Abstract
Purpose
The American Heart Association recommended sodium-glucose cotransporter-2 inhibitors (SGLT2i) for the management of heart failure with preserved ejection fraction (HFpEF). However, little is known about their real-world in-class comparative safety in patients with HFpEF. We aimed to assess the comparative safety of SGLT2i in the risk of urinary tract infection (UTI) or genital infection separately or as a composite outcome among patients with HFpEF.
Methods
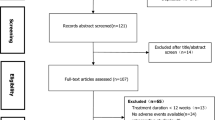
This cohort study using MarketScan® Commercial and Medicare supplemental databases (2012–2020) included patients aged ≥ 18 years with a diagnosis of HFpEF who initiated SGLT2i therapy. Three pairwise comparison groups were established: cohort 1, dapagliflozin versus canagliflozin; cohort 2, empagliflozin versus canagliflozin; and cohort 3, dapagliflozin versus empagliflozin. After stabilized inverse probability treatment weighting, Cox proportional hazards regression was used to compare the risk of UTI or genital infection separately or as a composite outcome in each cohort.
Results
The risk of the composite outcome did not significantly differ between canagliflozin and dapagliflozin (adjusted hazard ratio [aHR] 0.64; 95% confidence interval [CI] 0.36–1.14) or between empagliflozin and canagliflozin (aHR 1.25; 95% CI 0.77–2.05). Similarly, there was no evidence of difference between dapagliflozin and empagliflozin in this risk (aHR 0.76; 95% CI 0.48–1.21). The results of analyses separately assessing UTI or genital infection were similar.
Conclusions
There was no significant difference in the risk of UTI or genital infection among patients with HFpEF who initiated canagliflozin, dapagliflozin, or empagliflozin.
Plain Language Summary
Sodium-glucose cotransporter-2 inhibitors (SGLT2i) are used for the management of heart failure with preserved ejection fraction (HFpEF). It is important to assess their comparative risk of urinary tract infection (UTI) or genital infection among patients with HFpEF. We compared patients with HFpEF using SGLT2i in three pairwise groups: cohort 1, dapagliflozin versus canagliflozin; cohort 2, empagliflozin versus canagliflozin; and cohort 3, dapagliflozin versus empagliflozin. We found that there was no significant difference in the risk of genitourinary infections including UTI or genital infections among dapagliflozin, empagliflozin, and canagliflozin.
Similar content being viewed by others
References
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61. https://doi.org/10.1056/NEJMoa2107038.
Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022. https://doi.org/10.1056/NEJMoa2206286.
Heidenreich PA, Bozkurt B, Aguilar D, et al. AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022. https://doi.org/10.1161/CIR.0000000000001063.
JARDIANCE® (empagliflozin) tablets, for oral use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/204629s026lbl.pdf. Accessed 15 Sep 2023
FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. https://www.fda.gov/drugs/drug-safety-and-availability/fda-revises-labels-sglt2-inhibitors-diabetes-include-warnings-about-too-much-acid-blood-and-serious#:~:text=FDA Accessed 14 Sep 2023.
Qiu R, Balis D, **e J, Davies MJ, Desai M, Meininger G. Longer-term safety and tolerability of canagliflozin in patients with type 2 diabetes: a pooled analysis. Curr Med Res Opin. 2017;33(3):553–62. https://doi.org/10.1080/03007995.2016.1271780.
Storgaard H, Gluud LL, Bennett C, et al. Benefits and harms of sodium-glucose co-transporter 2 inhibitors in patients with type 2 diabetes: a systematic review and meta-analysis. PLoS ONE. 2016;11(11): e0166125.
Liu J, Li L, Li S, et al. Effects of SGLT2 inhibitors on UTIs and genital infections in type 2 diabetes mellitus: a systematic review and meta-analysis. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-02733-w.
Jabbour S, Seufert J, Scheen A, Bailey CJ, Karup C, Langkilde AM. Dapagliflozin in patients with type 2 diabetes mellitus: a pooled analysis of safety data from phase IIb/III clinical trials. Diabetes Obes Metab. 2018;20(3):620–8. https://doi.org/10.1111/dom.13124.
Caparrotta TM, Greenhalgh AM, Osinski K, et al. Sodium-glucose co-transporter 2 inhibitors (SGLT2i) EXPOSURE AND OUTCOMES IN TYPE 2 DIABETES: A SYSTEMATIC REVIEW OF POPULATION-BASED OBSERVATIONAL STUDIES. Diabetes Ther. 2021;12(4):991–1028. https://doi.org/10.1007/s13300-021-01004-2.
McGuire DK, Shih WJ, Cosentino F, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiology. 2021;6(2):148–58. https://doi.org/10.1001/jamacardio.2020.4511.
Younes AM, Salem M, Maraey A, et al. Safety outcomes of SGLT2i in the heart failure trials: a systematic review and Meta-analysis. Int J Cardiol. 2022;366:51–6. https://doi.org/10.1016/j.ijcard.2022.06.059.
Cao Y, Li P, Li Y, Han Y. Sodium-glucose cotransporter-2 inhibitors in heart failure: an updated meta-analysis. ESC Heart Fail. 2022;9(3):1942–53. https://doi.org/10.1002/ehf2.13905.
