Abstract
Objective
The aim of this study is to examine service utilization disparities among Black youth participating in Linking Individuals Needing Care (LINC), a 90-day research-informed suicide care coordination intervention.
Methods
An open trial pilot was conducted to examine the effectiveness of LINC in increasing access to and engagement in mental health and non-mental health services among suicidal youth (N = 587). Other variables of interest included service use facilitators and service use barriers. Generalized linear mixed models with binomial distribution and logit link were performed to ascertain if service use facilitators and barriers were associated with service utilization and if disparities in service use and engagement existed between Black and White suicidal youth through a comparative analysis.
Results
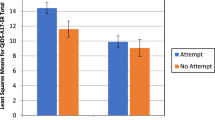
Service utilization differences were found between Black and White youth. While Black and White youth were both likely to engage in individual therapy (OR = 1.398, p < .001) and non-mental health services (OR = 1.289, p < .001), utilization rates for mental health and medication management services were lower for Black (55.1% to 60.6%) youth compared to White (66.0% to 71.0%) youth. Specifically, Black youth were significantly less likely than Whites to receive medication management (OR = .466, p = .002). Systemic barriers such long waitlists for care (OR = 1.860, p = .039) and poor relationship with providers (OR = 7.680, p = .028) increased odds of engagement in non-mental health services. Clinical disorders and engagement in suicide-related behaviors increased the likelihood of obtaining care from both medication management and non-mental health services.
Conclusion
Care coordination services for suicidal youth can increase access and engagement in mental health and non-mental health services. Culturally adapted models attending to cultural and social assets of Black families are needed to reduce disparities and suicide risk among Black youth.
Similar content being viewed by others
References
The Congressional Black Caucus, Emergency Taskforce on Black Youth Suicide and Mental Health. Ring the alarm: the crisis of black youth suicide in America; 2019. https://theactionalliance.org. Accessed 2 July 2022
Centers for Disease Control and Prevention, National Center for Health Statistics. National vital statistics system, mortality 1999–2020 on CDC Wonder online database. Accessed 5 July 2022. http://wonder.cdc.gov/ucd-icd10.html
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. WISQARS — Web-based Injury Statistics Query and Reporting System. Accessed 10 July 2022. https://wisqars.cdc.gov/data/explore-data/home
Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatr. 2018;172(7):697–9. https://doi.org/10.1001/jamapediatrics.2018.0399.
Bridge JA, Asti L, Horowitz LM, et al. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatr. 2015;169(7):673. https://doi.org/10.1001/jamapediatrics.2015.0465.
Lindsey MA, Sheftall AH, **ao Y, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. 2019;144(5). https://doi.org/10.1542/peds.2019-1187
**ao Y, Cerel J, Mann JJ. Temporal trends in suicidal ideation and attempts among US adolescents by sex and race/ethnicity, 1991–2019. JAMA Netw Open. 2021;4(6):e2113513. https://doi.org/10.1001/jamanetworkopen.2021.13513.
Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS): 2019 YRBS results. Accessed 5 July 2022. http://www.cdc.gov/healthyyouth/data/yrbs/features/index.htm
Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141(6). https://doi.org/10.1542/peds.2017-2426.
Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. 2011;50(2):160–70. https://doi.org/10.1016/j.jaac.2010.11.004.
Kodjo C, Auinger P. Predictors for emotionally distressed adolescents to receive mental health care. J Adolesc Health. 2004;35(5):368–73. https://doi.org/10.1016/S1054-139X(04)00061-8.
Lu W. Adolescent depression: National trends, risk factors, and healthcare disparities. Am J Health Behav. 2019;43(1):181–94. https://doi.org/10.5993/AJHB.43.1.15.
Marrast L, Himmelstein DU, Woolhandler S. Racial and ethnic disparities in mental health care for children and young adults: A national study. Int J Health Serv. 2016;46(4):810–24. https://doi.org/10.1177/0020731416662736.
Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4):e20182192. https://doi.org/10.1542/peds.2018-2192.
Nestor BA, Cheek SM, Liu RT. Ethnic and racial differences in mental health service utilization for suicidal ideation and behavior in a nationally representative sample of adolescents. J Affect Disord. 2016;202:197–202. https://doi.org/10.1016/j.jad.2016.05.021.
Abrams AH, Badolato GM, Boyle MD, McCarter R, Goyal MK. Racial and ethnic disparities in pediatric mental health-related emergency department visits. Pediatr Emerg Care. 2022;38(1):e214–8. https://doi.org/10.1097/PEC.0000000000002221.
