Abstract
Toluidine blue O (TBO) is a phenothiazine dye that, due to its photochemical characteristics and high affinity for biomembranes, has been revealed as a new photosensitizer (PS) option for antimicrobial photodynamic therapy (PDT). This points to a possible association with membranous organelles like mitochondrion. Therefore, here we investigated its effects on mitochondrial bioenergetic functions both in the dark and under photostimulation. Two experimental systems were utilized: (a) isolated rat liver mitochondria and (b) isolated perfused rat liver. Our data revealed that, independently of photostimulation, TBO presented affinity for mitochondria. Under photostimulation, TBO increased the protein carbonylation and lipid peroxidation levels (up to 109.40 and 119.87%, respectively) and decreased the reduced glutathione levels (59.72%) in mitochondria. TBO also uncoupled oxidative phosphorylation and photoinactivated the respiratory chain complexes I, II, and IV, as well as the FoF1-ATP synthase complex. Without photostimulation, TBO caused uncoupling of oxidative phosphorylation and loss of inner mitochondrial membrane integrity and inhibited very strongly succinate oxidase activity. TBO’s uncoupling effect was clearly seen in intact livers where it stimulated oxygen consumption at concentrations of 20 and 40 μM. Additionally, TBO (40 μM) reduced cellular ATP levels (52.46%) and ATP/ADP (45.98%) and ATP/AMP (74.17%) ratios. Consequently, TBO inhibited gluconeogenesis and ureagenesis whereas it stimulated glycogenolysis and glycolysis. In conclusion, we have revealed for the first time that the efficiency of TBO as a PS may be linked to its ability to photodynamically inhibit oxidative phosphorylation. In contrast, TBO is harmful to mitochondrial energy metabolism even without photostimulation, which may lead to adverse effects when used in PDT.
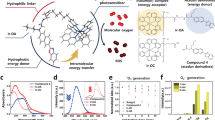
Graphical abstract















Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Will, Y., Shields, J. E., & Wallace, K. B. (2019). Drug-induced mitochondrial toxicity in the geriatric population: Challenges and future directions. Biology, 8(2), 1–14. https://doi.org/10.3390/biology8020032
Will, Y., & Dykens, J. (2014). Mitochondrial toxicity assessment in industry-a decade of technology development and insight. Expert Opinion on Drug Metabolism and Toxicology, 10(8), 1061–1067. https://doi.org/10.1517/17425255.2014.939628
Begriche, K., Massart, J., Robin, M. A., Borgne-Sanchez, A., & Fromenty, B. (2011). Drug-induced toxicity on mitochondria and lipid metabolism: Mechanistic diversity and deleterious consequences for the liver. Journal of Hepatology, 54(4), 773–794. https://doi.org/10.1016/j.jhep.2010.11.006
Rana, P., Aleo, M. D., Gosink, M., & Will, Y. (2019). Evaluation of in vitro mitochondrial toxicity assays and physicochemical properties for prediction of organ toxicity using 228 pharmaceutical drugs. Chemical Research in Toxicology, 32(1), 156–167.
Jaeschke, H. (2018). Mitochondrial dysfunction as a mechanism of drug-induced hepatotoxicity: Current understanding and future perspectives. Journal of Clinical and Translational Research, 4(1), 75–100. https://doi.org/10.18053/jctres.04.201801.005
Wallace, K. B., & Starkov, A. A. (2000). Mitochondrial targets of drug toxicity. Annual Review of Pharmacology and Toxicology, 40, 353–388. https://doi.org/10.1146/annurev.pharmtox.40.1.353
Oleinick, N. L., & Evans, H. H. (1998). The photobiology of photodynamic therapy: Cellular targets and mechanisms. Radiation Research, 150(5 SUPPL.), 146–156. https://doi.org/10.2307/3579816
Morgan, J., & Oseroff, A. R. (2001). Mitochondria-based photodynamic anti-cancer therapy. Advanced Drug Delivery Reviews, 49(1–2), 71–86.
