Abstract
Cerebral small vessel disease (CSVD) is the most common progressive vascular disease that causes vascular dementia. Aging and hypertension are major contributors to CSVD, but the pathophysiological mechanism remains unclear, mainly due to the lack of an ideal animal model. Our previous study revealed that vascular smooth muscle cell (VSMC)-specific myosin phosphatase target subunit 1 (MYPT1) knockout (MYPT1SMKO) leads to constant hypertension, prompting us to explore whether hypertensive MYPT1SMKO mice can be considered a novel CSVD animal model. Here, we found that MYPT1SMKO mice displayed age-dependent CSVD-like neurobehaviors, including decreased motion speed, anxiety, and cognitive decline. MYPT1SMKO mice exhibited remarkable white matter injury compared with control mice, as shown by the more prominent loss of myelin at 12 months of age. Additionally, MYPT1SMKO mice were found to exhibit CSVD-like small vessel impairment, including intravascular hyalinization, perivascular space enlargement, and microbleed and blood-brain barrier (BBB) disruption. Last, our results revealed that the brain of MYPT1SMKO mice was characterized by an exacerbated inflammatory microenvironment, which is similar to patients with CSVD. In light of the above structural and functional phenotypes that closely mimic the conditions of human CSVD, we suggest that MYPT1SMKO mice are a novel age- and hypertension-dependent animal model of CSVD.





Similar content being viewed by others
Data Availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
References
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689–701. https://doi.org/10.1016/S1474-4422(10)70104-6.
Gorelick, P.B., et al., Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke, 2011. 42(9): p. 2672-2713. https://doi.org/10.1161/STR.0b013e3182299496
de Leeuw FE, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J Neurol Neurosurg Psychiatry. 2001;70(1):9–14. https://doi.org/10.1136/jnnp.70.1.9.
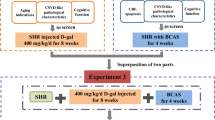
Mustapha M, et al. Cerebral small vessel disease (CSVD) - lessons from the animal models. Front Physiol. 2019;10:1317. https://doi.org/10.3389/fphys.2019.01317.
Kaiser D, et al. Spontaneous white matter damage, cognitive decline and neuroinflammation in middle-aged hypertensive rats: an animal model of early-stage cerebral small vessel disease. Acta Neuropathol Commun. 2014;2:169. https://doi.org/10.1186/s40478-014-0169-8.
Bailey EL, et al. Cerebral small vessel endothelial structural changes predate hypertension in stroke-prone spontaneously hypertensive rats: a blinded, controlled immunohistochemical study of 5- to 21-week-old rats. Neuropathol Appl Neurobiol. 2011;37(7):711–26. https://doi.org/10.1111/j.1365-2990.2011.01170.x.
Hannawi Y, et al. Characterizing the neuroimaging and histopathological correlates of cerebral small vessel disease in spontaneously hypertensive stroke-prone rats. Front Neurol. 2021;12:740298. https://doi.org/10.3389/fneur.2021.740298.
Yamagata K, Tagami M, Yamori Y. Neuronal vulnerability of stroke-prone spontaneously hypertensive rats to ischemia and its prevention with antioxidants such as vitamin E. Neuroscience. 2010;170(1):1–7. https://doi.org/10.1016/j.neuroscience.2010.07.013.
Meneses A, et al. Spontaneously hypertensive rat (SHR) as an animal model for ADHD: a short overview. Rev Neurosci. 2011;22(3):365–71. https://doi.org/10.1515/RNS.2011.024.
Shibata M, et al. White matter lesions and glial activation in a novel mouse model of chronic cerebral hypoperfusion. Stroke. 2004;35(11):2598–603. https://doi.org/10.1161/01.STR.0000143725.19053.60.
Yang Y, et al. Rodent models of vascular cognitive impairment. Transl Stroke Res. 2016;7(5):407–14. https://doi.org/10.1007/s12975-016-0486-2.
Joutel A, et al. Cerebrovascular dysfunction and microcirculation rarefaction precede white matter lesions in a mouse genetic model of cerebral ischemic small vessel disease. J Clin Invest. 2010;120(2):433–45. https://doi.org/10.1172/JCI39733.