Gryglewicz K, Peterson A, Nam E, Vance MM, Borntrager L, Karver MS. Caring transitions – A care coordination intervention to reduce suicide risk among youth discharged from inpatient psychiatric hospitalization. Crisis. 2021. https://doi.org/10.1027/0227-5910/a000795.
Fontanella CA, Warner LA, Steelesmith DL, Brock G, Bridge JA, Campo JV. association of timely outpatient mental health services for youths after psychiatric hospitalization with risk of death by suicide. JAMA Netw Open. 2020;3(8):e2012887. https://doi.org/10.1001/jamanetworkopen.2020.12887.
Berry S, Soltau E, Richmond NE, Kieltyka RL, Tran T, Williams A. Care coordination in a medical home in post-Katrina New Orleans: lessons learned. Matern Child Health J. 2011;15(6):782–93. https://doi.org/10.1007/s10995-010-0641-4.
Cosgrove JA, Lee BR, Unick GJ. A longitudinal evaluation of wraparound’s impact on youth mental health service use. J Emot Behav Disord. 2020;28(3):156–66. https://doi.org/10.1177/1063426619842568.
Blizzard AM, Glos LJ, Stephan SH, Medoff D, Slade EP. Impacts of a Medicaid wraparound model demonstration program on youth specialty mental health services use. J Behav Health Serv Res. 2017;44(3):373–85. https://doi.org/10.1007/s11414-016-9520-0.
Schultz EM, McDonald KM. What is care coordination? Int J Care Coord. 2014;17(1–2):5–24. https://doi.org/10.1177/2053435414540615.
Council on Children with Disabilities. Care coordination in the medical home: Integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116(5):1238–44. https://doi.org/10.1542/peds.2005-2070.
Antonelli R, McAllister J, Popp J. Making care coordination a critical component of the pediatric health system: a multidisciplinary framework. 2009. https://www.commonwealthfund.org/publications/fund-reports/2009/may/making-care-coordination-criticalcomponent-pediatric-health. Accessed 15 Jul 2022.
Björkelund C, Svenningsson I, Hange D, et al. Clinical effectiveness of care managers in collaborative care for patients with depression in Swedish primary health care: a pragmatic cluster randomized controlled trial. BMC Fam Pract. 2018;19(1):28. https://doi.org/10.1186/s12875-018-0711-z.
Stanard RP. The effect of training in a strengths model of case management on client outcomes in a community mental health center. Community Ment Health J. 1999;35(2):169–79. https://doi.org/10.1023/A:1018724831815.
Rapp C, Wintersteen R. The strengths model of case management: results from twelve demonstrations. Psychosoc Rehabil J. 1989;13(1):23–32.
Vance M. An examination of the Florida Linking Individuals Needing Care Coordination program for racial and ethnic minority females. University of Central Florida; 2019. http://purl.fcla.edu/fcla/etd/CFE0007548
Turchi RM, Berhane Z, Bethell C, Pomponio A, Antonelli R, Minkovitz CS. Care coordination for CSHCN: associations with family-provider relations and family/child outcomes. Pediatrics. 2009;124(Supplement_4):S428-S434. https://doi.org/10.1542/peds.2009-1255O
Olson JR, Benjamin PH, Azman AA, et al. Systematic review and meta-analysis: effectiveness of wraparound care coordination for children and adolescents. J Am Acad Child Adolesc Psychiatry. 2021;60(11):1353–66. https://doi.org/10.1016/j.jaac.2021.02.022.
Unützer J, Harbin H, Schoenbaum M, Druss B. The Collaborative Care Model: an approach for integrating physical and mental health care in Medicaid health homes; 2013:1–13. https://www.chcs.org/media/HH_IRC_Collaborative_Care_Model__052113_2.pdf
Sobolewski B, Richey L, Kowatch RA, Grupp-Phelan J. Mental health follow-up among adolescents with suicidal behaviors after emergency department discharge. Arch Suicide Res. 2013;17(4):323–34. https://doi.org/10.1080/13811118.2013.801807.
Adrian M, DeCou C, Gold LS. Medically treated self-injury among children and adolescents: repeated attempts and service use over 1 year. Psychiatr Serv. 2020;71(5):447–55. https://doi.org/10.1176/appi.ps.201900152.
Hogan MF. Better suicide screening and prevention are possible. JAMA Psychiat. 2016;73(11):1111. https://doi.org/10.1001/jamapsychiatry.2016.2411.
Hom MA, Stanley IH, Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: a review of the literature. Clin Psychol Rev. 2015;40:28–39. https://doi.org/10.1016/j.cpr.2015.05.006.
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust E-J Adv Ment Health. 2005;4(3):218–51. https://doi.org/10.5172/jamh.4.3.218.