Mahalingam, S. M., Ordaz, J. D., & Low, P. S. (2018). Targeting of a photosensitizer to the Mitochondrion enhances the potency of photodynamic therapy [Research-article]. ACS Omega, 3(6), 6066–6074. https://doi.org/10.1021/acsomega.8b00692
Martins, W. K., Santos, N. F., de Sousa Rocha, C., Bacellar, I. O. L., Tsubone, T. M., Viotto, A. C., Matsukuma, A. Y., de P Abrantes, A. B., Siani, P., Dias, L. G., & Baptista, M. S. (2019). Parallel damage in mitochondria and lysosomes is an efficient way to photoinduce cell death. Autophagy, 15(2), 259–279. https://doi.org/10.1080/15548627.2018.1515609
Chilakamarthi, U., & Giribabu, L. (2017). Photodynamic therapy: Past, present and future. Chemical Record, 17(8), 775–802. https://doi.org/10.1002/tcr.201600121
Plotino, G., Grande, N. M., & Mercade, M. (2019). Photodynamic therapy in endodontics. International Endodontic Journal, 52(6), 760–774. https://doi.org/10.1111/iej.13057
Santos, A. F., Terra, L. F., Wailemann, R. A. M., Oliveira, T. C., Morais Gomes, V., Mineiro, M. F., Meotti, F. C., Bruni-Cardoso, A., Baptista, M. S., & Labriola, L. (2017). Methylene blue photodynamic therapy induces selective and massive cell death in human breast cancer cells. BMC Cancer, 17(1), 1–15. https://doi.org/10.1186/s12885-017-3179-7
Lu, Y., Jiao, R., Chen, X., Zhong, J., Ji, A., & Shen, P. (2008). Methylene blue-mediated photodynamic therapy induces mitochondria-dependent apoptosis in HeLa cell. Journal of Cellular Biochemistry, 105(6), 1451–1460. https://doi.org/10.1002/jcb.21965
Lan, M., Zhao, S., Liu, W., Lee, C. S., Zhang, W., & Wang, P. (2019). Photosensitizers for photodynamic therapy. Advanced Healthcare Materials, 8(13), 1–37. https://doi.org/10.1002/adhm.201900132
Castano, A. P., Demidova, T. N., & Hamblin, M. R. (2004). Mechanisms in photodynamic therapy: Part one—photosensitizers, photochemistry and cellular localization. Photodiagnosis and Photodynamic Therapy, 1, 279–293. https://doi.org/10.1016/S1572-1000(05)00007-4
Oliveira, C. S., Turchiello, R., Kowaltowski, A. J., Indig, G. L., & Baptista, M. S. (2011). Major determinants of photoinduced cell death: Subcellular localization versus photosensitization efficiency. Free Radical Biology and Medicine, 51(4), 824–833. https://doi.org/10.1016/j.freeradbiomed.2011.05.023
Ormond, A. B., & Freeman, H. S. (2013). Dye sensitizers for photodynamic therapy. Materials, 6(3), 817–840. https://doi.org/10.3390/ma6030817
Van Straten, D., Mashayekhi, V., Bruijn, H. S., Oliveira, S., & Robinson, D. J. (2017). Oncologic photodynamic therapy: Basic principles, current clinical status and future directions. Cancers, 9(2), 1–54. https://doi.org/10.3390/cancers9020019
Afkhami, F., Karimi, M., Bahador, A., Ahmadi, P., Pourhajibagher, M., & Chiniforush, N. (2020). Evaluation of antimicrobial photodynamic therapy with toluidine blue against Enterococcus faecalis: Laser vs LED. Photodiagnosis and Photodynamic Therapy. https://doi.org/10.1016/j.pdpdt.2020.102036
Di Stasio, D., Romano, A., Russo, D., Fiori, F., Laino, L., Caponio, V. C. A., Troiano, G., Muzio, L. L., Serpico, R., & Lucchese, A. (2020). Photodynamic therapy using topical toluidine blue for the treatment of oral leukoplakia: A prospective case series. Photodiagnosis and Photodynamic Therapy, 31(June), 101888. https://doi.org/10.1016/j.pdpdt.2020.101888
Harris, F., Sayed, Z., Hussain, S., & Phoenix, D. A. (2004). An investigation into the potential of phenothiazinium-based photo-sensitisers to act as PDT agents. Photodiagnosis and Photodynamic Therapy, 1(3), 231–239. https://doi.org/10.1016/S1572-1000(04)00046-8
Parasuraman, P., Antony, A. P., Sruthil Lal, S. B., et al. (2019). Antimicrobial photodynamic activity of toluidine blue encapsulated in mesoporous silica nanoparticles against Pseudomonas aeruginosa and Staphylococcus aureus. Biofouling, 35, 89–103. https://doi.org/10.1080/08927014.2019.1570501
