Abstract
Introduction
The presence of atypical squamous cells of undetermined significance (ASCUS) from pap smear result should be followed by cytology follow-up, HPV DNA testing, or colposcopy, as there is a possibility of progress to cervical cancer. This study aims to evaluate the frequency of distinct HPV genotypes and colposcopy findings among women with ASCUS cytology results.
Methods
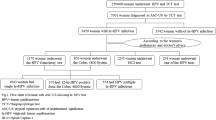
A descriptive study in 846 women was conducted in Dr. Cipto Mangunkusumo General Hospital using retrospective data between 2016 and 2018. Of 124 patients with ASCUS cytology results, all had HPV DNA examinations, but only 63 had colposcopy examinations. Participants who were married, sexually active, and willing to participate were included. Patients with incomplete data were excluded. The data were processed using Statistical Product and Service Solutions (SPSS) version 25.0.
Results
The incidence of ASCUS in the population was 14.7%. Among 124 subjects with ASCUS, 47 (37.9%) had a high-risk HPV infection. From 63 ASCUS women who underwent colposcopy, 27 subjects (42.8%) were normal. Type 52 of HPV showed the most frequent genotype appearing, especially within 30–50 years of age.
Conclusion
42.8% of the colposcopy findings for women with ASCUS were normal, and 37.9% of ASCUS women had a high-risk HPV infection. Type 52 was found to be the most frequent genotype that appears in ASCUS patients in Indonesia.
Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
WHO. Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. WHO Guidelines. 2013;60.
Solomon D, Davey D, Kurman R, Moriarty A, O’Connor D, Prey M, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002;287(16):2114–9.
Nayar R, Wilbur DC. The Bethesda system for reporting cervical cytology: definitions, criteria, and explanatory notes. 3rd ed. New York: Springer; 2015.
Marcos Lopes AC, Campaner AB, Henrique LQ. Prevalence of high-grade intraepithelial neoplasia in patients with cytology presenting atypical squamous cells of undetermined significance. Acta Cytol. 2016;60(2):139–44.
Kombe Kombe AJ, Li B, Zahid A, Mengist HM, Bounda GA, Zhou Y, et al. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Public Health. 2021;8: 552028.
Corneanu LM, Stănculescu D, Corneanu C. HPV and cervical squamous intraepithelial lesions: clinicopathological study. Rom J Morphol Embryol. 2011;52(1):89–94.
Molloy M, Comer R, Rogers P, Dowling M, Meskell P, Asbury K, et al. High risk HPV testing following treatment for cervical intraepithelial neoplasia. Ir J Med Sci. 2016;185(4):895–900.
Chen CA, Liu CY, Chou H, Chou C, Ho C, Twu N, et al. The distribution and differential risks of human papillomavirus genotypes in cervical preinvasive lesions: a Taiwan Cooperative Oncologic Group Study. Int J Gynecol Cancer. 2006;16:180Q1808.
Abreu ALP, Souza RP, Gimenes F, Consolaro MEL. A review of methods for detect human Papillomavirus infection. Virol J. 2012;9:262.
Agorastos T, Chatzistamatiou K, Katsamagkas T, Koliopoulos G, Daponte A, Constantinidis T, et al. Primary screening for cervical cancer based on high-risk human papillomavirus (HPV) detection and HPV 16 and HPV 18 genoty**, in comparison to cytology. PLoS ONE. 2015;10(3): e0119755.
Bornstein J, Bentley J, Bösze P, Girardi F, Haefner H, Menton M, et al. colposcopic terminology of the international federation for cervical pathology and colposcopy. Obstet Gynecol. 2011;120:166–72.
Dursun P, Senger SS, Arslan H, Kuşçu E, Ayhan A. Human papillomavirus (HPV) prevalence and types among Turkish women at a gynecology outpatient unit. BMC Infect Dis. 2009;9(1):191. https://doi.org/10.1186/1471-2334-9-191.
Lee SJ, Jung KL, Lee JW, Song SY, Kim BG, Lee JH, et al. Analyses of atypical squamous cells refined by the 2001 Bethesda System: the distribution and clinical significance of follow-up management. Int J Gynecol Cancer. 2006;16(2):664–9.
Barcelos ACM, Michelin MA, Adad SJ, Murta EFC. Atypical squamous cells of undetermined significance: Bethesda classification and association with human papillomavirus. Infect Dis Obstet Gynecol. 2011;2011:1–9.
Srodon M, Parry Dilworth H, Ronnett BM. Atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion: diagnostic performance, human papillomavirus testing, and follow-up results. Cancer. 2006;108(1):32–8.
Martín P, Kilany L, García D, López-García AM, Martín-Azaña MJ, Abraira V, et al. Human papillomavirus genotype distribution in Madrid and correlation with cytological data. BMC Infect Dis. 2011;11:2–6.
Wang Z, Gu Y, Wang H, Chen J, Zheng Y, Cui B, et al. Distribution of cervical lesions in high-risk HPV (hr-HPV) positive women with ASC-US: a retrospective single-center study in China. Virol J. 2020;17(1):1–10.
Tota J, Franco EL. HPV infection and cervical carcinogenesis:epidemiology and prevention. In: Textbook of Gynaecological Oncology. 3rd ed. Gunes Publishing: Ankara; 2016.
Wang Y, Gao S, Wang Y, Chen F, Deng H, Lu Y. The efficiency of type-specific high-risk human papillomavirus models in the triage of women with atypical squamous cells of undetermined significance. Cancer Manag Res. 2020;12:5265–75.
Beyazit F, Silan F, Gencer M, Aydin B, Paksoy B, Unsal MA, et al. The prevalence of human papillomavirus (HPV) genotypes detected by PCR in women with normal and abnormal cervico-vaginal cytology. Ginekol Pol. 2018;89(2):62–7.
Ortashi O, Abdalla D. Colposcopic and histological outcome of atypical squamous cells of undetermined significance and atypical squamous cell of undetermined significance cannot exclude high-grade in women screened for cervical cancer. Asian Pac J Cancer Prev. 2019;20(9):2579–82.
Yarandi F, Izadi Mood N, Mirashrafi F, Eftekhar Z. Colposcopic and histologic findings in women with a cytologic diagnosis of atypical squamous cells of undetermined significance. Aust N Z J Obstet Gynaecol. 2004;44(6):514–6.
Acknowledgements
The authors thank the medical records unit of Cipto Mangunkusumo Hospital, Jakarta, Indonesia.
Author information
Authors and Affiliations
Contributions
JI and LR took part in concept and design of study. LTAS, RH and KA performed the analysis, interpretation of data and wrote the manuscript. JI revised the paper and had primary responsibility for the final content. All authors agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest in this study.
Informed consent
Informed consent was not sought for the present study as this was a retrospective study. Only clinically relevant information was extracted, and patients’ privacy was protected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Indarti, J., Rachmadi, L., Sutrisna, L.T.A. et al. The Most Common Type of HPV and Colposcopic Findings in Women with Ascus. Indian J Gynecol Oncolog 20, 42 (2022). https://doi.org/10.1007/s40944-022-00641-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-022-00641-0