Abstract
Background and Objective:
In patients with coronary artery disease (CAD), obesity is paradoxically associated with better survival (the ‘obesity paradox’). Our objective was to determine whether this counterintuitive relationship extends to health-related quality of life (HRQOL) outcomes.
Design:
Cross-sectional observational study.
Subjects:
All adults undergoing coronary angiography residing in Alberta, Canada between January 2003 and March 2006 in the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) registry.
Methods:
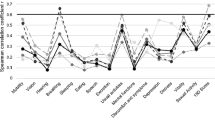
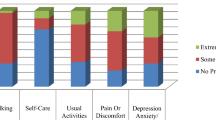
Patients completed self-reported questionnaires 1 year after their index cardiac catheterization, including the Seattle Angina Questionnaire (SAQ) and the EuroQol 5D (EQ-5D Index). Patients were grouped into six body mass index (BMI) categories (underweight, normal, overweight, mild obesity, moderate obesity and severe obesity). An analysis of covariance was used to create risk-adjusted scores.
Results:
A total of 5362 patients were included in the analysis. Obese patients were younger than normal and overweight participants, and had a higher prevalence of depression and cardiovascular risk factors. In the adjusted models, SAQ physical function scores and the EQ Index (representing overall QOL) were significantly reduced in patients with mild, moderate and severe obesity compared with patients with a normal BMI. Patients with severe obesity had both statistically and clinically significant reductions in HRQOL scores. Depressive symptoms accounted for a large proportion in variability of all HRQOL scores.
Conclusions:
BMI is inversely associated with physical function and overall HRQOL in CAD patients, especially in patients with severe obesity. High body weight is a modifiable risk factor; however, given the apparent obesity paradox in patients with CAD, it is critical that future studies be conducted to fully clarify the relationships between HRQOL and body composition (body fat and lean mass), nutritional state and survival outcomes.
Similar content being viewed by others
References
Oreopoulos A, Padwal R, Norris C, Mullen M, Kalantar-Zadeh K . Effect of obesity on short- and long-term mortality post coronary revascularization: a meta-analysis. Obesity 2008; 16: 442–450.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 2006; 368: 666–678.
Kalantar-Zadeh K, Kilpatrick RD, Kuwae N, Wu DY . Reverse epidemiology: a spurious hypothesis or a hardcore reality? Blood Purif 2005; 23: 57–63.
Oreopoulos A, McAlister F, Kalantar-Zadeh K, Padwal R, Ezekowitz J, Sharma A et al. Relationship between BMI, treatment, and mortality in coronary artery disease. Euro Heart J 2009; 30: 2584–2592.
Lavie CJ, Milani RV . Effects of cardiac rehabilitation, exercise training, and weight reduction on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in obese coronary patients. Am J Cardiol 1997; 79: 397–401.
Lavie CJ, Milani RV, Artham SM, Patel DA, Ventura HO . The obesity paradox, weight loss, and coronary disease. Am J Med 2009; 112: 1106–1114.
Lavie CJ, Morshedi-Meibodi A, Milani RV . Impact of cardiac rehabilitation on coronary risk factors, inflammation, and the metabolic syndrome in obese coronary patients. J Cardiometab Syndr 2008; 3: 136–140.
Lavie CJ, Thomas RJ, Squires RW, Allison TG, Milani RV . Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc 2009; 84: 373–383.
Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ . Obesity and psychiatric disorder: developmental trajectories. Pediatrics 2003; 111: 851–859.
Larsson U, Karlsson J, Sullivan M . Impact of overweight and obesity on health-related quality of life—a Swedish population study. Int J Obes Relat Metab Disord 2002; 26: 417–424.
Hassan MK, Joshi AV, Madhavan SS, Amonkar MM . Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes Relat Metab Disord 2003; 27: 1227–1232.
Hopman W, Perger C, Joseph L, Barr S, Bao Y, Prior J et al. The association between body mass index and health-related quality of life: data from CaMos, a stratified population study. Qual Life Res 2007; 16: 1595–1603.
Ghali WA, Knudtson ML . Overview of the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease. On behalf of the APPROACH investigators. Can J Cardiol 2000; 16: 1225–1230.
Smith LR, Harrel Jr FE, Rankin JS, Califf JM, Pryor DB, Muhlbaier LH et al. Determinants of early versus late cardiac death in patients undergoing coronary artery bypass graft surgery. Circulation 1991; 84 (Suppl III): III-245–III-253.
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol 1995; 25: 333–341.
McDowell I, Newell C . Measuring Health: A Guide to Rating Scales and Questionnaires, 2nd edn. Oxford University Press: New York, NY, 1996.
Shaw JW, Johnson JA, Coons SJ . US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care 2005; 43: 203–220.
Johnson JA, Pickard AS . Comparison of the EQ-5D and SF-12 health surveys in a general population survey in Alberta, Canada. Med Care 2000; 38: 115–121.
Denollet J, Brutsaert DL . Personality, disease severity, and the risk of long-term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation 1998; 97: 167–173.
Irwin M, Artin KH, Oxman MN . Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med 1999; 159: 1701–1704.
