Abstract
Background
Diabetic ketoacidosis (DKA) is a critical manifestation in patients with diabetes mellitus. DKA has been conventionally diagnosed by the presence of hyperglycemia (blood glucose levels > 250 mg/dl) and metabolic acidosis (blood gas bicarbonate [HCO3−] < 18 mmol/l and pH in blood gas < 7.30). However, quantitative evaluation of serum ketone bodies has not been established. The current study investigates serum ketone body levels in patients suspected for DKA.
Methods
We have retrospectively evaluated patients with hyperglycemia whose serum ketone body levels at the outpatient clinic and emergency department were measured simultaneously with blood gas analysis during 2011–2019. Clinical backgrounds, severity of diabetes, serum ketone bodies, and blood gas factors were analyzed.
Results
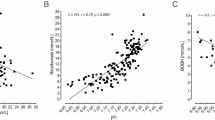
Seventy-two patients were enrolled in the study, after the exclusion of patients who had ketosis due to factors other than diabetes. Serum ketone body levels were negatively correlated with the levels of blood HCO3− and pH. By receiver-operating-characteristic curve analyses, optimal cut-off values for diagnosis of DKA were determined at 6.3 mmol/l of beta-hydroxybutyrate, 1.4 mmol/l of acetoacetate, and 8.0 mmol/l of total ketone body, respectively. Moreover, serum ketone bodies appeared to effectively differentiate between type 1 and type 2 diabetes mellitus. The cut-off values were higher than those in previous reports.
Conclusions
Serum ketone body levels were thought to be useful in the diagnosis of DKA. Further investigations with increased numbers of patients are required to establish the appropriate application of serum ketone bodies in patients with DKA.




Similar content being viewed by others
Data availability statement
The datasets in the manuscript are available from the corresponding authors on reasonable request.
Abbreviations
- AcAc:
-
Acetoacetate
- CPR:
-
C-peptide
- DM:
-
Diabetes mellitus
- DKA:
-
Diabetic ketoacidosis
- GADAb:
-
Glutamic acid decarboxylase autoantibody
- HCO3 − :
-
Bicarbonate
- ICAs:
-
Autoantibodies to islet cells
- IDDM:
-
Insulin-dependent diabetes mellitus
- KPD:
-
Ketosis-prone type 2 diabetes mellitus
- NIDDM:
-
Non-insulin-dependent diabetes mellitus
- ROC:
-
Receiver-operating-characteristic
- TKB:
-
Total ketone body
- T1DM:
-
Type 1 diabetes mellitus
- T2DM:
-
Type 2 diabetes mellitus
- βOHB:
-
Beta-hydroxybutyrate
References
Dhatariya KK, Glaser NS, Codner E, Umpierrez GE. Diabetic ketoacidosis. Nat Rev Dis Primers. 2020;6(1):40. https://doi.org/10.1038/s41572-020-0165-1.
Dhatariya KK. Blood ketones: measurement, interpretation, limitations, and utility in the management of diabetic ketoacidosis. Rev Diabet Stud. 2016;13(4):217–25.
Cotter DG, Schugar RC, Crawford PA. Ketone body metabolism and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2013;304(8):H1060–76.
Féry F, Balasse EO. Ketone body production and disposal in diabetic ketosis: a comparison with fasting ketosis. Diabetes. 1985;34(4):326–32.
Fulop M, Murthy V, Michilli A, Nalamati J, Qian Q, Saitowitz A. Serum β-hydroxybutyrate measurement in patients with uncontrolled diabetes mellitus. Arch Intern Med. 1999;159(4):381–4.
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–43.
Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, et al. ISPAD clinical practice consensus guidelines 2018: diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Diabetes. 2018;19(Suppl 27):155–77.
Sheikh-Ali M, Karon BS, Basu A, Kudva YC, Muller LA, Xu J, et al. Can serum beta-hydroxybutyrate be used to diagnose diabetic ketoacidosis? Diabetes Care. 2008;31(4):643–7.
Arora S, Henderson SO, Long T, Menchine M, et al. Diagnostic accuracy of point-of care testing for diabetic ketoacidosis at emergency-department triage. Diabetes Care. 2011;34(4):852–4.
Harano Y, Kosugi K, Hyosu T, Suzuki M, Hidaka A, Kashiwagi A, et al. Ketone bodies as markers for type 1 (insulin-dependent) diabetes and their value in the monitoring of diabetic control. Diabetologia. 1984;26(5):343–8.
Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese clinical guideline for diabetes 2019. Diabetol Int. 2020;11(3):165–223.
Umpierrez GE. Ketosis-prone type 2 diabetes: time to revise the classification of diabetes. Diabetes Care. 2006;29(12):2755–7.
Aizawa T, Katakura M, Taguchi N, Kobayashi H, Aoyagi E, Hashizume K, Yoshizawa K. Ketoacidosis-onset noninsulin dependent diabetes in Japanese subjects. Am J Med Sci. 1995;310(5):198–201.
Matsui J, Tamasawa N, Tanabe J, Kasai N, Murakami H, Matsuki K, et al. Clinical characteristics of Japanese youth-onset type 2 diabetes with ketonuria. Diabetes Res Clin Pract. 2005;70(3):235–8.
Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan D, Peterson CM, et al. Tests of glycemia in diabetes. Diabetes Care. 2004;27(7):1761–73.
Acknowledgements
We acknowledge proofreading and editing by Benjamin Phillis at the Clinical Study Support Center, Wakayama Medical University.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to disclose.
Compliance with ethical standards
The study protocol was approved by the Japanese Red Cross Wakayama Medical Center Ethics Committee (No. 680, April 30. 2019), and all participants had the opportunity to opt-out of research. The necessity for written informed consent from each patient was waived in this retrospective study. We used clinical information obtained in routine clinical practice, and no patients refused to participate in the study. All procedures were in accordance with the institutional ethical standards regarding human experimentation and with the Declaration of Helsinki, as revised in Fortaleza, Brazil in October 2013.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

13340_2022_581_MOESM1_ESM.jpg
Supplementary file1 Supplemental Fig. 1 Patient enrollment procedures. Detailed patient enrollment procedures were described thoroughly in the method. Among consecutive outpatients with DM at our department and emergency room during the 2011- 2019 year, a total of 202 patients were recruited for the study. Based on the inclusion and exclusion procedures as indicated, patients with T1DM (n=21), patients with T2DM-IDDM (n=29), and patients with T2DM-NIDDM (n=22) during the follow-up period were analyzed. *T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; IDDM, insulin dependent diabetes mellitus; NIDDM, non-insulin dependent diabetes mellitus (JPG 256 KB)

13340_2022_581_MOESM2_ESM.jpg
Supplementary file2 Supplemental Fig. 2 ROC analysis of serum βOHB levels for diagnosis of T1DM from T2DM. Optimal cut-off value of βOHB for diagnosis of T1DM was estimated by ROC analysis. 2.5 mmol/l of βOHB had 95.2% of sensitivity and 56.9% of specificity, area under the curve (AUC) was 0.77871. *βOHB, beta-hydroxybutyrate; ROC, receiver-operating-characteristic; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus (JPG 66 KB)
About this article
Cite this article
Hirobata, T., Inaba, H., Kaido, Y. et al. Serum ketone body measurement in patients with diabetic ketoacidosis. Diabetol Int 13, 624–630 (2022). https://doi.org/10.1007/s13340-022-00581-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-022-00581-2