Abstract
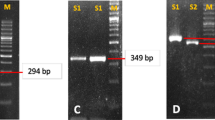
Despite extensive studies on the gastric microbiota, including Helicobacter pylori and non-H. pylori, the bacterial composition in children remains unknown. In this study, we analyzed the culturable gastric bacteria in stomach biopsies from 346 children aged 1–15 years affected by gastric diseases. H. pylori and non-H. pylori were identified by specific PCR and 16S rDNA sequencing, respectively. Antibiotic susceptibilities of H. pylori and non-H. pylori were tested by the E-test and disk diffusion methods, respectively. Rapid diagnosis was also performed by H. pylori–specific PCR. Twenty-two H. pylori strains were obtained from culture, and 92 biopsies were positive by H. pylori–specific PCR. The positive rate was higher in boys (40.3%) than in girls (23.3%) (P = 0.001). Resistance rates of 22 H. pylori strains were as follows: metronidazole, 86.4%; tetracycline, 22.7%; amoxicillin, 22.7%; levofloxacin, 31.8%; clarithromycin, 36.4%. Ten isolates were multidrug-resistant. Additionally, among 366 non-H. pylori strains, 204 exhibited urease activity. Non-H. pylori resistance rates were as follows: metronidazole, 94.8%; tetracycline, 26.2%; amoxicillin, 42.6%; levofloxacin, 15.3%; clarithromycin, 46.7%. Our results showed that children with gastric disorders harbor stomach bacteria with urease activity or nitrate reductase activity. Further studies will determine the effects of non-H. pylori bacteria in gastric diseases.
Similar content being viewed by others
References
Nardone G, Compare D (2015) The human gastric microbiota: is it time to rethink the pathogenesis of stomach diseases? United European Gastroenterol J 3(3):255–260. https://doi.org/10.1177/2050640614566846
Hunt RH, Yaghoobi M (2017) The esophageal and gastric microbiome in health and disease. Gastroenterol Clin N Am 46(1):121–141. https://doi.org/10.1016/j.gtc.2016.09.009
Warren JR, Marshall B (1983) Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1(8336):1273–1275. https://doi.org/10.1016/S0140-6736(83)92719-8
Wang F, Meng W, Wang B, Qiao L (2014) Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett 345(2):196–202. https://doi.org/10.1016/j.canlet.2013.08.016
Bugaytsova JA, Björnham O, Chernov YA, Gideonsson P, Henriksson S, Mendez M, Sjöström R, Mahdavi J, Shevtsova A, Ilver D, Moonens K, Quintana-Hayashi MP, Moskalenko R, Aisenbrey C, Bylund G, Schmidt A, Åberg A, Brännström K, Königer V, Vikström S, Rakhimova L, Hofer A, Ögren J, Liu H, Goldman MD, Whitmire JM, Ådén J, Younson J, Kelly CG, Gilman RH, Chowdhury A, Mukhopadhyay AK, Nair GB, Papadakos KS, Martinez-Gonzalez B, Sgouras DN, Engstrand L, Unemo M, Danielsson D, Suerbaum S, Oscarson S, Morozova-Roche LA, Olofsson A, Gröbner G, Holgersson J, Esberg A, Strömberg N, Landström M, Eldridge AM, Chromy BA, Hansen LM, Solnick JV, Lindén SK, Haas R, Dubois A, Merrell DS, Schedin S, Remaut H, Arnqvist A, Berg DE, Borén T (2017) Helicobacter pylori adapts to chronic infection and gastric disease via pH-responsive BabA-mediated adherence. Cell Host Microbe 21(3):376–389. https://doi.org/10.1016/j.chom.2017.02.013
Li H, Yang T, Liao T, Debowski AW, Nilsson HO, Fulurija A, Haslam SM, Mulloy B, Dell A, Stubbs KA, Marshall BJ, Benghezal M (2017) The redefinition of Helicobacter pylori lipopolysaccharide O-antigen and core-oligosaccharide domains. PLoS Pathog 13(3):e1006280. https://doi.org/10.1371/journal.ppat.1006280
Emara MH, Elhawari SA, Yousef S, Radwan MI, Abdel-Aziz HR (2016) Emerging role of probiotics in the management of Helicobacter pylori infection: histopathologic perspectives. Helicobacter 21(1):3–10. https://doi.org/10.1111/hel.12237