Salzer MS, Nixon CT, Schut LJA, Karver MS, Bickman L. Validating quality indicators: quality as relationship between structure, process, and outcome. Eval Rev. 1997;21(3):292–309. https://doi.org/10.1177/0193841X9702100302.
Prochaska JO, Velicer WF. The Transtheoretical Model of Health Behavior Change. Am J Health Promot. 1997;12(1):38–48. https://doi.org/10.4278/0890-1171-12.1.38.
Kominski GF, ed. Changing the U.S. health care system: key issues in health services policy and management. 4th ed. Jossey-Bass. 2014.
Rollnick S, Miller WR. Motivational interviewing: hel** people change. New York: Guilford Press; 2013.
Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum Press; 1985.
Karver MS, Handelsman JB, Fields S, Bickman L. A theoretical model of common process factors in youth and family therapy. Ment Health Serv Res. 2005;7(1):35–51. https://doi.org/10.1007/s11020-005-1964-4.
Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the services assessment for children and adolescents. Psychiatr Serv. 2001;52(8):1088–94. https://doi.org/10.1176/appi.ps.52.8.1088.
Kazdin AE, Holland L, Crowley M, Breton S. Barriers to treatment participation scale: evaluation and validation in the context of child outpatient treatment. J Child Psychol Psychiatry. 1997;38(8):1051–62. https://doi.org/10.1111/j.1469-7610.1997.tb01621.x.
Osman A, Downs WR, Kopper BA, et al. The reasons for living inventory for adolescents (RFL-A): development and psychometric properties. J Clin Psychol. 1998;54(8):1063–78. https://doi.org/10.1002/(SICI)1097-4679(199812)54:8%3c1063:AID-JCLP6%3e3.0.CO;2-Z.
O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. https://doi.org/10.1016/S2215-0366(14)70222-6.
Fowler JC. Suicide risk assessment in clinical practice: pragmatic guidelines for imperfect assessments. Psychotherapy. 2012;49(1):81–90. https://doi.org/10.1037/a0026148.
Rudd MD, Joiner T. The assessment, management, and treatment of suicidality: toward clinically informed and balanced standards of care. Clin Psychol Sci Pract. 1998;5(2):135–50. https://doi.org/10.1111/j.1468-2850.1998.tb00140.x.
Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. https://doi.org/10.1097/01.CHI.0000046821.95464.CF.
Planey AM, Smith SM, Moore S, Walker TD. Barriers and facilitators to mental health help-seeking among African American youth and their families: a systematic review study. Child Youth Serv Rev. 2019;101:190–200. https://doi.org/10.1016/j.childyouth.2019.04.001.
Kim HY. Statistical notes for clinical researchers: chi-squared test and fisher’s exact test. Restor Dent Endod. 2017;42(2):152–5. https://doi.org/10.5395/rde.2017.42.2.152.
IBM SPSS Statistics for Windows. https://www.ibm.com/analytics/spss-statistics-software.
Barksdale CL, Azur M, Leaf PJ. Differences in mental health service sector utilization among African American and Caucasian youth entering systems of care programs. J Behav Health Serv Res. 2010;37(3):363–73. https://doi.org/10.1007/s11414-009-9166-2.
Angold A, Erkanli A, Farmer EMZ, et al. Psychiatric disorder, impairment, and service Use in rural African American and White youth. Arch Gen Psychiatry. 2002;59(10):893. https://doi.org/10.1001/archpsyc.59.10.893.
Molock SD, Barksdale C, Matlin S, Puri R, Cammack N, Spann M. Qualitative study of suicidality and help-seeking behaviors in African American adolescents. Am J Community Psychol. 2007;40(1–2):52–63. https://doi.org/10.1007/s10464-007-9122-3.
Murry VM, Heflinger CA, Suiter SV, Brody GH. Examining perceptions about mental health care and help-seeking among rural African American families of adolescents. J Youth Adolesc. 2011;40(9):1118–31. https://doi.org/10.1007/s10964-010-9627-1.
Abram KM, Paskar LD, Washburn JJ, Teplin LA. Perceived barriers to mental health services among youths in detention. J Am Acad Child Adolesc Psychiatry. 2008;47(3):301–8. https://doi.org/10.1097/CHI.0b013e318160b3bb.
Lindsey MA, Chambers K, Pohle C, Beall P, Lucksted A. Understanding the behavioral determinants of mental health service use by urban, under-resourced black youth: adolescent and caregiver perspectives. J Child Fam Stud. 2013;22(1):107–21. https://doi.org/10.1007/s10826-012-9668-z.