Valle, L. A., Lopes, M. M. R., Zangrando, M. S. R., Sant’Ana, A. C. P., Greghi, S. L. A., de Rezende, M. L. R., & Damante, C. A. (2019). Blue photosensitizers for aPDT eliminate Aggregatibacter actinomycetemcomitans in the absence of light: An in vitro study. Journal of Photochemistry and Photobiology B: Biology, 194, 56–60. https://doi.org/10.1016/j.jphotobiol.2019.03.005
Souza, R. C., Junqueira, J. C., Rossoni, R. D., Pereira, C. A., Munin, E., & Jorge, A. O. C. (2010). Comparison of the photodynamic fungicidal efficacy of methylene blue, toluidine blue, malachite green and low-power laser irradiation alone against Candida albicans. Lasers in Medical Science, 25(3), 385–389. https://doi.org/10.1007/s10103-009-0706-z
Shen, J., Liang, Q., Su, G., Zhang, Y., Wang, Z., Baudouin, C., & Labbé, A. (2019). In vitro effect of toluidine blue antimicrobial photodynamic chemotherapy on staphylococcus epidermidis and staphylococcus aureus isolated from ocular surface infection. Translational Vision Science and Technology, 8(3), 1–10. https://doi.org/10.1167/tvst.8.3.45
Pinto, A. P., Rosseti, I. B., Carvalho, M. L., da Silva, B. G. M., Alberto-Silva, C., & Costa, M. S. (2018). Photodynamic Antimicrobial Chemotherapy (PACT), using Toluidine blue O inhibits the viability of biofilm produced by Candida albicans at different stages of development. Photodiagnosis and Photodynamic Therapy, 21, 182–189. https://doi.org/10.1016/j.pdpdt.2017.12.001
Balhaddad, A. A., AlQranei, M. S., Ibrahim, M. S., Weir, M. D., Martinho, F. C., Xu, H. H. K., & Melo, M. A. S. (2020). Light energy dose and photosensitizer concentration are determinants of effective photo-killing against caries-related biofilms. International Journal of Molecular Sciences, 21(20), 1–14. https://doi.org/10.3390/ijms21207612
Park, D., Choi, E. J., Weon, K. Y., Lee, W., Lee, S. H., Choi, J. S., Park, G. H., Lee, B., Byun, M. R., Baek, K., & Choi, J. W. (2019). Non-invasive photodynamic therapy against -periodontitis-causing bacteria. Scientific Reports, 9(1), 1–12. https://doi.org/10.1038/s41598-019-44498-4
Usacheva, M. N., Teichert, M. C., & Biel, M. A. (2001). Comparison of the methylene blue and toluidine blue photobactericidal efficacy against gram-positive and gram-negative microorganisms. Lasers in Surgery and Medicine, 29(2), 165–173. https://doi.org/10.1002/lsm.1105
Klosowski, E. M., de Souza, B. T. L., Mito, M. S., Constantin, R. P., Mantovanelli, G. C., Mewes, J. M., Bizerra, P. F. V., da Menezes, P. V. M., Coasta Menezes, Gilglioni, E. H., Utsunomiya, K. S., Marchiosi, R., dos Santos, W. D., Filho, O. F., Caetano, W., de Souza Pereira, P. C., Gonçalves, R. S., Constantin, J., Ishii-Iwamoto, E. L., & Constantin, R. P. (2020). The photodynamic and direct actions of methylene blue on mitochondrial energy metabolism: A balance of the useful and harmful effects of this photosensitizer. Free Radical Biology and Medicine, 153(January), 34–53. https://doi.org/10.1016/j.freeradbiomed.2020.04.015
de Souza, B. T. L., Klosowski, E. M., Mito, M. S., Constantin, R. P., Mantovanelli, G. C., Mewes, J. M., Bizerra, P. F. V., da Silva, F. S. I., da Costa Menezes, P. V. M., Gilglioni, E. H., Utsunomiya, K. S., Marchiosi, R., dos Santos, W. D., Ferrarese-Filho, O., Caetano, W., de Souza Pereira, P. C., Gonçalves, R. S., Constantin, J., Ishii-Iwamoto, E. L., & Constantin, R. P. (2021). The photosensitiser azure A disrupts mitochondrial bioenergetics through intrinsic and photodynamic effects. Toxicology. https://doi.org/10.1016/j.tox.2021.152766
