Key summary points
The aim of this systematic review was to quantify the association between low calf circumference and mortality.
AbstractSection FindingsLow calf circumference (CC) was associated with a higher risk of mortality than normal calf circumference, with a pooled HR of 2.42 (95% CI 1.97–2.97, I2 = 74.3.0%). In addition, this association between low calf circumference and morality was still statistically significant in the subgroup analysis across different settings, including hospitals, nursing homes and communities.
AbstractSection MessageCalf circumference, which is simple and convenient to measure, could be used to stratify the high-risk groups, as low calf circumference was significantly associated with mortality among patients.
Abstract
Purpose
Low calf circumference is an important indicator of malnutrition and has been widely studied, especially among older adults. However, data on the association between low calf circumference and mortality have been inconsistent. This systematic review was aimed to quantify this association.
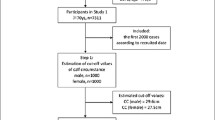
Methods
The internet databases (PubMed, Embase, ScienceDirect and Cochrane Library databases) were systematically searched from inception to November 01, 2021 for studies investigating the association between low calf circumference and mortality. A random effects model was adopted to pool the relevant data.
Results
Low calf circumference was associated with a higher risk of mortality than normal calf circumference, with a pooled HR of 2.42 (95% CI 1.97–2.97, I2 = 74.3%). In addition, this association between low calf circumference and morality was still statistically significant in the subgroup analysis across different settings, including hospitals (pooled HR = 2.63, 95% CI 1.93–3.58), nursing homes (pooled HR = 2.49, 95% CI 1.76–3.54), and communities (pooled HR = 2.22, 95% CI 1.60–3.07). Other subgroup analyses based on different cutoffs of calf circumference showed that, compared to individual with normal calf circumference, participants with low calf circumference had an increased risk of mortality (pooled HR = 2.66, 95% CI 2.06–3.43) when using the Asian Working Group for Sarcopenia (AWGS) criterion (≤ 34 cm for males and ≤ 33 cm for females). Similar results were found when the Mini Nutritional Assessment (MNA) criterion (≤ 31 cm) was used, with a pooled HR of 2.11 (95% CI 1.59–2.81).
Conclusion
Calf circumference, which is simple and convenient to measure, could be used to stratify the high-risk group, as low calf circumference was significantly associated with mortality among patients. Interventions, including exercise and nutrition programs, could be conducted promptly once low calf circumference is detected.





Similar content being viewed by others
Availability of data and materials
The data sets generated and/or analyzed during the current study are available in the PubMed database.
Code availability
Not applicable.
References
Damayanthi H, Moy FM, Abdullah KL, Dharmaratne SD (2018) Prevalence of malnutrition and associated factors among community-dwelling older persons in Sri Lanka: a cross-sectional study. BMC Geriatr 18(1):199
Corkins MR, Guenter P, DiMaria-Ghalili RA, Jensen GL, Malone A, Miller S, Patel V, Plogsted S, Resnick HE (2014) Malnutrition diagnoses in hospitalized patients: United States, 2010. JPEN J Parenter Enteral Nutr 38(2):186–195
Hegendörfer E, VanAcker V, Vaes B, Degryse JM: Malnutrition risk and its association with adverse outcomes in a Belgian cohort of community-dwelling adults aged 80 years and over. Acta Clinica Belgica 2020:1–8.
