Abstract
Introduction
The increase in the pulsatile component of left ventricle afterload is suspected to cause a mismatch between the left ventricle (LV) and the vascular tree.
Aim
To demonstrate that ventricular-arterial uncoupling is frequently present in the development of LV hypertrophy (H) and diastolic dysfunction (DD) in hypertension (HBP).
Methods
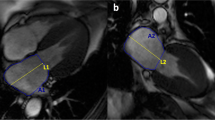
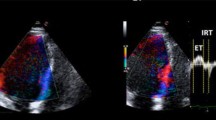
Observational study, HBP patients with ejection fraction > 54%. Conventional 2D echocardiography and tissue Doppler performed following imaging guidelines. LV end systolic elastance (Ees), the effective arterial elastance (Ea), and ventricular-arterial coupling (VAC) measured by Chen single beat method.
Results
288 patients, mean age 56.3 ± 12.5 years and 168 patients (58.3%) males. Mean LV mass index was 87.2 ± 20.4 grs/m2 and frequency of LVH 20.1% (58 patients). The mean VAC was 0.54 ± 9.23. LV Stroke volume, stroke work and systolic stress were 46.2 ± 10.3 cc/m2, 91.4 ± 22.2 g-min/m2, and 57 ± 14.6 dynes/cm2 in quartile 1, and 33.5 ± 6.6 cc/m2, 65.5 ± 15.2 g-min/m2, and 77.8 ± 17.1 dynes/cm2, in quartile 4, respectively (p < 0.001). Peripheral resistance index was 3349 ± 1072 and 4410 ± 1143 dynes*s/cm-5/m2 quartiles 1 vs. 4 (p < 0.005). The frequency of LVH was 31.9% in quartile 1 and 11.3% in quartile 4 (p < 0.005) and LVH or DD was 37.5% and 12.7%, respectively (p < 0.001).
Conclusions
Stroke volume and stroke work were significantly increased while systolic stress and peripheral resistance index were significantly reduced in patients with worst VAC. Ventricular-arterial uncoupling is mostly caused by an increase in Ees rather than by an elevation of Ea. LVH or DD are more frequent in the worst cases of ventricular-arterial uncoupling.
Similar content being viewed by others
References
Chirinos JA, Segers P, Gillebert TC, Gupta AK, De Buyzere ML, De Bacquer D, St John-Sutton M, Rietzschel ER, on behalf of the Asklepios Investigators. Arterial properties as determinants of time-varying myocardial stress in humans. Hypertension 2012;60:64–70.
Chirinos JA, Segers P, Rietzschel ER, De Buyzere ML, Raja MW, Claessens T, De Bacquer D, St John Sutton M, Gillebert TC; Asklepios Investigators. Early and late systolic wall stress differentially relate to myocardial contraction and relaxation in middle-aged adults: the Asklepios study. Hypertension 2013;61:296–303.
Piskorz D, Bongarzoni L, Citta L, Citta N, Citta P, Keller L, Mata L, Tommasi A, et al. Functional organ damage in cardiovascular low risk patients with high central aortic pressure. High Blood Press Cardiovasc Prev. 2015;22:281–7.
Tissera G, Piskorz D, Citta L, Citta N, Citta P, Keller L, Bongarzoni L, Mata L, Tommasi A. Morphologic and functional heart abnormalities associated to high modified Tei index in hypertensive patients. High Blood Press Cardiovasc Prev. 2016;23:373–80.
De Tombe PP, Jones S, Burkhoff D, Hunter WC, Kass DA. Ventricular stroke work and efficiency both remain nearly optimal despite altered vascular loading. Am J Physiol. 1993;264:1817–24.
Guarracino F, Baldassarri R, Pinsky MR. Ventriculo-arterial decoupling in acutely altered hemodynamic states. Crit Care. 2013;17:213.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti† A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I. 2018 ESH/ESC Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2018;36:1953–2041.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W; American Society of Echocardiography's Nomenclature and Standards Committee; Task Force on Chamber Quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr 2006;7:79–108.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Alexandru Popescu B, Waggoner AD. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Sunagawa K, Maughan WL, Burkhoff D, Sagawa K. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol. 1983;245:H773–80.
Chen CH, Fetics B, Nevo E, Rochitte CE, Chiou KR, Ding PA, Kawaguchi M, Kass DA. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J Am Coll Cardiol. 2001;38:2028–34.