Raimundo, A. F. G., dos Santos, K. B. P., Klosowski, E. M., de Souza, B. T. L., Mito, M. S., Constantin, R. P., Mantovanelli, G. C., Mewes, J. M., Bizerra, P. F. V., da Menezes, P. V. M., Costa, Utsunomiya, K. S., Gilglioni, E. H., Marchiosi, R., dos Dantas Santos, W. D., Ferrarese-Filho, O., Caetano, W., de Souza Pereira, P. C., Gonçalves, R. S., … Constantin, R. P. (2021). The photodynamic and intrinsic effects of Azure B on mitochondrial bioenergetics and the consequences of its intrinsic effects on hepatic energy metabolism. Photodiagnosis and Photodynamic Therapy, 35(April), 102446. https://doi.org/10.1016/j.pdpdt.2021.10244
Chakrabortty, S., Agrawalla, B. K., Stumper, A., Vegi, N. M., Fischer, S., Reichardt, C., Kögler, M., Dietzek, B., Feuring-Buske, M., Buske, C., Rau, S., & Weil, T. (2017). Mitochondria targeted protein-ruthenium photosensitizer for efficient photodynamic applications. Journal of the American Chemical Society, 139(6), 2512–2519. https://doi.org/10.1021/jacs.6b13399
Ramachandran, A., Duan, L., Akakpo, J.Y., & Jaeschke, H. (2018). Mitochondrial dysfunction as a mechanism of drug induced hepatotoxicity: current understanding and future perspectives. Journal of Clinical and Translational Research, 4(1), 75–100. https://doi.org/10.18053/jctres.04.201801.005
Du, K., Ramachandran, A., & Jaeschke, H. (2016). Oxidative stress during acetaminophen hepatotoxicity: Sources, pathophysiological role and therapeutic potential. Redox Biology, 10(September), 148–156. https://doi.org/10.1016/j.redox.2016.10.001
Degli Esposti, D., Hamelin, J., Bosselut, N., Saffroy, R., Sebagh, M., Pommier, A., Martel, C., & Lemoine, A. (2012). Mitochondrial roles and cytoprotection in chronic liver injury. Biochemistry Research International. https://doi.org/10.1155/2012/387626
Scholz, R., & Bücher, T. (1965). Hemoglobin-free perfusion of rat liver. In B. Changce, W. Estabrook, & J. R. Williamson (Eds.), Control of Energy Metabolism (pp. 393–414). New York: Academic Press.
Voss, D., Campello, A. P., & Bacila, M. (1961). The respiratory chain and the oxidative phosphorylation of rat brain mitochondria. Biochemical and Biophysical Research Communications, 4, 48–51. https://doi.org/10.1016/0006-291x(61)90253-4
Bracht, A., Ishii-Iwamoto, E. L. & Salgueiro-Pagadigorria, C. L. (2003). O estudo do metabolismo energético em mitocôndrias isoladas de tecido animal. In: A. Bracht & E. L. Ishii-Iwamoto (Eds.), Métodos de Laboratório em Bioquímica, Manole Ltda. (1st ed., pp. 227–247).
Lowry, O., Rosebrough, N., Farr, A., & Randall, R. (1951). Protein measurement with the Folin phenol reagent. Journal of Biological Chemistry, 193(1), 265–275.
Bolton, J. R., Mayor-Smith, I., & Linden, K. G. (2015). Rethinking the concepts of fluence (UV Dose) and fluence rate: The importance of photon-based units—A systemic review. Photochemistry and Photobiology, 91(6), 1252–1262. https://doi.org/10.1111/php.12512
Salla, G. B. F., Bracht, L., de Sá-Nakanishi, A. B., Parizotto, A. V., Bracht, F., Peralta, R. M., & Bracht, A. (2017). Distribution, lipid-bilayer affinity and kinetics of the metabolic effects of dinoseb in the liver. Toxicology and Applied Pharmacology, 329, 259–271. https://doi.org/10.1016/j.taap.2017.06.013
Guarnier, F. A., Cecchini, A. L., Suzukawa, A. A., Maragno, A. L. G. C., Simão, A. N. C., Gomes, M. D., & Cecchini, R. (2010). Time course of skeletal muscle loss and oxidative stress in rats with walker 256 solid tumor. Muscle & Nerve, 42(6), 950–958. https://doi.org/10.1002/mus.21798
Ohkawa, H., Ohishi, N., & Yagi, K. (1979). Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Analytical Biochemistry, 95(2), 351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Hissin, P. J., & Hilf, R. (1976). A fluorometric method for determination of oxidized and reduced glutathione in tissues. Analytical Biochemistry, 74(1), 214–226. https://doi.org/10.1016/0003-2697(76)90326-2
Ellman, G. L. (1959). Tissue sulfhydryl groups. Archives of Biochemistry and Biophysics, 82(1), 70–77. https://doi.org/10.1016/0003-9861(59)90090-6
Clark, L. C., Jr. (1956). Monitor and control of blood and tissue oxygen tensions. ASAIO Journal, 2(1), 41–48.