Eckert C, Gell NM, Wingood M, Schollmeyer J, Tarleton EK (2021) Malnutrition risk, rurality, and falls among community-dwelling older adults. J Nutr Health Aging 25(5):624–627
Sharma Y, Miller M, Kaambwa B, Shahi R, Hakendorf P, Horwood C, Thompson C (2017) Malnutrition and its association with readmission and death within 7 days and 8–180 days postdischarge in older patients: a prospective observational study. BMJ Open 7(11):e018443
White JV, Guenter P, Jensen G, Malone A, Schofield M (2012) Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr 36(3):275–283
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, Baptista G, Barazzoni R, Blaauw R, Coats A et al (2019) GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr (Edinburgh, Scotland) 38(1):1–9
Zhang XM, Wu X, Ma Y, Zhu C, Cao J, Liu G, Li FF, Cheng ASK (2021) Comparing the performance of calf circumference, albumin, and BMI for predicting mortality in immobile patients. Risk Manag Healthcare Policy 14:2289–2300
Zhang XM, Chen D, **e XH, Zhang JE, Zeng Y, Cheng AS (2021) Sarcopenia as a predictor of mortality among the critically ill in an intensive care unit: a systematic review and meta-analysis. BMC Geriatr 21(1):339
Zhang X, Huang P, Dou Q, Wang C, Zhang W, Yang Y, Wang J, **e X, Zhou J, Zeng Y (2020) Falls among older adults with sarcopenia dwelling in nursing home or community: a meta-analysis. Clin Nutr (Edinburgh, Scotland) 39(1):33–39
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S et al (2020) Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 21(3):300-307.e302
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31
Fernandes DPS, Juvanhol LL, Lozano M, Ribeiro AQ (2021) Calf circumference is an independent predictor of mortality in older adults: An approach with generalized additive models. Nutr Clin Pract
Leandro-Merhi VA, de Aquino JLB, Reis LO (2017) Predictors of Nutritional Risk According to NRS-2002 and Calf Circumference in Hospitalized Older Adults with Neoplasms. Nutr Cancer 69(8):1219–1226
Real GG, Frühauf IR, Sedrez JHK, Dall’Aqua EJF, Gonzalez MC (2018) Calf circumference: a marker of muscle mass as a predictor of hospital readmission. JPEN J Parenter Enteral Nutr 42(8):1272–1279
Moon S, Hong GS (2020) Predictive factors of mortality in older adult residents of long-term care facilities. J Nurs Res 28(2):e82
Abreo AP, Bailey SR, Abreo K (2021) Associations between calf, thigh, and arm circumference and cardiovascular and all-cause mortality in NHANES 1999–2004. Nutr Metab Cardiovasc Dis 31(5):1410–1415
Cardoso AS, Xavier MO, Dos Santos CC, Tomasi E, Cesar JA, Gonzalez MC, Domingues MR, Barbosa-Silva TG, Bielemann RM (2020) Body mass index and mortality among community-dwelling elderly of Southern Brazil. Prevent Med 139:106173
Tsai AC, Lai MC, Chang TL (2012) Mid-arm and calf circumferences (MAC and CC) are better than body mass index (BMI) in predicting health status and mortality risk in institutionalized elderly Taiwanese. Arch Gerontol Geriatr 54(3):443–447
Nishikawa H, Yoh K, Enomoto H, Nishimura T, Nishiguchi S, Iijima H (2021) Combined grip strength and calf circumference as a useful prognostic system in patients with liver diseases: a large cohort study. Ann Transl Med 9(8):624
Sousa IM, Bielemann RM, Gonzalez MC, da Rocha IMG, Barbalho ER, de Carvalho ALM, Dantas MAM, de Medeiros GOC, Silva FM, Fayh APT: Low calf circumference is an independent predictor of mortality in cancer patients: A prospective cohort study. Nutrition (Burbank, Los Angeles County, Calif) 2020, 79–80:110816.
Easton JF, Stephens CR, Román-Sicilia H, Cesari M, Pérez-Zepeda MU (2018) Anthropometric measurements and mortality in frail older adults. Exp Gerontol 110:61–66
Rodrigues J, Santin F, Brito F, Lindholm B, Stenvinkel P, Avesani CM (2019) Nutritional status of older patients on hemodialysis: Which nutritional markers can best predict clinical outcomes? Nutrition (Burbank, Los Angeles County, Calif) 65:113–119
de Almeida Roediger M, de Fátima Nunes Marucci M, Quintiliano Scarpelli Dourado DA, de Oliveira C, Licio Ferreira Santos J, de Oliveira Duarte YA (2019) Body Composition Changes and 10-Year Mortality Risk in Older Brazilian Adults: Analysis of Prospective Data from the SABE Study. J Nutr Health Aging 23(1):51–59
de Sousa OV, Mendes J, Amaral TF (2020) Nutritional and Functional Indicators and Their Association With Mortality Among Older Adults With Alzheimer’s Disease. Am J Alzheimers Dis Other Demen 35:1533317520907168
Ho SC, Wang JY, Kuo HP, Huang CD, Lee KY, Chuang HC, Feng PH, Chen TT, Hsu MF (2016) Mid-arm and calf circumferences are stronger mortality predictors than body mass index for patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 11:2075–2080
Bernardes S, Silva FM, da Costa CC, de Souza RM, Teixeira PJZ (2021) Reduced calf circumference is an independent predictor of worse quality of life, severity of disease, frequent exacerbation, and death in patients with chronic obstructive pulmonary disease admitted to a pulmonary rehabilitation program: A historic cohort study. JPEN J Parent Enteral Nutr