Ruchoux MM, et al. Transgenic mice expressing mutant Notch3 develop vascular alterations characteristic of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Am J Pathol. 2003;162(1):329–42. https://doi.org/10.1016/S0002-9440(10)63824-2.
Wallays G, et al. Notch3 Arg170Cys knock-in mice display pathologic and clinical features of the neurovascular disorder cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Arterioscler Thromb Vasc Biol. 2011;31(12):2881–8. https://doi.org/10.1161/ATVBAHA.111.237859.
Cannistraro RJ, et al. CNS small vessel disease: a clinical review. Neurology. 2019;92(24):1146–56. https://doi.org/10.1212/WNL.0000000000007654.
Qiao YN, et al. Myosin phosphatase target subunit 1 (MYPT1) regulates the contraction and relaxation of vascular smooth muscle and maintains blood pressure. J Biol Chem. 2014;289(32):22512–23. https://doi.org/10.1074/jbc.M113.525444.
He WQ, et al. Altered contractile phenotypes of intestinal smooth muscle in mice deficient in myosin phosphatase target subunit 1. Gastroenterology. 2013;144(7):1456–65. https://doi.org/10.1053/j.gastro.2013.02.045.
Gebara E, et al. Mitofusin-2 in the nucleus accumbens regulates anxiety and depression-like behaviors through mitochondrial and neuronal actions. Biol Psychiatry. 2021;89(11):1033–44. https://doi.org/10.1016/j.biopsych.2020.12.003.
Tao W, et al. miR-204-3p/Nox4 mediates memory deficits in a mouse model of Alzheimer’s disease. Mol Ther. 2021;29(1):396–408. https://doi.org/10.1016/j.ymthe.2020.09.006.
Zheng L, et al. Pentoxifylline alleviates ischemic white matter injury through up-regulating Mertk-mediated myelin clearance. J Neuroinflammation. 2022;19(1):128. https://doi.org/10.1186/s12974-022-02480-4.
Jenkinson M, et al. Fsl. Neuroimage. 2012;62(2):782–90. https://doi.org/10.1016/j.neuroimage.2011.09.015.
Nie B, et al. A stereotaxic MRI template set of mouse brain with fine sub-anatomical delineations: Application to MEMRI studies of 5XFAD mice. Magn Reson Imaging. 2019;57:83–94. https://doi.org/10.1016/j.mri.2018.10.014.
Friston KJ. Commentary and opinion: II. Statistical parametric map**: ontology and current issues. J Cereb Blood Flow Metab. 1995;15(3):361–70. https://doi.org/10.1038/jcbfm.1995.45.
Yamazaki Y, et al. Vascular cell senescence contributes to blood-brain barrier breakdown. Stroke. 2016;47(4):1068–77. https://doi.org/10.1161/STROKEAHA.115.010835.
Li HQ, et al. Gamma-glutamylcysteine alleviates ischemic stroke-induced neuronal apoptosis by inhibiting ROS-mediated endoplasmic reticulum stress. Oxid Med Cell Longev. 2021;2021:2961079. https://doi.org/10.1155/2021/2961079.
Su N, et al. The consequence of cerebral small vessel disease: linking brain atrophy to motor impairment in the elderly. Hum Brain Mapp. 2018;39(11):4452–61. https://doi.org/10.1002/hbm.24284.
Edrissi H, et al. Cilostazol reduces blood brain barrier dysfunction, white matter lesion formation and motor deficits following chronic cerebral hypoperfusion. Brain Res. 2016;1646:494–503. https://doi.org/10.1016/j.brainres.2016.06.036.
Rensma SP, et al. Cerebral small vessel disease and risk of incident stroke, dementia and depression, and all-cause mortality: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;90:164–73. https://doi.org/10.1016/j.neubiorev.2018.04.003.
Duering M, et al. Strategic role of frontal white matter tracts in vascular cognitive impairment: a voxel-based lesion-symptom map** study in CADASIL. Brain. 2011;134(Pt 8):2366–75. https://doi.org/10.1093/brain/awr169.
Nordahl CW, et al. Different mechanisms of episodic memory failure in mild cognitive impairment. Neuropsychologia. 2005;43(11):1688–97. https://doi.org/10.1016/j.neuropsychologia.2005.01.003.
