Abstract
Purpose
Highly stressful conditions in the operating room are associated with an increased risk of surgical adverse events and worse patient outcomes. Identifying and measuring mental stress in the surgical setting can guide our intervention efforts. The aim of this study was to evaluate the feasibility of heart rate variability (HRV) monitoring as an objective measure of mental stress and its correlation with expertise level in surgical simulation.
Methods
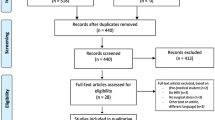
General surgery residents and faculty participated in a laparoscopic hiatal hernia repair simulation on porcine and synthetic models. Whole-procedure electrocardiographic (ECG) data was recorded, and manual artifact correction was performed. On power spectral density analysis, we computed the low-frequency/high-frequency (LF/HF) ratio, considered a surrogate for stress and mental strain. Mental workload was also subjectively assessed using the NASA-TLX rating scale.
Results
We recruited 37 participants: 18 novice, 14 intermediate, and 5 expert surgeons. When comparing the first to the second half of the procedure, the LF/HF ratio (stress level) relatively increased in novices (+ 23% for fundoplication, + 19% for crural repair), decreased in intermediates (− 11% and − 8%, respectively), and decreased in experts (− 40%, − 30%) (p = 0.001, p = 0.009). Pairwise comparison showed significant differences in stress level between novices and experts in both simulation models. NASA-TLX revealed higher mental and physical load among novice trainees, while experts reported greater satisfaction with their performance.
Conclusions
HRV monitoring in surgical simulation is a feasible and effective method to objectively evaluate mental stress and correlate it with the level of surgical expertise. We have shown that the relative change in LF/HF ratio can adequately distinguish between novice and expert surgeons. Our study supports the incorporation of HRV monitoring in surgical simulators to complement objective assessment of technical skills.







Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144(4):371–6. https://doi.org/10.1001/archsurg.2008.575.
Dalager T, Søgaard K, Boyle E, Jensen PT, Mogensen O. Surgery is physically demanding and associated with multisite musculoskeletal pain: a cross-sectional study (in eng). J Surg Res. 2019;240:30–9. https://doi.org/10.1016/j.jss.2019.02.048.
Greenberg AL, et al. Emotional regulation in surgery: fostering well-being, performance, and leadership (in eng). J Surg Res. 2022;277:A25-a35. https://doi.org/10.1016/j.jss.2022.02.032.
Yosef B, Woldegerima Berhe Y, Yilkal Fentie D, Belete Getahun A. Occupational stress among operation room clinicians at ethiopian university hospitals (in eng). J Environ Public Health. 2022;2022:2077317. https://doi.org/10.1155/2022/2077317.
Guerrier G, Margetis D, Agostini C, Machroub Z, Di Maria S. Improving wellness of operating room personnel: a light-based intervention on perceived nursing-related stress (in English). Front Psych. 2021. https://doi.org/10.3389/fpsyt.2021.718194.
Hardy L, Parfitt G. A catastrophe model of anxiety and performance (in eng). Br J Psychol. 1991;82(Pt 2):163–78. https://doi.org/10.1111/j.2044-8295.1991.tb02391.x.
Grantcharov PD, Boillat T, Elkabany S, Wac K, Rivas H. Acute mental stress and surgical performance (in eng). BJS Open. 2019;3(1):119–25. https://doi.org/10.1002/bjs5.104.
Tawfik DS, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors (in eng). Mayo Clin Proc. 2018;93(11):1571–80. https://doi.org/10.1016/j.mayocp.2018.05.014.
Hull L, Arora S, Aggarwal R, Darzi A, Vincent C, Sevdalis N. The impact of nontechnical skills on technical performance in surgery: a systematic review (in eng). J Am Coll Surg. 2012;214(2):214–30. https://doi.org/10.1016/j.jamcollsurg.2011.10.016.
Wetzel CM, et al. The effects of stress and co** on surgical performance during simulations (in eng). Ann Surg. 2010;251(1):171–6. https://doi.org/10.1097/SLA.0b013e3181b3b2be.
Lebares CC, et al. Enhanced stress resilience training in surgeons: iterative adaptation and biopsychosocial effects in 2 small randomized trials (in eng). Ann Surg. 2021;273(3):424–32. https://doi.org/10.1097/sla.0000000000004145.