Baglivio MT, Wolff KT, Piquero AR, Greenwald MA, Epps N. Racial/ethnic disproportionality in psychiatric diagnoses and treatment in a sample of serious juvenile offenders. J Youth Adolesc. 2017;46(7):1424–51. https://doi.org/10.1007/s10964-016-0573-4.
AAKOMA Project Adult Advisory Board, Breland-Noble AM, Bell CC, Burriss A. “Mama just won’t accept this”: adult perspectives on engaging depressed African American teens in clinical research and treatment. J Clin Psychol Med Settings. 2011;18(3):225–34. https://doi.org/10.1007/s10880-011-9235-6.
Lindsey MA, Korr WS, Broitman M, Bone L, Green A, Leaf PJ. Help-seeking behaviors and depression among African American adolescent boys. Soc Work. 2006;51(1):49–58. https://doi.org/10.1093/sw/51.1.49.
Samuel IA. Utilization of mental health services among African-American male adolescents released from juvenile detention: examining reasons for within-group disparities in help-seeking behaviors. Child Adolesc Soc Work J. 2015;32(1):33–43. https://doi.org/10.1007/s10560-014-0357-1.
Vázquez AL, Villodas MT. Racial/ethnic differences in caregivers’ perceptions of the need for and utilization of adolescent psychological counseling and support services. Cultur Divers Ethnic Minor Psychol. 2019;25(3):323–30. https://doi.org/10.1037/cdp0000255.
Mishra SI, Lucksted A, Gioia D, Barnet B, Baquet CR. Needs and preferences for receiving mental health information in an African American Focus Group sample. Community Ment Health J. 2009;45(2):117–26. https://doi.org/10.1007/s10597-008-9157-4.
Cavell TA, Spencer R, McQuillin SD. Back to the future: mentoring as means and end in promoting child mental health. J Clin Child Adolesc Psychol. 2021;50(2):281–99. https://doi.org/10.1080/15374416.202.1875327.
Haan AM, Boon AE, Jong JTVM, Geluk CAML, Vermeiren RRJM. Therapeutic relationship and dropout in youth mental health care with ethnic minority children and adolescents. Clin Psychol. 2014;18(1):1–9. https://doi.org/10.1111/cp.12030.
Hays K. Black churches’ capacity to respond to the mental health needs of African Americans. Soc Work Christ. 2015;42(3):296–312.
Bruckner TA, Singh P, Yoon J, Chakravarthy B, Snowden LR. African American/white disparities in psychiatric emergencies among youth following rapid expansion of Federally Qualified Health Centers. Health Serv Res. 2020;55(1):26–34. https://doi.org/10.1111/1475-6773.13237.
Robinson WL, Case MH, Whipple CR, et al. Culturally grounded stress reduction and suicide prevention for African American adolescents. Pract Innov. 2016;1(2):117–28. https://doi.org/10.1037/pri0000020.
Amutah-Onukagha N, Mahadevan M, Opara I, Rodriguez M, Trusdell M, Kelly J. Project THANKS: examining HIV/AIDS-related barriers and facilitators to care in African American women: a community perspective. AIDS Patient Care STDs. 2018;32(4):119–28. https://doi.org/10.1089/apc.2017.0215.
Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. 2010;19(4):759–74. https://doi.org/10.1016/j.chc.2010.07.001.
Lanier Y, Sommers MS, Fletcher J, Sutton MY, Roberts DD. Examining racial discrimination frequency, racial discrimination stress, and psychological well-being among black early adolescents. J Black Psychol. 2017;43(3):219–29. https://doi.org/10.1177/0095798416638189.
Assari S, Moghani Lankarani M, Caldwell CH. Discrimination increases suicidal ideation in black adolescents regardless of ethnicity and gender. Behav Sci. 2017;7(4):75-. https://doi.org/10.3390/bs7040075
Acknowledgements
We would also like to thank Marissa McNeil (a graduate student) for her assistance with this manuscript.
Funding
This work was supported by the Substance Abuse and Mental Health Services Administration (SAMHSA) through the Garrett Lee Smith Memorial Act, grant number 1 U79 SM061748.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Kim Gryglewicz and Eunji Nam. The first draft of the manuscript was written by Michelle Vance and Kim Gryglewicz, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study protocols were determined to be NHSR (“not human subjects research”) by the university institutional review board.
Disclaimer
The views expressed in this paper do not necessarily reflect the views, opinions, or policies of SAMHSA or the US Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the US Government.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vance, M.M., Gryglewicz, K., Nam, E. et al. Exploring Service Use Disparities among Suicidal Black Youth in a Suicide Prevention Care Coordination Intervention. J. Racial and Ethnic Health Disparities 10, 2231–2243 (2023). https://doi.org/10.1007/s40615-022-01402-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01402-7