Norris CM, Saunders LD, Ghali WA, Brant R, Galbraith PD, Graham M et al. Health-related quality of life outcomes of patients with coronary artery disease treated with cardiac surgery, percutaneous coronary intervention or medical management. Can J Cardiol 2004; 20: 1259–1266.
Radloff L . The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 395–401.
Andresen EM, Malmgren JA, Carter WB, Patrick DL . Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994; 10: 77–84.
World Health Organization. Physical status: the use and interpretation of anthropometry: report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D . Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics 1999; 15: 141–155.
Spertus JA, McDonell M, Woodman CL, Fihn SD . Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am Heart J 2000; 140: 105–110.
Sullivan P, Lawrence WF, Ghushchyan V . A national catalogue of preference-based scores for chronic conditions in the U.S. Med Care 2005; 43: 736–749.
Kalantar-Zadeh K, Kuwae N, Wu DY, Shantouf RS, Fouque D, Anker SD et al. Associations of body fat and its changes over time with quality of life and prospective mortality in hemodialysis patients. Am J Clin Nutr 2006; 83: 202–210.
Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH . Association among SF36 quality of life measures and nutrition, hospitalization, and mortality in hemodialysis. J Am Soc Nephrol 2001; 12: 2797–2806.
Evangelista LS, Moser DK, Westlake C, Hamilton MA, Fonarow GC, Dracup K . Impact of obesity on quality of life and depression in patients with heart failure. Eur J Heart Fail 2006; 8: 750–755.
Poston WS, Haddock CK, Conard M, Spertus JA . Impact of obesity on disease-specific health status after percutaneous coronary intervention in coronary disease patients. Int J Obes Relat Metab Disord 2004; 28: 1011–1017.
Milani RV, Lavie CJ, Cassidy MM . Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. Am Heart J 1996; 132: 726–732.
Fine JT, Colditz GA, Coakley EH, Moseley G, Manson JE, Willett WC et al. A prospective study of weight change and health-related quality of life in women. JAMA 1999; 282: 2136–2142.
Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO . A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr 1997; 66: 239–246.
O’Brien PE, Dixon JB, Brown W, Schachter LM, Chapman L, Burn AJ et al. The laparoscopic adjustable gastric band (Lap-Band): a prospective study of medium-term effects on weight, health and quality of life. Obes Surg 2002; 12: 652–660.
Karlsson J, Sjostrom L, Sullivan M . Swedish Obese Subjects (SOS)—an intervention study of obesity. Measuring psychosocial factors and health by means of short-form questionnaires. Results from a method study. J Clin Epidemiol 1995; 48: 817–823.
Sorensen TI . Weight loss causes increased mortality: pros. Obes Rev 2003; 4: 3–7.
Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, VanItallie TB et al. Weight loss increases and fat loss decreases all-cause mortality rates: results from two independent cohort studies. Int J Obes Relat Metab Disord 1999; 23: 603–611.
Katzmarzyk PT, Perusse L, Malina RM, Bouchard C . Seven-year stability of indicators of obesity and adipose tissue distribution in the Canadian population. Am J Clin Nutr 1999; 69: 1123–1129.
Zavaroni I, Ardigo D, Massironi P, Gasparini P, Barilli A, Vetrugno E et al. Do coronary heart disease risk factors change over time. Metabolism 2002; 51: 1022–1102:1022-1102.
De Bacquer D, De Backer G, Cokkinos D, Keil U, Montaye M, Ostor E et al. Overweight and obesity in patients with established coronary heart disease: are we meeting the challenge? Eur Heart J 2004; 25: 121–128.
Acknowledgements
We gratefully acknowledge the cardiac personnel for their diligence in data collection and entry: Foothills Medical Center, Royal Alexandra Hospital and the University of Alberta Hospital. AO is supported by the Heart and Stroke Foundation of Canada Doctoral Research Award and the Gender and Sex Determinants of Cardiovascular Disease: From Bench to Beyond (GENESIS) scholarship; CN is supported by the Alberta Heritage Foundation for Medical Research (AHFMR) and the Canadian Institutes of Health Research (CIHR); KK is supported by a grant from the National Institute of Diabetes, Digestive and Kidney Disease from the National Institute of Health (NIH) and by a grant-in-aid from the American Heart Association; AS is supported by the CIHR and the Heart and Stroke Foundation of Canada; JE is supported by the CIHR and AHFMR; FM is supported by the AHFMR and the Aventis/Merck Frosst Chair in Patient Health Management. APPROACH was initially funded with a grant from the W. Garfield Weston Foundation. The ongoing operation of this project has been made possible by contributions from the Provincial Wide Services Committee of Alberta Health and Wellness and the following industry sponsors: Merck Frosst Canada Inc., Roche Canada, Eli Lilly Canada Inc., Bristol-Myers Squibb, Philips Medical Systems Canada, Searle Pharmaceuticals, Guidant Corporation, Boston Scientific Ltd and Cordis. We appreciate support from the Calgary Health Region, Capital Health Authority, Libin Cardiovascular Institute and Mazankowski Heart Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Oreopoulos, A., Padwal, R., McAlister, F. et al. Association between obesity and health-related quality of life in patients with coronary artery disease. Int J Obes 34, 1434–1441 (2010). https://doi.org/10.1038/ijo.2010.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2010.73
- Springer Nature Limited