hepatocellular carcinoma (HCC) previously treated with sorafenib. Ann. Oncol. 29, ix48 (2018).
Cappuzzo, F., Marchetti, A., Skokan, M., Rossi, E., Gajapathy, S., Felicioni, L. et al. Increased MET gene copy number negatively affects survival of surgically resected non-small-cell lung cancer patients. J. Clin. Oncol. 27, 1667–1674 (2009).
Shitara, K., Yamazaki, K., Tsushima, T., Naito, T., Matsubara, N. & Watanabe, M. Phase I trial of the MET inhibitor tepotinib in Japanese patients with solid tumors. Jpn. J. Clin. Oncol. 50, 859–866 (2020).
Faivre, S. J., Blanc, J.-F., Merle, P., Fasolo, A., Iacobellis, A., Decaens, T. et al. Final phase Ib data for the oral c-Met inhibitor tepotinib in patients with previously treated advanced hepatocellular carcinoma. J. Clin. Oncol. 35, e15676 (2017).
Abou-Alfa, G. K., Meyer, T., Cheng, A.-L., El-Khoueiry, A. B., Rimassa, L., Ryoo, B.-Y. et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 379, 54–63 (2018).
Santoro, A., Rimassa, L., Borbath, I., Daniele, B., Salvagni, S., Van Laethem, J. L. et al. Tivantinib for second-line treatment of advanced hepatocellular carcinoma: a randomised, placebo-controlled phase 2 study. Lancet Oncol. 14, 55–63 (2013).
Rimassa, L., Assenat, E., Peck-Radosavljevic, M., Pracht, M., Zagonel, V., Mathurin, P. et al. Tivantinib for second-line treatment of MET-high, advanced hepatocellular carcinoma (METIV-HCC): a final analysis of a phase 3, randomised, placebo-controlled study. Lancet Oncol. 19, 682–693 (2018).
Kudo, M., Morimoto, M., Moriguchi, M., Izumi, N., Takayama, T., Yoshiji, H. et al. A randomized, double-blind, placebo-controlled, phase 3 study of tivantinib in Japanese patients with MET-high hepatocellular carcinoma. Cancer Sci. 111, 3759–3769 (2020).
Qin, S., Chan, S. L., Sukeepaisarnjaroen, W., Han, G., Choo, S. P., Sriuranpong, V. et al. A phase II study of the efficacy and safety of the MET inhibitor capmatinib (INC280) in patients with advanced hepatocellular carcinoma. Ther. Adv. Med. Oncol. 11, 1758835919889001 (2019).
Basilico, C., Pennacchietti, S., Vigna, E., Chiriaco, C., Arena, S., Bardelli, A. et al. Tivantinib (ARQ197) displays cytotoxic activity that is independent of its ability to bind MET. Clin. Cancer Res. 19, 2381–2392 (2013).
Remsing Rix, L. L., Kuenzi, B. M., Luo, Y., Remily-Wood, E., Kinose, F., Wright, G. et al. GSK3 alpha and beta are new functionally relevant targets of tivantinib in lung cancer cells. ACS Chem. Bio. 9, 353–358 (2014).
Wu, Y. L., Soo, R. A., Locatelli, G., Stammberger, U., Scagliotti, G. & Park, K. Does c-Met remain a rational target for therapy in patients with EGFR TKI-resistant non-small cell lung cancer? Cancer Treat. Rev. 61, 70–81 (2017).
Zhu, A. X., Park, J. O., Ryoo, B. Y., Yen, C. J., Poon, R., Pastorelli, D. et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 16, 859–870 (2015).
Zhu, A. X., Kang, Y. K., Yen, C. J., Finn, R. S., Galle, P. R., Llovet, J. M. et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased alpha-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 20, 282–296 (2019).
Llovet, J. M., Pena, C. E., Lathia, C. D., Shan, M., Meinhardt, G., Bruix, J. et al. Plasma biomarkers as predictors of outcome in patients with advanced hepatocellular carcinoma. Clin. Cancer Res. 18, 2290–2300 (2012).
Tepotinib Japanese Package Insert (2020).