Chance, B., & Williams, G. R. (1956). The respiratory chain and oxidative phosphorylation. Advances in Enzymology and Related Areas of Molecular Biology, 17, 65–134. https://doi.org/10.1002/9780470122624.ch2
Singer, T. P. (1974). Determination of the activity of succinate, NADH, choline, and α-glycerophosphate dehydrogenases. Methods of Biochemical Analysis, 22, 123–175. https://doi.org/10.1002/9780470110423.ch3
Pullman, M. E., Penefsky, H. S., Datta, A., & Racker, E. (1960). Partial resolution of the enzymes catalyzing oxidative phosphorylation I. Purification and properties of soluble, dinitrophenol-stimulated adenosine triphosphatase. Journal of Biological Chemistry, 235(11), 3322–3329.
Fiske, C. H., & Subarrow, Y. (1925). The colorimetric determination of phosphorus. Journal of Biological Chemistry, 66(2), 375–400.
Lanza, I. R., & Nair, K. S. (2009). Functional assessment of isolated mitochondria in vitro. Methods in Enzymology, 457, 349–372. https://doi.org/10.1016/S0076-6879(09)05020-4
Gabrielli, D., Belisle, E., Severino, D., Kowaltowski, A. J., & Baptista, M. S. (2004). Binding, aggregation and photochemical properties of methylene blue in mitochondrial suspensions. Photochemistry and Photobiology, 79(3), 227–232. https://doi.org/10.1562/be-03-27.1
Colturato, C. P., Constantin, R. P., Maeda, A. S., Jr., Constantin, R. P., Yamamoto, N. S., Bracht, A., Ishii-Iwamoto, E. L., & Constantin, J. (2012). Metabolic effects of silibinin in the rat liver. Chemico-Biological Interactions. https://doi.org/10.1016/j.cbi.2011.11.006
Bracht, A., Ishii-Iwamoto, E. L. & Kelmer-Bracht, A. M. (2003). O estudo do metabolismo no fígado em perfusão. In: A. Bracht & E. L. Ishii-Iwamoto (Eds.), Métodos de Laboratório em Bioquímica. Manole Ltda (1st ed., pp. 275–289)
Bergmeyer, H. U. (1974). Methods of enzymatic analysis. London: Academic Press.
Shimojo, N., Naka, K., Nakajima, C., Yoshikawa, C., Okuda, K., & Okada, K. (1989). Test-strip method for measuring lactate in whole blood. Clinical Chemistry, 35(9), 1992–1994.
Mihara, K., & Sato, R. (1972). Partial purification of NADH-cytochrome b5 reductase from rabbit liver microsomes with detergents and its properties. Journal of Biochemistry, 71(4), 725–735.
Groot, H. D., Noll, T., & Sies, H. (1985). Oxygen dependence and subcellular partitioning of hepatic menadione-mediated oxygen uptake: Studies with isolated hepatocytes, mitochondria, and microsomes from rat liver in an oxystat system. Archives of Biochemistry and Biophysics, 243(2), 556–562. https://doi.org/10.1016/0003-9861(85)90532-6
Eler, G. J., Peralta, R. M., & Bracht, A. (2009). The action of n-propyl gallate on gluconeogenesis and oxygen uptake in the rat liver. Chemico-Biological Interactions, 181(3), 390–399. https://doi.org/10.1016/j.cbi.2009.07.006
da Silva Simões, M., Bracht, L., Parizotto, A. V., Comar, J. F., Peralta, R. M., & Bracht, A. (2017). The metabolic effects of diuron in the rat liver. Environmental Toxicology and Pharmacology, 54(June), 53–61. https://doi.org/10.1016/j.etap.2017.06.024
Saling, S. C., Comar, J. F., Mito, M. S., Peralta, R. M., & Bracht, A. (2011). Actions of juglone on energy metabolism in the rat liver. Toxicology and Applied Pharmacology, 257(3), 319–327. https://doi.org/10.1016/j.taap.2011.09.004
Mito, M. S., Constantin, J., De Castro, C. V., Yamamoto, N. S., & Bracht, A. (2010). Effects of ranolazine on fatty acid transformation in the isolated perfused rat liver. Molecular and Cellular Biochemistry, 345(1–2), 35–44. https://doi.org/10.1007/s11010-010-0557-8
Schmidt, T. F., Caseli, L., Oliveira, O. N., & Itri, R. (2015). Binding of methylene blue onto Langmuir monolayers representing cell membranes may explain its efficiency as photosensitizer in photodynamic therapy. Langmuir, 31(14), 4205–4212.