Jiang J, Chen Y, Shi J, Song C, Zhang J, Wang K (2017) Population attributable burden of Helicobacter pylori-related gastric cancer, coronary heart disease, and ischemic stroke in China. Eur J Clin Microbiol Infect Dis 36(2):199–212. https://doi.org/10.1007/s10096-016-2810-x
Tegtmeyer N, Wessler S, Necchi V, Rohde M, Harrer A, Rau TT, Asche CI, Boehm M, Loessner H, Figueiredo C, Naumann M, Palmisano R, Solcia E, Ricci V, Backert S (2017) Helicobacter pylori employs a unique basolateral type IV secretion mechanism for CagA delivery. Cell Host Microbe 22(4):552–560. https://doi.org/10.1016/j.chom.2017.09.005
Sigal M, Logan CY, Kapalczynska M, Mollenkopf HJ, Berger H, Wiedenmann B, Nusse R, Amieva MR, Meyer TF (2017) Stromal R-spondin orchestrates gastric epithelial stem cells and gland homeostasis. Nature 548(7668):451–455. https://doi.org/10.1038/nature23642
Schulz C, Schütte K, Malfertheiner P (2016) Helicobacter pylori and other gastric microbiota in gastroduodenal pathologies. Dig Dis 34(3):210–216. https://doi.org/10.1159/000443353
Franceschi F, Zuccalà G, Roccarina D, Gasbarrini A (2014) Clinical effects of Helicobacter pylori outside the stomach. Nat Rev Gastroenterol Hepatol 11(4):234–242. https://doi.org/10.1038/nrgastro.2013.243
Hunt RH, Camilleri M, Crowe SE, el-Omar EM, Fox JG, Kuipers EJ, Malfertheiner P, McColl KEL, Pritchard DM, Rugge M, Sonnenberg A, Sugano K, Tack J (2015) The stomach in health and disease. Gut 64(10):1650–1668. https://doi.org/10.1136/gutjnl-2014-307595
Sheh A, Fox JG (2013) The role of the gastrointestinal microbiome in Helicobacter pylori pathogenesis. Gut Microbes 4(6):505–531. https://doi.org/10.4161/gmic.26205
Coker OO, Dai Z, Nie Y, Zhao G, Cao L, Nakatsu G, Wu WKK, Wong SH, Chen Z, Sung JJY, Yu J (2017) Mucosal microbiome dysbiosis in gastric carcinogenesis. Gut 67:1024–1032. https://doi.org/10.1136/gutjnl-2017-314281
Yin L, Liu F, Guo CC et al (2016) Investigation of clinical significance of Pseudomonas putida isolated from gastric biopsies. Chin J Zoonoses 32(12):1102–1107 (In Chinese)
Hu Y, He LH, **ao D, Liu GD, Gu YX, Tao XX, Zhang JZ (2012) Bacterial flora concurrent with Helicobacter pylori in the stomach of patients with upper gastrointestinal diseases. World J Gastroenterol 18(11):1257–1261. https://doi.org/10.3748/wjg.v18.i11.1257
Khosravi Y, Dieye Y, Poh BH et al (2014) Culturable bacterial microbiota of the stomach of Helicobacter pylori positive and negative gastric disease patients. Scientific World J 2014:610421. https://doi.org/10.1155/2014/610421
Chen D, Cunningham SA, Cole NC et al (2017) Phenotypic and molecular antimicrobial susceptibility of Helicobacter pylori. Antimicrob Agents Chemother 61(4):e02530–e02516. https://doi.org/10.1128/AAC.02530-16
Thoreson AC, Borre MB, Andersen LP et al (1995) Development of a PCR-based technique for detection of Helicobacter pylori. Fems Immunol Med Mic 10(3–4):325–334
Wei G, Lu H, Zhou Z, **e H, Wang A, Nelson K, Zhao L (2007) The microbial community in the feces of the giant panda (Ailuropoda melanoleuca) as determined by PCR-TGGE profiling and clone library analysis. Microb Ecol 54(1):194–202. https://doi.org/10.1007/s00248-007-9225-2
Ogata SK, Gales AC, Kawakami E (2014) Antimicrobial susceptibility testing for Helicobacter pylori isolates from Brazilian children and adolescents: comparing agar dilution, E-test, and disk diffusion. Bra J Mic 45(4):1439–1448
Liou JM, Chen CC, Chang CY, Chen MJ, Chen CC, Fang YJ, Lee JY, Yang TH, Luo JC, Wu JY, Liou TC, Chang WH, Hsu YC, Tseng CH, Chang CC, Bair MJ, Liu TY, Hsieh CF, Tsao FY, Shun CT, Lin JT, Lee YC, Wu MS, Taiwan Gastrointestinal Disease and Helicobacter Consortium (2016) Sequential therapy for 10 days versus triple therapy for 14 days in the eradication of Helicobacter pylori in the community and hospital populations: a randomised trial. Gut 65(11):1784–1792. https://doi.org/10.1136/gutjnl-2015-310142