Chen JF, et al. Oligodendrocytes and myelin: active players in neurodegenerative brains? Dev Neurobiol. 2022;82(2):160–74. https://doi.org/10.1002/dneu.22867.
Tan XL, et al. Partial eNOS deficiency causes spontaneous thrombotic cerebral infarction, amyloid angiopathy and cognitive impairment. Mol Neurodegener. 2015;10:24. https://doi.org/10.1186/s13024-015-0020-0.
Meng H, et al. Synthetic VSMCs induce BBB disruption mediated by MYPT1 in ischemic stroke. iScience. 2021;24(9):103047. https://doi.org/10.1016/j.isci.2021.103047.
Zhang DD, et al. Inflammatory biomarkers and cerebral small vessel disease: a community-based cohort study. Stroke Vasc Neurol. 2022. https://doi.org/10.1136/svn-2021-001102.
Noz MP, et al. Trained immunity characteristics are associated with progressive cerebral small vessel disease. Stroke. 2018;49(12):2910–7. https://doi.org/10.1161/STROKEAHA.118.023192.
Verhaaren BF, et al. High blood pressure and cerebral white matter lesion progression in the general population. Hypertension. 2013;61(6):1354–9. https://doi.org/10.1161/HYPERTENSIONAHA.111.00430.
Wardlaw JM, et al. White matter hyperintensity reduction and outcomes after minor stroke. Neurology. 2017;89(10):1003–10. https://doi.org/10.1212/WNL.0000000000004328.
Shan LL, et al. Association of serum interleukin-8 and serum amyloid a with anxiety symptoms in patients with cerebral small vessel disease. Front Neurol. 2022;13:938655. https://doi.org/10.3389/fneur.2022.938655.
Yang Y, Rosenberg GA. Blood-brain barrier breakdown in acute and chronic cerebrovascular disease. Stroke. 2011;42(11):3323–8. https://doi.org/10.1161/STROKEAHA.110.608257.
Wardlaw JM, et al. Blood-brain barrier permeability and long-term clinical and imaging outcomes in cerebral small vessel disease. Stroke. 2013;44(2):525–7. https://doi.org/10.1161/STROKEAHA.112.669994.
De Silva TM, Miller AA. Cerebral small vessel disease: targeting oxidative stress as a novel therapeutic strategy? Front Pharmacol. 2016;7:61. https://doi.org/10.3389/fphar.2016.00061.
Guy R, et al. A novel rodent model of hypertensive cerebral small vessel disease with white matter hyperintensities and peripheral oxidative stress. Int J Mol Sci. 2022;23(11). https://doi.org/10.3390/ijms23115915.
Liao FF, et al. Endothelial nitric oxide synthase-deficient mice: a model of spontaneous cerebral small-vessel disease. Am J Pathol. 2021;191(11):1932–45. https://doi.org/10.1016/j.ajpath.2021.02.022.
Chen CP, et al. In vivo roles for myosin phosphatase targeting subunit-1 phosphorylation sites T694 and T852 in bladder smooth muscle contraction. J Physiol. 2015;593(3):681–700. https://doi.org/10.1113/jphysiol.2014.283853.
Acknowledgements
We thank Feng Han and Meiling Sun from Nan**g Medical University in China for their help in the two-photon imaging analysis.
Funding
This study was funded by the National Natural Science Foundation of China (82130036, 81920108017), the National Science and Technology Innovation 2030—Major program of “Brain Science and Brain-Like Research” 2022ZD0211800, the Key Research and Development Program of Jiangsu Province of China (BE2020620). Jiangsu Province Key Medical Discipline (ZDXKA2016020).
Author information
Authors and Affiliations
Contributions
YX designed research; JC, C-GL, L-XY, YQ, L-WZ, and P-YL performed research; JC, L-XY, and C-GL analyzed data; M-SZ developed the mice; YW assisted with animal breed; JC, YX wrote the paper. YX and M-SZ revised the paper. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
All the animal experiments were conducted according to institutional guidelines and were approved by the Animal Use and Care Committees at Nan**g University.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, J., Li, CG., Yang, LX. et al. MYPT1SMKO Mice Function as a Novel Spontaneous Age- and Hypertension-Dependent Animal Model of CSVD. Transl. Stroke Res. 15, 606–619 (2024). https://doi.org/10.1007/s12975-023-01142-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-023-01142-8