Ercan, N. I., Stroeve, P., Tringe, J. W., & Faller, R. (2018). Molecular dynamics modeling of methylene blue− DOPC lipid bilayer interactions. Langmuir, 34(14), 4314–4323. https://doi.org/10.1021/acs.langmuir.8b00372
Schneider, J. M., & Younes, A. (1989). Binding of bepridil to isolated rat heart mitochondria. Basic Research in Cardiology, 84(6), 623–630. https://doi.org/10.1007/BF01906947
Tardivo, J. P., Del Giglio, A., Oliveira, C. S., Gabrielli, D. S., Junqueira, H. C., Tada, D. B., Severino, D., Fátima Turchiello, R., & Baptista, M. S. (2005). Methylene blue in photodynamic therapy: From basic mechanisms to clinical applications. Photodiagnosis and Photodynamic Therapy, 2(3), 175–191. https://doi.org/10.1016/S1572-1000(05)00097-9
Cwiklik, L., & Jungwirth, P. (2010). Massive oxidation of phospholipid membranes leads to pore creation and bilayer disintegration. Chemical Physics Letters, 486(4–6), 99–103. https://doi.org/10.1016/j.cplett.2010.01.010
Itri, R., Junqueira, H. C., Mertins, O., & Baptista, M. S. (2014). Membrane changes under oxidative stress: The impact of oxidized lipids. Biophysical Reviews, 6(1), 47–61. https://doi.org/10.1007/s12551-013-0128-9
Caetano, W., Haddad, P. S., Itri, R., Severino, D., Vieira, V. C., Baptista, M. S., Schröder, A. P., & Marques, C. M. (2007). Photo-induced destruction of giant vesicles in methylene blue solutions. Langmuir, 23(3), 1307–1314. https://doi.org/10.1021/la061510v
Kotova, E. A., Kuzevanov, A. V., Pashkovskaya, A. A., & Antonenko, Y. N. (2011). Selective permeabilization of lipid membranes by photodynamic action via formation of hydrophobic defects or pre-pores. Biochimica et Biophysica Acta - Biomembranes, 1808(9), 2252–2257. https://doi.org/10.1016/j.bbamem.2011.05.018
Almeida, A. M., Oliveira, O. N., & Aoki, P. H. B. (2019). Role of toluidine blue-o binding mechanism for photooxidation in bioinspired bacterial membranes. Langmuir, 35(51), 16745–16751. https://doi.org/10.1021/acs.langmuir.9b03045
Chatterjee, S. R., Srivastava, T. S., Kamat, J. P., & Devasagayam, T. P. A. (1997). Lipid peroxidation induced by a novel porphyrin plus light in isolated mitochondria: Possible implications in photodynamic therapy. Molecular and Cellular Biochemistry, 166(1–2), 25–33. https://doi.org/10.1023/A:1006840714583
Chatterjee, S. R., Shetty, S. J., Srivastava, T. S., & Devasagayam, T. P. (1997). Oxidative damage induced by a novel porphyrin on rat brain mitochondria and its possible implications in therapy. Redox Report, 3(3), 183–188. https://doi.org/10.1080/13510002.1997.11747107
Girotti, A. W. (1990). Photodynamic lipid peroxidation in biological systems. Photochemistry and Photobiology, 51(4), 497–509. https://doi.org/10.1111/j.1751-1097.1990.tb01744.x
Fedorova, M., Bollineni, R. C., & Hoffmann, R. (2014). Protein carbonylation as a major hallmark of oxidative damage: Update of analytical strategies. Mass Spectrometry Reviews, 33(2), 79–97.
Stadtman, E. R., & Levine, R. L. (2003). Free radical-mediated oxidation of free amino acids and amino acid residues in proteins. Amino Acids, 25(3–4), 207–218. https://doi.org/10.1007/s00726-003-0011-2
Gonos, E. S., Kapetanou, M., Sereikaite, J., Bartosz, G., Naparlo, K., Grzesik, M. & Sadowska-Bartosz, I. (2018). Origin and pathophysiology of protein carbonylation, nitration and chlorination in age-related brain diseases and aging. Aging, 10(5), 868–901. https://doi.org/10.18632/aging.101450
Keller, M. A., Piedrafita, G., & Ralser, M. (2015). The widespread role of non-enzymatic reactions in cellular metabolism. Current Opinion in Biotechnology, 34, 153–161. https://doi.org/10.1016/j.copbio.2014.12.020
Kwiecien, S., Jasnos, K., Magierowski, M., Sliwowski, Z., Pajdo, R., Brzozowski, B., Mach, T., Wojcik, D., & Brzozowski, T. (2014). Lipid peroxidation, reactive oxygen species and antioxidative factors in the pathogenesis of gastric mucosal lesions and mechanism of protection against oxidative stress—induced gastric injury. Journal of Physiology and Pharmacology, 65(5), 613–622.