Jacoby R, Greenfeld Barsky K, Porat T, Harel S, Hanalis Miller T, Goldzweig G. Individual stress response patterns: preliminary findings and possible implications (in eng). PLoS One. 2021;16(8):e0255889. https://doi.org/10.1371/journal.pone.0255889.
Torkamani-Azar M, Lee A, Bednarik R. Methods and measures for mental stress assessment in surgery: a systematic review of 20 years of literature (in eng). IEEE J Biomed Health Inform. 2022;26(9):4436–49. https://doi.org/10.1109/jbhi.2022.3182869.
Walvekar SS, Ambekar JG, Devaranavadagi BB. Study on serum cortisol and perceived stress scale in the police constables (in eng). J Clin Diagn Res. 2015;9(2):BC10–4. https://doi.org/10.7860/jcdr/2015/12015.5576.
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms (in eng). Front Public Health. 2017;5:258. https://doi.org/10.3389/fpubh.2017.00258.
Singh N, Moneghetti KJ, Christle JW, Hadley D, Plews D, Froelicher V. Heart rate variability: an old metric with new meaning in the era of using mHealth technologies for health and exercise training guidance. Part one: physiology and methods (in eng). Arrhythm Electrophysiol Rev. 2018;7(3):193–8. https://doi.org/10.15420/aer.2018.27.2.
The AF, Reijmerink I, van der Laan M, Cnossen F. “Heart rate variability as a measure of mental stress in surgery: a systematic review”, (in eng). Int Arch Occup Environ Health. 2020;93(7):805–21. https://doi.org/10.1007/s00420-020-01525-6.
Amirian I, Toftegård Andersen L, Rosenberg J, Gögenur I. Decreased heart rate variability in surgeons during night shifts (in eng). Can J Surg. 2014;57(5):300–4. https://doi.org/10.1503/cjs.028813.
Wetzel CM, et al. Stress management training for surgeons—a randomized, controlled, intervention study. Ann Surg. 2011;253(3):488–94. https://doi.org/10.1097/SLA.0b013e318209a594.
Hinzmann D, et al. Differences in beginner and expert neurointerventionalists” heart rate variability during simulated neuroangiographies (in eng). Interv Neuroradiol. 2022. https://doi.org/10.1177/15910199221128439.
Ghazali DA, Darmian-Rafei I, Ragot S, Oriot D. Performance under stress conditions during multidisciplinary team immersive pediatric simulations (in eng). Pediatr Crit Care Med. 2018;19(6):e270–8. https://doi.org/10.1097/pcc.0000000000001473.
Baker BG, et al. Simulation fails to replicate stress in trainees performing a technical procedure in the clinical environment (in eng). Med Teach. 2017;39(1):53–7. https://doi.org/10.1080/0142159x.2016.1230188.
Rosser JC Jr, Lynch PJ, Cuddihy L, Gentile DA, Klonsky J, Merrell R. The impact of video games on training surgeons in the 21st century (in eng). Arch Surg. 2007;142(2):181–6. https://doi.org/10.1001/archsurg.142.2.181. (discusssion 186).
Athanasiadis DI, Anton NE, Karim A, Colgate CL, Stefanidis D. Does the advanced training in laparoscopic suturing enhance laparoscopic suturing skill beyond fundamentals of laparoscopic surgery? (in eng). Surgery. 2021;170(4):1125–30. https://doi.org/10.1016/j.surg.2021.06.041.
Neo EL, Zingg U, Devitt PG, Jamieson GG, Watson DI. Learning curve for laparoscopic repair of very large hiatal hernia (in eng). Surg Endosc. 2011;25(6):1775–82. https://doi.org/10.1007/s00464-010-1461-8.
Messick S. Validity of psychological assessment: validation of inferences from persons’ responses and performances as scientific inquiry into score meanING. ETS Res Rep Ser. 1994;1994(2):i–28. https://doi.org/10.1002/j.2333-8504.1994.tb01618.x.
Ghaferi AA, Schwartz TA, Pawlik TM. STROBE Reporting Guidelines for Observational Studies (in eng). JAMA Surg. 2021;156(6):577–8. https://doi.org/10.1001/jamasurg.2021.0528.