Liou JM, Chen CC, Chang CY, Chen MJ, Fang YJ, Lee JY, Chen CC, Hsu SJ, Hsu YC, Tseng CH, Tseng PH, Chang L, Chang WH, Wang HP, Shun CT, Wu JY, Lee YC, Lin JT, Wu MS, on behalf of the Taiwan Helicobacter Consortium (2013) Efficacy of genotypic resistance-guided sequential therapy in the third-line treatment of refractory Helicobacter pylori infection: a multicentre clinical trial. J Antimicrob Chemother 68(2):450–456. https://doi.org/10.1093/jac/dks407
CLSI (ed) (2018) Performance standards for antimicrobial susceptibility testing. 28th ed. CLSI supplement M100. Clinical and Laboratory Standards Institute, Wayne
Inoue M (2017) Changing epidemiology of Helicobacter pylori in Japan. Gastric Cancer 20(1):3–7. https://doi.org/10.1007/s10120-016-0658-5
Nagy P, Johansson S, Molloy-Bland M (2016) Systematic review of time trends in the prevalence of Helicobacter pylori, infection in China and the USA. Gut Pathog 8:8. https://doi.org/10.1186/s13099-016-0091-7
Ueda J, Gosho M, Inui Y, Matsuda T, Sakakibara M, Mabe K, Nakajima S, Shimoyama T, Yasuda M, Kawai T, Murakami K, Kamada T, Mizuno M, Kikuchi S, Lin Y, Kato M (2014) Prevalence of Helicobacter pylori infection by birth year and geographic area in Japan. Helicobacter 19(2):105–110. https://doi.org/10.1111/hel.12110
Wangda S, Richter JM, Kuenzang P, Wangchuk K, Choden T, Tenzin K, Malaty HM (2017) Epidemiology of Helicobacter pylori infection in asymptomatic school children in Bhutan. Helicobacter 22(6):e12439. https://doi.org/10.1111/hel.12439
Ibrahim A, Morais S, Ferro A, Lunet N, Peleteiro B (2017) Sex-differences in the prevalence of Helicobacter pylori infection in pediatric and adult populations: systematic review and meta-analysis of 244 studies. Dig Liver Dis 49(7):742–749. https://doi.org/10.1111/hel.12439
Zincir H, Kaya Erten Z, Özkan F, Sevig Ü, Baser M, Elmali F (2012) Prevalence of urinary tract infections and its risk factors in elementary school students. Urol Int 88(2):194–197. https://doi.org/10.1111/hel.12439
de Martel C, Parsonnet J (2006) Helicobacter pylori infection and gender: a meta-analysis of population-based prevalence surveys. Dig Dis Sci 51(12):2292–2301. https://doi.org/10.1007/s10620-006-9210-5
Shao Y, Lu R, Yang Y et al (2017) Antibiotic resistance of Helicobacter pylori to 16 antibiotics in clinical patients. J Clin Lab Anal e22339. https://doi.org/10.1002/jcla.22339
Hu Y, Zhu Y, Lu NH (2017) Primary antibiotic resistance of Helicobacter pylori in China. Dig Dis Sci 62(5):1146–1154. https://doi.org/10.1007/s10620-017-4536-8
Li L, Ke Y, Yu C, Li G, Yang N, Zhang J, Li Y (2017) Antibiotic resistance of Helicobacter pylori in Chinese children: a multicenter retrospective study over 7 years. Helicobacter 22(3):e12373. https://doi.org/10.1111/hel.12373
Rook G, Bäckhed F, Levin BR, McFall-Ngai MJ, McLean AR (2017) Evolution, human-microbe interactions, and life history plasticity. Lancet 390(10093):521–530. https://doi.org/10.1016/S0140-6736(17)30566-4
Sanduleanu S, Jonkers D, De Bruïne A et al (2001) Double gastric infection with Helicobacter pylori, and non-Helicobacter pylori, bacteria during acid-suppressive therapy: increase of pro-inflammatory cytokines and development of atrophic gastritis. Aliment Pharmacol Ther 15(8):1163–1175. https://doi.org/10.1046/j.1365-2036.2001.01029.x
Ferreira RM, Pereira-Marques J, Pinto-Ribeiro I, Costa JL, Carneiro F, Machado JC, Figueiredo C (2018) Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut 67(2):226–236. https://doi.org/10.1136/gutjnl-2017-314205