Aliberti MJR, Szlejf C, Covinsky KE, Lee SJ, Jacob-Filho W, Suemoto CK (2020) Prognostic value of a rapid sarcopenia measure in acutely ill older adults. Clin Nutr (Edinburgh, Scotland) 39(7):2114–2120
Tarnowski M, Stein E, Marcadenti A, Fink J, Rabito E, Silva FM (2020) Calf circumference is a good predictor of longer hospital stay and nutritional risk in emergency patients: a prospective cohort study. J Am Coll Nutr 39(7):645–649
Teixeira PP, Kowalski VH, Valduga K, de Araújo BE, Silva FM (2020) Low Muscle Mass Is a Predictor of Malnutrition and Prolonged Hospital Stay in Patients With Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Longitudinal Study. J Parent Enteral Nutr
Yajima Y, Kikutani T, Tamura F, Yoshida M (2017) Relationship between tongue strength and 1-year life expectancy in elderly people needing nursing care. Odontology 105(4):477–483
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Valmorbida E, Trevisan C, Imoscopi A, Mazzochin M, Manzato E, Sergi G (2020) Malnutrition is associated with increased risk of hospital admission and death in the first 18 months of institutionalization. Clin Nutr (Edinburgh, Scotland) 39(12):3687–3694
de Sousa IM, Silva FM, de Carvalho ALM, da Rocha IMG, Fayh APT (2021) Accuracy of isolated nutrition indicators in diagnosing malnutrition and their prognostic value to predict death in patients with gastric and colorectal cancer: A prospective study. J Parent Enteral Nutr
Bourdel-Marchasson I, Diallo A, Bellera C, Blanc-Bisson C, Durrieu J, Germain C, Mathoulin-Pélissier S, Soubeyran P, Rainfray M, Fonck M et al (2016) One-year mortality in older patients with cancer: development and external validation of an MNA-based prognostic score. PloS One 11(2):e0148523
Rogeri PS, Gasparini SO, Martins GL, Costa LKF, Araujo CC, Lugaresi R, Kopfler M, Lancha AH, Jr. (2020) Crosstalk Between Skeletal Muscle and Immune System: Which Roles Do IL-6 and Glutamine Play? Front Physiol 11:582258
Mukund K, Subramaniam S (2020) Skeletal muscle: a review of molecular structure and function, in health and disease. Wiley Interdiscip Rev Syst Biol Med 12(1):e1462
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet (London, England) 393(10191):2636–2646
**a L, Zhao R, Wan Q, Wu Y, Zhou Y, Wang Y, Cui Y, Shen X, Wu X (2020) Sarcopenia and adverse health-related outcomes: an umbrella review of meta-analyses of observational studies. Cancer Med 9(21):7964–7978
Liu P, Hao Q, Hai S, Wang H, Cao L, Dong B (2017) Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: aA systematic review and meta-analysis. Maturitas 103:16–22
Zhang X, Wang C, Dou Q, Zhang W, Yang Y, **e X (2018) Sarcopenia as a predictor of all-cause mortality among older nursing home residents: a systematic review and meta-analysis. BMJ Open 8(11):e021252
Volpi E, Nazemi R, Fujita S (2004) Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care 7(4):405–410
Mrowka R, Westphal A (2018) Skeletal muscle in the fight against chronic diseases. Acta Physiol (Oxford, England) 223(4):e13086
Li Z, Cui M, Yu K, Zhang XW, Li CW, Nie XD, Wang F (2021) Effects of nutrition supplementation and physical exercise on muscle mass, muscle strength and fat mass among sarcopenic elderly: a randomized controlled trial. Appl Physiol Nutr Metab 46(5):494–500
de Santana FM, Premaor MO, Tanigava NY, Pereira RMR (2021) Low muscle mass in older adults and mortality: a systematic review and meta-analysis. Exp Gerontol 152:111461
Wulan SN, Westerterp KR, Plasqui G (2010) Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas 65(4):315–319
Monereo-Muñoz M, Martín-Ponce E, Hernández-Luis R, Quintero-Platt G, Gómez-Rodríguez-Bethencourt M, González-Reimers E, Santolaria F (2019) Prognostic value of muscle mass assessed by DEXA in elderly hospitalized patients. Clin Nutr ESPEN 32:118–124
Acknowledgements
The authors thank the staff of Peking Union Medical College and People's Hospital of Baoan, Shenzhen, for their guidance and support.
Funding
This work was not supported by any funding.
Author information
Authors and Affiliations
Contributions
XJW, XMZ and WWZ were responsible for the concept and design. JW and XMZ helped design the study and wrote the initial manuscript. JJ and CLC collected data. Screening and selecting the articles were conducted by WYT and YJY. XMZ and JW extracted all of the raw data and finished the assessment of the quality of bias. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The author(s) declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Approval was obtained from all authors.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wei, J., Jiao, J., Chen, CL. et al. The association between low calf circumference and mortality: a systematic review and meta-analysis. Eur Geriatr Med 13, 597–609 (2022). https://doi.org/10.1007/s41999-021-00603-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00603-3