Decaens, T., Barone, C., Assenat, E., Wermke, M., Fasolo, A., Merle, P. et al. Phase 1b/2 trial of tepotinib in sorafenib pretreated advanced hepatocellular carcinoma with MET overexpression. Br. J. Cancer https://doi.org/10.1038/s41416-021-01334-9 (2021).
Bruix, J., Qin, S., Merle, P., Granito, A., Huang, Y. H., Bodoky, G. et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389, 56–66 (2017).
Zhu, A. X., Finn, R. S., Edeline, J., Cattan, S., Ogasawara, S., Palmer, D. et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 19, 940–952 (2018).
Finn, R. S., Ryoo, B. Y., Merle, P., Kudo, M., Bouattour, M., Lim, H. Y. et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, Phase III trial. J. Clin. Oncol. 38, 193–202 (2020).
El-Khoueiry, A. B., Sangro, B., Yau, T., Crocenzi, T. S., Kudo, M., Hsu, C. et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389, 2492–2502 (2017).
Yau, T., Kang, Y.-K., Kim, T.-Y., El-Khoueiry, A. B., Santoro, A., Sangro, B. et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the CheckMate 040 randomized clinical trial. JAMA Oncol. 6, e204564 (2020).
Crocenzi, T. S., El-Khoueiry, A. B., Yau, T. C., Melero, I., Sangro, B., Kudo, M. et al. Nivolumab (nivo) in sorafenib (sor)-naive and -experienced pts with advanced hepatocellular carcinoma (HCC): CheckMate 040 study. J. Clin. Oncol. 35, 4013 (2017).
Yau, T., Park, J. W., Finn, R. S., Cheng, A. L., Mathurin, P., Edeline, J. et al. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 30, v874–v875 (2019).
Kelley, R. K., J, W. O., Hazra, S., Benzaghou, F., Yau, T., Cheng, A. L. et al. Cabozantinib in combination with atezolizumab versus sorafenib in treatment-naive advanced hepatocellular carcinoma: COSMIC-312 Phase III study design. Future Oncol. 16, 1525–1536 (2020).
Papaccio, F., Della Corte, C. M., Viscardi, G., Di Liello, R., Esposito, G., Sparano, F. et al. HGF/MET and the immune system: relevance for cancer immunotherapy. Int. J. Mol. Sci. 19, 3295 (2018).
Acknowledgements
The authors would like to thank patients, investigators, co-investigators and the study teams at all participating centres and at Merck KGaA, Darmstadt, Germany, and Merck Serono Pharmaceutical R&D Co., Ltd., Bei**g, China (an affiliate of Merck KGaA, Darmstadt, Germany). Part of this paper has been previously presented at congresses: Qin, S., Kim, T.-Y., Lim, H.Y., Ryoo, B.-Y., Scheele, J., Zhou, D. et al. Phase Ib trial of tepotinib in Asian patients with advanced hepatocellular carcinoma (HCC): final data including long-term outcomes. J. Clin. Oncol. 35(Suppl 15): abstract 4087 (2017). Qin, S., Kim, T.-Y., Lim, H.Y., Ryoo, B.-Y., Zhou, D., Zhao, C., Becker, A. et al. Final data from a phase Ib trial of tepotinib in Asian patients with advanced hepatocellular carcinoma (HCC). Ann. Oncol. 28(Suppl 5): abstract 701 P (2017). Ryoo, B.Y., Ren, Z., Kim, T.-Y., Pan, H., Rau, K.-M., Choi, H.J. et al. Phase 2 trial of tepotinib vs sorafenib for treatment-naïve advanced hepatocellular carcinoma (HCC) in Asian patients. Ann. Oncol. 29(Suppl 9): abstract 186 P (2018). Qin, S., Ryoo, B.-Y., Decaens, T., Bruns, R., Zhou, D., Scheele, J. et al. Safety of tepotinib in patients with MET overexpressing (MET+) advanced hepatocellular carcinoma (HCC): outcomes from two studies. Liver Cancer 8(Suppl 1): abstract O-042 (2019).