Cohen SS, Roger VL, Weston SA, et al. Evaluation of claims-based computable phenotypes to identify heart failure patients with preserved ejection fraction. Pharmacol Res Perspect. 2020;8(6):1–8. https://doi.org/10.1002/prp2.676.
Sarayani A, Wang X, Thai TN, Albogami Y, Jeon N, Winterstein AG. Impact of the transition from ICD-9-CM to ICD-10-CM on the identification of pregnancy episodes in US Health Insurance Claims Data. Clin Epidemiol. 2020;12:1129–38. https://doi.org/10.2147/CLEP.S269400.
Germanos G, Light P, Zoorob R, et al. Validating use of electronic health data to identify patients with urinary tract infections in outpatient settings. Antibiotics (Basel, Switzerland). 2020;9(9):536. https://doi.org/10.3390/antibiotics9090536.
Dave CV, Schneeweiss S, Patorno E. Comparative risk of genital infections associated with sodium-glucose co-transporter-2 inhibitors. Diabetes Obes Metab. 2019;21(2):434–8. https://doi.org/10.1111/dom.13531.
Gong FF, Jelinek MV, Castro JM, et al. Risk factors for incident heart failure with preserved or reduced ejection fraction, and valvular heart failure, in a community-based cohort. Open heart. 2018;5(2):e000782–e000782. https://doi.org/10.1136/openhrt-2018-000782.
Dave CV, Schneeweiss S, Kim D, Fralick M, Tong A, Patorno E. Sodium-glucose cotransporter-2 inhibitors and the risk for severe urinary tract infections: a population-based cohort study. Ann Intern Med. 2019;171(4):248–56. https://doi.org/10.7326/M18-3136.
Caro MKC, Cunanan EC, Kho SA. Incidence and factors associated with genitourinary infections among Type 2 diabetes patients on SGLT2 Inhibitors: A single retrospective cohort study. Diabetes Epidemiol Manag. 2022;7: 100082. https://doi.org/10.1016/j.deman.2022.100082.
Riaz M, Smith SM, Dietrich EA, Winchester DE, Guo J, Park H. Comparative effectiveness of sodium-glucose cotransporter-2 inhibitors among patients with heart failure with preserved ejection fraction. Pharmacotherapy. 2023;43(10):1024–1031. https://doi.org/10.1002/phar.2853.
Brookhart MA, Wyss R, Layton JB, Stürmer T. Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes. 2013;6(5):604–11. https://doi.org/10.1161/CIRCOUTCOMES.113.000359.
Uitrakul S, Aksonnam K, Srivichai P, Wicheannarat S, Incomenoy S. The incidence and risk factors of urinary tract infection in patients with type 2 diabetes mellitus using SGLT2 inhibitors: a real-world observational study. Medicines. 2022. https://doi.org/10.3390/medicines9120059.
Lopaschuk GD, Verma S. Mechanisms of cardiovascular benefits of sodium glucose co-transporter 2 (SGLT2) inhibitors: a State-of-the-Art Review. JACC Basic Transl Sci. 2020;5(6):632–44. https://doi.org/10.1016/j.jacbts.2020.02.004.
Geerlings S, Fonseca V, Castro-Diaz D, List J, Parikh S. Genital and urinary tract infections in diabetes: Impact of pharmacologically-induced glucosuria. Diabetes Res Clin Pract. 2014;103(3):373–81. https://doi.org/10.1016/j.diabres.2013.12.052.
Spertus JA, Birmingham MC, Nassif M, et al. The SGLT2 inhibitor canagliflozin in heart failure: the CHIEF-HF remote, patient-centered randomized trial. Nat Med. 2022;28(4):809–13. https://doi.org/10.1038/s41591-022-01703-8.
Male circumcision. Pediatrics. 2012;130(3):e756-85. https://doi.org/10.1542/peds.2012-1990.
Rayens E, Rayens MNK. Demographic and socioeconomic factors associated with fungal infection risk, United States, 2019. Emerg Infect Dis. 2022;28(10):1955–69.
Funding
No funding was received to conduct this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Statement
This study was approved by the University of Florida Institutional Review Board and used de-identified data from administrative claims databases.
Conflict of Interest
Munaza Riaz, **gchuan Guo, Steven M. Smith, Eric A. Dietrich, David E. Winchester, and Haesuk Park declare that they have no potential conflicts of interest that might be relevant to the contents of this article.
Author Contributions
The study was conceptualized by MR. All the authors designed the methodology of the study. MR analyzed the data and drafted the first version of the manuscript. All authors reviewed the manuscript and read and approved the final version.
Data Availability Statement
This study utilized MarketScan® data under a licensed agreement, which restricts the authors from sharing the data. Individuals seeking access to the data should contact the provider directly.
Code Availability
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riaz, M., Guo, J., Smith, S.M. et al. Comparative Genitourinary Safety of In-class Sodium-Glucose Cotransporter-2 Inhibitors among Patients with Heart Failure with Preserved Ejection Fraction: A Cohort Study. Am J Cardiovasc Drugs 24, 455–464 (2024). https://doi.org/10.1007/s40256-024-00648-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-024-00648-2