Tlaskalová-Hogenová H, Štěpánková R, Kozáková H, Hudcovic T, Vannucci L, Tučková L, Rossmann P, Hrnčíř T, Kverka M, Zákostelská Z, Klimešová K, Přibylová J, Bártová J, Sanchez D, Fundová P, Borovská D, Šrůtková D, Zídek Z, Schwarzer M, Drastich P, Funda DP (2011) The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases. Cell Mol Immunol 8(2):110–120. https://doi.org/10.1038/cmi.2010.67
Wang ZK, Yang YS (2013) Upper gastrointestinal microbiota and digestive diseases. World J Gastroenterol 19(10):1540–1550. https://doi.org/10.3748/wjg.v19.i10.1541
He C, Yang Z, Lu N (2016) Imbalance of gastrointestinal microbiota in the pathogenesis of Helicobacter pylori-associated diseases. Helicobacter 21(5):337–348. https://doi.org/10.1111/hel.12297
Brawner KM, Morrow CD, Smith PD (2014) Gastric microbiome and gastric cancer. Cancer J 20(3):211–216. https://doi.org/10.1097/PPO.0000000000000043
Zilberstein B, Quintanilha AG, Santos MA et al (2007) Digestive tract microbiota in healthy volunteers. Clinics (Sao Paulo) 62(1):47–54
Osaki T, Mabe K, Hanawa T, Kamiya S (2008) Urease-positive bacteria in the stomach induce a false-positive reaction in a urea breath test for diagnosis of Helicobacter pylori infection. J Med Microbiol 57(7):814–819. https://doi.org/10.1099/jmm.0.47768-0
Michaud L, Gottrand F, Ganga-Zandzou PS et al (1998) Gastric bacterial overgrowth is a cause of false positive diagnosis of Helicobacter pylori infection using 13C urea breath test. Gut 42(4):594–595
Patel SK, Pratap CB, Verma AK, Jain AK, Dixit VK, Nath G (2013) Pseudomonas fluorescens-like bacteria from the stomach: a microbiological and molecular study. World J Gastroenterol 19(7):1056–1067. https://doi.org/10.3748/wjg.v19.i7.1056
Kulkarni G, Gohil K, Misra V, Kakrani AL, Misra SP, Patole M, Shouche Y, Dharne M (2017) Multilocus sequence ty** of Ochrobactrum spp. isolated from gastric niche. J Infect Public Health 10(2):201–210. https://doi.org/10.1016/j.jiph.2016.04.013
Zeng B, Sun L, Chen Y, Qian Y, Cao Q, Zhang Z, Li Z (2018) Neisseria flavescens: a urease-expressing potential pathogen isolated from gastritis patients. Cur Microbiol 75(2):186–193. https://doi.org/10.1007/s00284-017-1364-1
Tsuzukibashi O, Uchibori S, Kobayashi T, Umezawa K, Mashimo C, Nambu T, Saito M, Hashizume-Takizawa T, Ochiai T (2017) Isolation and identification methods of Rothia species in oral cavities. J Microbiol Methods 134:21–26. https://doi.org/10.1016/j.mimet.2017.01.005
Zamakhchari M, Wei G, Dewhirst F, Lee J, Schuppan D, Oppenheim FG, Helmerhorst EJ (2011) Identification of Rothia bacteria as gluten-degrading natural colonizers of the upper gastro-intestinal tract. PLoS One 6(9):e24455. https://doi.org/10.1371/journal.pone.0024455
Nicodemo AC, Gonçalves LG, Odongo FC et al (2014) Rothia aeria endocarditis in a patient with a bicuspid aortic valve: case report. Braz J Infect Dis 18(5):561–564. https://doi.org/10.1016/j.bjid.2014.05.001
Geng X, Li W, Chen Z et al (2017) The bifunctional enzyme SpoT is involved in the clarithromycin tolerance of Helicobacter pylori by upregulating the transporters HP0939, HP1017, HP0497, and HP0471. Antimicrob Agents Chemother 61(5):e02011–e02016. https://doi.org/10.1128/AAC.02011-16
Acknowledgements
We would like to thank Editage [www.editage.cn] for the English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81460314 and 3176080034), Foundation of Education Department of Guizhou (Project number: KY-2014-216), and Foundation of Guiyang Health and Family Planning Commission (No. 2014-018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible Editor: Ana Lucia Darini
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, C., Liu, F., Zhu, L. et al. Analysis of culturable microbiota present in the stomach of children with gastric symptoms. Braz J Microbiol 50, 107–115 (2019). https://doi.org/10.1007/s42770-018-0030-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-018-0030-5