Author information
Authors and Affiliations
Contributions
All authors participated fully in develo** and reviewing the paper for publication with final approval for submission. B-Y.R. and S.Q. were involved in conceptualisation, data curation, formal analysis, investigation, supervision and validation. A.C. was involved in data curation, investigation, supervision and validation. J.H.K. and H.P. were involved in investigation and resources. K-M.R. was involved in investigation and project administration. C.J.Y. was involved in investigation, data curation and visualisation of the paper. K.B., D.Z. and J.S. were involved in formal analysis, investigation and validation. H.Y.L. was involved in conceptualisation, data curation, investigation, validation and visualisation. Z.R., T-Y.K., H.J.C. and J-W.P. were involved in investigation. J.Sc. was involved in conceptualisation, data curation, formal analysis, investigation and supervision (Medical Lead).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients provided written informed consent for participation in the study. The study was conducted in accordance with the Declaration of Helsinki. This study has been reviewed and approved by the respective Institutional Review Boards/Independent Ethics Committees according to national and international regulations (Supplementary Table 5).
Consent to publish
Not applicable.
Data availability
Data are held by the sponsor Merck KGaA (Darmstadt, Germany), to whom any request for additional data should be addressed.
Competing interests
Ann-Lii Cheng has provided consulting for AstraZeneca, Bristol-Myers Squibb, Eisai, Merck KGaA, Novartis, Ono Pharmaceutical, Exelixis, IPSEN Innovation, Bayer Healthcare, Merck Sharp Dohme, Roche/Genentech, BeiGene, CSR Pharma Group, F. Hoffmann-La Roche and IQVIA; attended speakers’ bureau for Bayer Yakuhin Ltd., Novartis, Eisai, Ono Pharmaceutical and Amgen Taiwan; received travel grants from Bayer Yakuhin Ltd, Roche/Genentech and IQVIA. Joong-Won Park participated in consultant and advisory boards for AstraZeneca, Ipsen, Bristol-Myers Squibb, Roche and Bayer, and attended speaker’s bureau for Bayer, Ipsen and Eisai. Ho Yeong Lim attended advisory boards for Bayer, Eisai, Ono Pharmaceuticals, Bristol-Myers Squibb, Merck KGaA, Ipsen, AstraZeneca, and attended speaker’s bureau for Bayer. Baek-Yeol Ryoo, Zhenggang Ren, Tae-You Kim, Hongming Pan, Kun-Ming Rau, Hye ** Choi, Jee Hyun Kim, Chia Jui Yen and Shukui Qin have nothing to declare. Juergen Scheele was an employee of Merck KGaA, Darmstadt, Germany, at the time the work was conducted. Karin Berghoff, Josef Straub and Dongli Zhou are employees of Merck KGaA, Darmstadt, Germany and also hold stocks with the company.
Funding information
The sponsor, Merck KGaA, Darmstadt, Germany, provided the study drug and worked with investigators on the trial design and plan, collection and analyses of data, and interpretation of results. Data sets were reviewed by the authors, and all authors participated fully in develo** and reviewing the paper for publication. Funding for a professional medical writer with access to the data was provided by the sponsor for initial drafts of the paper. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. Medical writing assistance was provided by Helen Swainston (Bioscript Science, Macclesfield, UK), Jack Eaton (Syneos Health, UK) and Mark Dyson, DPhil (Berlin, Germany), and was funded by Merck KGaA, Darmstadt, Germany.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ryoo, BY., Cheng, AL., Ren, Z. et al. Randomised Phase 1b/2 trial of tepotinib vs sorafenib in Asian patients with advanced hepatocellular carcinoma with MET overexpression. Br J Cancer 125, 200–208 (2021). https://doi.org/10.1038/s41416-021-01380-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01380-3
- Springer Nature Limited
This article is cited by
-
New clinical trial design in precision medicine: discovery, development and direction
Signal Transduction and Targeted Therapy (2024)
-
Evolving therapeutic landscape of advanced hepatocellular carcinoma
Nature Reviews Gastroenterology & Hepatology (2023)
-
Exposure–response analyses for the MET inhibitor tepotinib including patients in the pivotal VISION trial: support for dosage recommendations
Cancer Chemotherapy and Pharmacology (2022)
-
Phase 1b/2 trial of tepotinib in sorafenib pretreated advanced hepatocellular carcinoma with MET overexpression
British Journal of Cancer (2021)