Ruha A, Sallinen S, Nissilä S. A real-time microprocessor QRS detector system with a 1-ms timing accuracy for the measurement of ambulatory HRV (in eng). IEEE Trans Biomed Eng. 1997;44(3):159–67. https://doi.org/10.1109/10.554762.
Task Force of the European Society of Cardiology the North A Electrophysiology. Heart rate variability. Circulation. 1996;93(5):1043–65. https://doi.org/10.1161/01.CIR.93.5.1043.
Ritter EM, Gardner AK, Dunkin BJ, Schultz L, Pryor AD, Feldman L. Video-based assessment for laparoscopic fundoplication: initial development of a robust tool for operative performance assessment (in eng). Surg Endosc. 2020;34(7):3176–83. https://doi.org/10.1007/s00464-019-07089-y.
Pagani M, Furlan R, Pizzinelli P, Crivellaro W, Cerutti S, Malliani A. Spectral analysis of R-R and arterial pressure variabilities to assess sympatho-vagal interaction during mental stress in humans (in eng). J Hypertens Suppl. 1989;7(6):S14–5. https://doi.org/10.1097/00004872-198900076-00004.
McCraty R, Atkinson M, Tiller WA, Rein G, Watkins AD. The effects of emotions on short-term power spectrum analysis of heart rate variability (in eng). Am J Cardiol. 1995;76(14):1089–93. https://doi.org/10.1016/s0002-9149(99)80309-9.
Grantcharov PD, Boillat T, Elkabany S, Wac K, Rivas H. Acute mental stress and surgical performance. BJS Open. 2018;3(1):119–25. https://doi.org/10.1002/bjs5.104.
Peabody JE, Ryznar R, Ziesmann MT, Gillman L. A systematic review of heart rate variability as a measure of stress in medical professionals (in eng). Cureus. 2023;15(1): e34345. https://doi.org/10.7759/cureus.34345.
Ghazali DA, et al. Stress response in the daily lives of simulation repeaters. A randomized controlled trial assessing stress evolution over one year of repetitive immersive simulations (in eng). PLoS One. 2019;14(7):e0220111. https://doi.org/10.1371/journal.pone.0220111.
Langelotz C, Scharfenberg M, Haase O, Schwenk W. Stress and heart rate variability in surgeons during a 24-hour shift (in eng). Arch Surg. 2008;143(8):751–5. https://doi.org/10.1001/archsurg.143.8.751.
Green CS, Bavelier D. Exercising your brain: a review of human brain plasticity and training-induced learning (in eng). Psychol Aging. 2008;23(4):692–701. https://doi.org/10.1037/a0014345.
Marrelli M, Gentile S, Palmieri F, Paduano F, Tatullo M. “Correlation between Surgeon’s experience, surgery complexity and the alteration of stress related physiological parameters”, (in eng). PLoS One. 2014;9(11): e112444. https://doi.org/10.1371/journal.pone.0112444.
Awad G, et al. Evaluation of stress levels of trainee cardiac surgery residents during training interventions using physiological stress parameters (in eng). Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182211953.
Stefanidis D, et al. Effectiveness of a comprehensive mental skills curriculum in enhancing surgical performance: results of a randomized controlled trial (in eng). Am J Surg. 2017;213(2):318–24. https://doi.org/10.1016/j.amjsurg.2016.10.016.
Schneider F, et al. Anesthetists’ heart rate variability as an indicator of performance during induction of general anesthesia and simulated critical incidents: an observational study. J Psychophysiol. 2019;33:232–42. https://doi.org/10.1027/0269-8803/a000225.
Acknowledgements
We appreciate the support of the UT Southwestern Simulation Center. We also thank Dave Primm of the UT Southwestern Department of Surgery for help in editing this article.
Funding
This work was supported by the National Institute of Health/National Institute of Biomedical Imaging and Bioengineering grant #R01EB025247.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Emile Farah, Alexis Desir, Carolina Marques, Shruti Hegde, Carla Holcomb, Andres Abreu, Patricio Polanco, Daniel Scott, and Ganesh Sankaranarayanan have no other conflict of interest or financial ties to disclose that are directly or indirectly related to the work submitted for publication.
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farah, E., Desir, A., Marques, C. et al. Heart rate variability: an objective measure of mental stress in surgical simulation. Global Surg Educ 3, 25 (2024). https://doi.org/10.1007/s44186-023-00220-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-023-00220-7