Sagawa K, Suga H, Shoukas AA, Bakalar KM. End-systolic pressure volume ratio: a new index of ventricular contractility. Am J Cardiol. 1977;40:748–53.
Kameyama T, Asanoi H, Ishizaka S, Yamanishi K, Fujita M, Sasayama S. Energy conversion efficiency in human left ventricle. Circulation. 1992;85:988–96.
Osranek M, Eisenach JH, Khandheria BK, Chandrasekaran K, Seward JB, Belohlavek M. Arterioventricular coupling and ventricular efficiency after antihypertensive therapy. A noninvasive prospective study. Hypertension. 2008;51:275–81.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled systolic-ventricular and vascular stiffening with age. Implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol. 1998;32:1221–7.
Rosa-Garrido M, Chapski DJ, Schmitt AD, Kimball TH, Karbassi E, Monte E, Balderas E, Pellegrini M, Shih TT, Soehalim E, Liem D, ** P, Galjart NJ, Ren S, Wang Y, Ren B, Vondriska TM. High-resolution map** of chromatin conformation in cardiac myocytes reveals structural remodeling of the epigenome in heart failure. Circulation. 2017;136:1613–25.
Li Z, Bing OHL, Long X, Robinson KG, Lakatta EG. Increased cardiomyocite apoptosis during the transition to heart failure in the spontaneously hypertensive rat. Am J Physiol. 1997;272:2313H-2319H.
Diez J, Fortuño MA, Ravassa S. Apoptosis in hypertensive heart disease. Curr Opin Cardiol. 1998;13:317–25.
Dzau VJ. Theodore Cooper Lecture: tissue angiotensin and pathobiology of vascular disease: a unifying hypothesis. Hypertension. 2001;37:1047–52.
Mordi IR, Singh S, Rudd A, Srinivasan J, Frenneaux M, Tzemos N, Dawson DK. Comprehensive echocardiographic and cardiac magnetic resonance evaluation differentiates among heart failure with preserved ejection fraction patients, hypertensive patients, and healthy control subjects. JACC Cardiovasc Imaging. 2018;11:577–85.
Kane J, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC Jr, Jacobsen SJ, Rodeheffer RJ. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856–63.
Vasan RS, Xanthakis V, Lyass A, Andersson C, Tsao C, Cheng S, Aragam J, Benjamin EJ, Larson MG. Epidemiology of left ventricular systolic dysfunction and heart failure in the framingham study: an echocardiographic study over 3 decades. JACC Cardivasc Imaging. 2018;11:1–11.
Piskorz D, Bongarzoni L, Citta L, Citta N, Citta P, Keller L, Tommasi A. Association of systolic dysfunction with left ventricular hypertrophy and diastolic dysfunction in hypertensive patients. Rev Fac Cien Med Univ Nac Cordoba. 2014;71:158–64.
D’Andrea A, Ilardi F, D’Ascenzi F, Bandera F, Benfari G, Esposito R, Malagoli A, Mandoli GE, Santoro C, Russo V, D'Alto M, Cameli M; On behalf of Working Group of Echocardiography of the Italian Society of Cardiology (SIC). Impaired myocardial work efficiency in heart failure with preserved ejection fraction. Eur Heart J Cardiovasc Imaging 2021;22:1312–20.
Tadic M, Cuspidi C, Saeed S, Lazic JS, Vukomanovic V, Grassi G, Sala C, Celic V. The influence of left ventricular geometry on myocardial work in essential hypertension. J Human Hypertens. 2021. https://doi.org/10.1038/s41371-021-00543-2.
Burkhoff D. Pressure-volume loops in clinical research. J Am Col Cardiol. 2013;62:1173–6.
Devereux RB, Bella JN, Palmieri V, Oberman A, Kitzman DW, Hopkins PN, Rao DC, Morgan D, Paranicas M, Fishman D, Arnett DK, Hypertension Genetic Epidemiology Network Study Group. Left ventricular systolic dysfunction in a biracial sample of hypertensive adults: the hypertension genetic epidemiology network (HyperGEN) Study. Hypertension 2001;38:417–25.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Rights and permissions
About this article
Cite this article
Piskorz, D., Keller, L., Citta, L. et al. Ventricular-Arterial Uncoupling and Hypertension Mediated Diastolic Dysfunction. High Blood Press Cardiovasc Prev 29, 361–366 (2022). https://doi.org/10.1007/s40292-022-00521-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00521-w