Patlevič, P., Vašková, J., Švorc, P., Vaško, L., & Švorc, P. (2016). Reactive oxygen species and antioxidant defense in human gastrointestinal diseases. Integrative Medicine Research, 5(4), 250–258. https://doi.org/10.1016/j.imr.2016.07.004
Theodossiou, T. A., Olsen, C. E., Jonsson, M., Kubin, A., Hothersall, J. S., & Berg, K. (2017). The diverse roles of glutathione-associated cell resistance against hypericin photodynamic therapy. Redox Biology, 12, 191–197. https://doi.org/10.1016/j.redox.2017.02.018
Hu, J., Wang, T., Zhou, L., & Wei, S. (2020). A ROS responsive nanomedicine with enhanced photodynamic therapy via dual mechanisms: GSH depletion and biosynthesis inhibition. Journal of Photochemistry & Photobiology, B: Biology. https://doi.org/10.1016/j.matdes.2019.108334
Zhang, W., Lu, J., Gao, X., Li, P., Zhang, W., Ma, Y., Wang, H., & Tang, B. (2018). Enhanced photodynamic therapy by reduced levels of intracellular glutathione obtained by employing a nano-MOF with cuii as the active center. Angewandte Chemie—International Edition, 57(18), 4891–4896. https://doi.org/10.1002/anie.201710800
Salgueiro-Pagadigorria, C. L., Kelmer-Bracht, A. M., Bracht, A., & Ishii-Iwamoto, E. L. (1996). Effects of the nonsteroidal anti-inflammatory drug piroxicam on rat liver mitochondria. Comparative Biochemistry and Physiology—C Pharmacology Toxicology and Endocrinology, 113(1), 85–91. https://doi.org/10.1016/0742-8413(95)02041-1
Pivato, L. S., Constantin, R. P., Ishii-Iwamoto, E. L., Kelmer-Bracht, A. M., Yamamoto, N. S., Constantin, J., & Bracht, A. (2006). Metabolic effects of carbenoxolone in rat liver. Journal of Biochemical and Molecular Toxicology. https://doi.org/10.1002/jbt.20139
Shinohara, Y., Bandou, S., Kora, S., Kitamura, S., Inazumi, S., & Terada, H. (1998). Cationic uncouplers of oxidative phosphorylation are inducers of mitochondrial permeability transition. FEBS Letters, 428(1–2), 89–92. https://doi.org/10.1016/S0014-5793(98)00499-289
McLaughlin, S. G., & Dilger, J. P. (1980). Transport of protons across membranes by weak acids. Physiological Reviews, 60(3), 825–863. https://doi.org/10.1152/physrev.1980.60.3.825
Robinson-Duggon, J., Pizarro, N., Gunther, G., Zúñiga-Núñez, D., Edwards, A. M., Greer, A., & Fuentealba, D. (2021). Fatty acid conjugates of toluidine blue o as amphiphilic photosensitizers: Synthesis, solubility, photophysics and photochemical properties. Photochemistry and Photobiology, 97(1), 71–79. https://doi.org/10.1111/php.13304
Atamna, H., Mackey, J., & Dhahbi, J. M. (2012). Mitochondrial pharmacology: Electron transport chain bypass as strategies to treat mitochondrial dysfunction. BioFactors, 38(2), 158–166. https://doi.org/10.1002/biof.197
Poteet, E., Winters, A., Yan, L. J., Shufelt, K., Green, K. N., Simpkins, J. W., Wen, Y., & Yang, S. H. (2012). Neuroprotective actions of methylene blue and its derivatives. PLoS ONE. https://doi.org/10.1371/journal.pone.0048279
Lee, K. K., & Boelsterli, U. A. (2014). Bypassing the compromised mitochondrial electron transport with methylene blue alleviates efavirenz/isoniazid-induced oxidant stress and mitochondria-mediated cell death in mouse hepatocytes. Redox Biology, 2, 599–609. https://doi.org/10.1016/j.redox.2014.03.003
Choudhury, G. R., Winters, A., Rich, R. M., Ryou, M. G., Gryczynski, Z., Yuan, F., Yang, S. H., & Liu, R. (2015). Methylene blue protects astrocytes against glucose oxygen deprivation by improving cellular respiration. PLoS ONE, 10(4), 1–14.
