Abstract
Aims/Introduction
An early-morning elevation of blood glucose levels known as the dawn phenomenon and consequent postbreakfast hyperglycemia occur in some individuals with type 1 diabetes (T1D). Whereas insulin pump therapy can mitigate this phenomenon, some individuals prefer or are limited to alternative treatments. We have now assessed the effectiveness of early-morning administration of rapid-acting insulin for amelioration of the dawn phenomenon in individuals with T1D.
Materials and Methods
Thirteen individuals with T1D who experienced the dawn phenomenon as determined by continuous glucose monitoring (CGM) and who received a small dose of rapid-acting insulin on waking were included in this retrospective study. We evaluated the change in sensor glucose levels during a 2-h period from before to after breakfast consumed at 0700 h. The change in blood glucose levels during additional time intervals, average daily sensor glucose values, CGM indices, and insulin dose were also evaluated.
Results
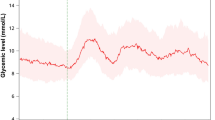
The early-morning administration of 0.5–1 unit of rapid-acting insulin was associated with a significant reduction in 2-h glucose variability between before (0700 h) and after breakfast from a median of 90.7–51.0 mg/dL. The glucose variability from 0300 to 0700 or 0900 h was also significantly decreased, from 67.7 to 29.0 mg/dL and from 172.5 to 78.3 mg/dL, respectively. Average sensor glucose levels throughout the day were significantly reduced (from 192.7 to 156.7 mg/dL), as was the daily total insulin dose.
Conclusion
Early-morning administration of rapid-acting insulin effectively managed the dawn phenomenon and subsequent postbreakfast hyperglycemia in individuals with T1D.


Similar content being viewed by others
Data availability
The data sets generated during the current study are available from the corresponding author upon reasonable request.
References
Schmidt MI, Hadji-Georgopoulos A, Rendell M, et al. The dawn phenomenon, an early morning glucose rise: implications for diabetic intraday blood glucose variation. Diabetes Care. 1981;4:579–85.
Rybicka M, Krysiak R, Okopień B. The dawn phenomenon and the Somogyi effect—two phenomena of morning hyperglycaemia. Endokrynol Pol. 2011;62:276–84.
Porcellati F, Lucidi P, Bolli GB, et al. Thirty years of research on the dawn phenomenon: lessons to optimize blood glucose control in diabetes. Diabetes Care. 2013;36:3860–2.
Monnier L, Colette C, Dunseath GJ, et al. The loss of postprandial glycemic control precedes stepwise deterioration of fasting with worsening diabetes. Diabetes Care. 2007;30:263–9.
Zheng X, Qi Y, Bi L, et al. Effects of exercise on blood glucose and glycemic variability in type 2 diabetic patients with dawn phenomenon. Biomed Res Int. 2020;2020:6408724.
Schiel R. Continuous subcutaneous insulin infusion in patients with diabetes mellitus. Ther Apher Dial. 2003;7:232–7.
Ostrovski I, Lovblom LE, Scarr D, et al. Analysis of prevalence, magnitude and timing of the dawn phenomenon in adults and adolescents with type 1 diabetes: descriptive analysis of 2 insulin pump trials. Can J Diabetes. 2020;44:229–35.
Koivisto VA, Yki-Jarvien H, Helve E, et al. Pathogenesis and prevention of the dawn phenomenon in diabetic patients treated with CSII. Diabetes. 1986;35:78–82.
Beck RW, Tamborlane WV, Bergenstal RM, et al. The T1D exchange clinic registry. Endocrinol Metab. 2012;97:4383–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Scheiner G, Boyer BA. Characteristics of basal insulin requirements by age and gender in Type-1 diabetes patients using insulin pump therapy. Diabetes Res Clin Pract. 2005;69:14–21.
Kuroda A, Kaneto H, Yasuda T, et al. Basal insulin requirement is ~30% of the total daily insulin dose in type 1 diabetic patients who use the insulin pump. Diabetes Care. 2011;34:1089–90.
Nakamura T, Hirota Y, Hashimoto N, et al. Diurnal variation of carbohydrate insulin ratio in adult type 1 diabetic patients treated with continuous subcutaneous insulin infusion. J Diabetes Invest. 2014;5:48–50.
Ceriello A, Esposito K, Piconi L, et al. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes. 2008;57:1349–54.
Author information
Authors and Affiliations
Contributions
Tomofumi Takayoshi and Yushi Hirota conceived the study, analyzed the data, and wrote the manuscript. Akane Yamamoto, Kai Yoshimura, Seiji Nishikage, Mariko Ueda and Wataru Ogawa contributed to discussion and interpretation of the data. Wataru Ogawa contributed to revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Yushi Hirota has received lecture fees from Eli Lilly Japan K.K., Sanofi Aventis, Abbott Japan, Terumo Co., and Sumitomo Pharma Co. Ltd.; research funding from Sumitomo Pharma Co. Ltd., Medtronic Japan Co. Ltd., and Kyowa Kirin Co. Ltd.; and a donation from Abbott Japan. Wataru Ogawa has received lecture fees from Sumitomo Pharma Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., Abbott Japan, and Novo Nordisk Pharma Ltd.; research grants from Noster Inc., Nippon Boehringer Ingelheim Co. Ltd., Eli Lilly Japan K.K., Abbott Diabetes Care UK Ltd., Sumitomo Pharma Co. Ltd., and Tei** Pharma Ltd.; and donations from Kowa Co. Ltd., Novo Nordisk Pharma Ltd., Sumitomo Pharma Co. Ltd., Takeda Pharmaceutical Co. Ltd., and Tei** Pharma Ltd. All remaining authors declare that they have no conflict of interest.
Ethical approval
13 November 2018/ approval no180249.
Informed consent
Informed consent was obtained in the form of an opt-out on the hospital.
Human rights
The ethics committee of Kobe University Graduate School of Medicine.
Animal studies
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Takayoshi, T., Hirota, Y., Yamamoto, A. et al. Impact of early-morning administration of rapid-acting insulin on the increase in blood glucose levels related to the dawn phenomenon in individuals with type 1 diabetes. Diabetol Int (2024). https://doi.org/10.1007/s13340-024-00709-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13340-024-00709-6