Sevcík, P., & Dunford, H. B. (1991). Kinetics of the oxidation of NADH by methylene blue in a closed system. Journal of Physical Chemistry, 95(6), 2411–2415. https://doi.org/10.1021/j100159a054
Engbersen, J. F. J., Koudijs, A., & van der Plas, H. C. (1985). Reaction of NADH models with methylene blue. Recueil Des Travaux Chimiques Des Pays-Bas, 104(5), 131–138. https://doi.org/10.1002/recl.19851040503
Acco, A., Comar, J. F., & Bracht, A. (2004). Metabolic effects of propofol in the isolated perfused rat liver. Pharmacology & Toxicology, 95(4), 166–174. https://doi.org/10.1002/cbf.290070405
De Souza, A. S., Pagadigorria, C. L. S., Ishii-Iwamoto, E. L., Bracht, A., Cortez, D. A. G., & Yamamoto, N. S. (2009). Effects of the Arrabidaea chica extract on energy metabolism in the rat liver. Pharmaceutical Biology, 47(2), 154–161. https://doi.org/10.1080/13880200802436281
Marek, C. B., Peralta, R. M., Itinose, A. M., & Bracht, A. (2011). Influence of tamoxifen on gluconeogenesis and glycolysis in the perfused rat liver. Chemico-Biological Interactions, 193(1), 22–33. https://doi.org/10.1016/j.cbi.2011.04.010
Scholz, R., Hansen, W., & Thurman, R. G. (1973). Interaction of mixed-function oxidation with biosynthetic processes: Inhibition of gluconeogenesis by aminopyrine in perfused rat liver. European Journal of Biochemistry, 38(1), 64–72. https://doi.org/10.1111/j.1432-1033.1973.tb03034.x
Maldonado, M. R., Bracht, L., de Sá-Nakanishi, A. B., Corrêa, R. C. G., Comar, J. F., Peralta, R. M., & Bracht, A. (2018). Actions of p-synephrine on hepatic enzyme activities linked to carbohydrate metabolism and ATP levels in vivo and in the perfused rat liver. Cell Biochemistry and Function, 36(1), 4–12. https://doi.org/10.1002/cbf.3311
Yamano, K., Yamamoto, K., Katashima, M., Kotaki, H., Takedomi, S., Matsuo, H., Ohtani, H., Sawada, Y., & Iga, T. (2001). Prediction of midazolam—cyp3a inhibitors interaction in the human liver from in vivo/in vitro absorption, distribution, and metabolism data. Drug Metabolism and Disposition, 29(4), 443–452.
Acknowledgements
Emy Luiza Ishii-Iwamoto, Rogério Marchiosi, Osvaldo Ferrarese-Filho, and Wanderley Dantas dos Santos are research fellows of the National Council for Scientific and Technological Development (CNPq). This study was financed in part by the Coordination of Enhancement of Higher Education Personal (CAPES)—Finance Code 001. The authors would like to express their gratitude for the technical assistance of Aparecida Pinto Munhos Hermoso and Célia Akemi Gasparetto. We also gratefully acknowledge the instrumental research facilities provided by the Complexo de Centrais de Apoio à Pesquisa (COMCAP) at the State University of Maringá (UEM).
Funding
This study was supported by grants from the National Council for Scientific and Technological Development (CNPq), Araucaria Foundation (FA), and Coordination for the Improvement of Higher Education Personnel (CAPES). The sponsors had no involvement in the study design, research execution, results interpretation, report writing, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
KBPdS: Investigation and Data Curation; AFGR: Investigation and Data Curation; EMK: Investigation; BTLdS: Investigation; MSM: Investigation; RPC: Investigation; GCM: Investigation; JMM: Investigation; PFVB: Investigation; PVMdCM: Investigation; KSU: Formal analysis; EHG: Formal analysis; RM: Methodology, Formal analysis, Resources, and Writing—Review & Editing; WDdS: Methodology, Formal analysis, and Resources; OFF: Methodology, Formal analysis, and Resources; WC: Conceptualization, Resources and Methodology; PCdSP: Investigation and Methodology; RSG: Investigation and Methodology; JC: Methodology, Formal analysis, and Resources; ELII: Funding acquisition, Conceptualization, Writing—Review & Editing; RPC: Conceptualization, Data curation, Writing—Original Draft, Project administration.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the study reported in this paper.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
dos Santos, K.B.P., Raimundo, A.F.G., Klosowski, E.M. et al. Toluidine blue O directly and photodynamically impairs the bioenergetics of liver mitochondria: a potential mechanism of hepatotoxicity. Photochem Photobiol Sci 22, 279–302 (2023). https://doi.org/10.1007/s43630-022-00312-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-022-00312-1