Abstract
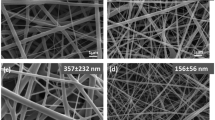
Recently, researchers have increasingly considered electrospun nanofibrous scaffolds for drug delivery systems due to their ability to control the release of various drugs and natural compounds. In our study, we utilized the uniaxial electrospinning technique to create nanofibrous scaffolds using polycaprolactone (PCL). Subsequently, curcumin (Cur) and vancomycin (Vn) were individually and synergically loaded into the electrospun PCL nanofibers (NFs). The nanofibrous scaffolds were meticulously characterized utilizing a comprehensive array of analytical techniques, including scanning electron microscopy (SEM) for morphological assessment, porosity evaluation for structural analysis, tensile strength measurements to gauge mechanical properties, and investigations into water vapor permeability, swelling kinetics, and degradation rates to assess performance and stability. Additionally, the release profiles of Cur and Vn were analyzed using spectrophotometry. Upon seeding HFF-2 cells on the fabricated scaffolds, we performed cytotoxicity and cytoprotective assessments using the MTT assay. Furthermore, the morphology of the cells on the scaffolds was investigated through SEM micrographs. The obtained results indicated that the fiber diameter for PCL, PCL/Cur, PCL/Vn, and PCL/ Vn-Cur was 204 ± 52, 218 ± 63, 227 ± 74, and 238 ± 72, respectively. The MTT assay confirmed that all nanofiber groups were non-toxic and biocompatible. Notably, PCL/Cur and PCL/Vn-Cur demonstrated increased cell viability and proliferation of human foreskin fibroblast (HFF-2) cells. The cytocompatibility study of Cur and Vn loaded nanofibers (NFs) revealed a synergistic effect, leading to enhanced relative cell viability when exposing HFF-2 cells to H2O2, an oxidant compound. SEM imaging provided additional evidence of the favorable cell adhesion on the nanofibrous scaffolds, corroborating the results obtained from the MTT assay. This observation underscores the efficacy of the Vn-Cur-loaded NFs in promoting cell attachment and proliferation, highlighting their potential for tissue engineering and wound healing applications.







Similar content being viewed by others
Data Availability
Not applicable.
Abbreviations
- EN:
-
Electrospinning
- NFs:
-
Nanofibers
- PCL:
-
Polycaprolactone
- Cur:
-
Curcumin
- Vn:
-
Vancomycin
- AA:
-
Acetic acid
- FA:
-
Formic acid
- PBS:
-
Phosphate-buffered saline
- MTT:
-
(4,5-Dimethyl- 2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide
- DMEM:
-
Dulbecco’s modified eagle’s medium
- DMSO:
-
Dimethyl sulfoxide
- WVTR:
-
Water vapor transition rate
- H2O2 :
-
Hydrogen peroxide
- GA:
-
Glutaraldehyde
- HFF-2:
-
Human foreskin fibroblast
References
Sabbagh, F., & Kim, B. S. (2022). Recent advances in polymeric transdermal drug delivery systems. Journal of Controlled Release,341, 132–146.
Hu, X., Liu, S., Zhou, G., Huang, Y., **e, Z., & **g, X. (2014). Electrospinning of polymeric nanofibers for drug delivery applications. Journal of Controlled Release,185(1), 12–21.
Hajati Ziabari, A., Ebrahimi, S., Jafari, K., Doodmani, S. M., Natouri, O., Nobakht, A., et al. (2024). Bilayer nanofibers loaded with Malva sylvestris extract for enhanced wound healing applications. Journal of Drug Delivery Science and Technology,93, 105373.
Doodmani, S. M., Bagheri, A., Natouri, O., Nobakht, A., & Saghebasl, S. (2024). Electrospinning-netting of spider-inspired polycaprolactone/collagen nanofiber-nets incorporated with Propolis extract for enhanced wound healing applications. International Journal of Biological Macromolecules, 267(Pt 1), 131452.
Parın, F. N., Ullah, A., Yeşilyurt, A., Parın, U., Haider, M. K., & Kharaghani, D. (2022). Development of PVA–psyllium husk meshes via emulsion electrospinning: Preparation, characterization, and antibacterial activity. Polymers (Basel), 14(7), 1490.
Haider, M. K., Kharaghani, D., Sun, L., Ullah, S., Sarwar, M. N., Ullah, A., et al. (2023). Synthesized bioactive lignin nanoparticles/polycaprolactone nanofibers: A novel nanobiocomposite for bone tissue engineering. Biomaterials Advances,144, 213203.
Phan, D. N., Khan, M. Q., Nguyen, V. C., Vu-Manh, H., Dao, A. T., Thanh Thao, P., et al. (2022). Investigation of mechanical, chemical, and antibacterial properties of electrospun cellulose-based scaffolds containing orange essential oil and silver nanoparticles. Polymers (Basel), 14(1), 85.
Ullah, A., Ullah, S., Khan, M. Q., Hashmi, M., Nam, P. D., Kato, Y., et al. (2020). Manuka honey incorporated cellulose acetate nanofibrous mats: Fabrication and in vitro evaluation as a potential wound dressing. International Journal of Biological Macromolecules,155, 479–489.
Abdollahi, A., Mirzaei, E., Amoozegar, F., Moemenbellah-Fard, M. D., Zarenezhad, E., & Osanloo, M. (2021). High antibacterial effect of impregnated nanofiber mats with a green nanogel against major human pathogens. Bionanoscience,11, 549–558.
Haider, M. K., Kharaghani, D., Yoshiko, Y., & Kim, I. S. (2023). Lignin-facilitated growth of Ag/CuNPs on surface-activated polyacryloamidoxime nanofibers for superior antibacterial activity with improved biocompatibility. International Journal of Biological Macromolecules,242, 124945.
Prabaharan, M., Jayakumar, R., & Nair, S. V. (2012). Electrospun nanofibrous scaffolds-Current status and prospects in drug delivery. Advances in Polymer Science, Biomedical Applications of Polymeric Nanofibers, pp 241–262.
Zhang, Y., Chwee, T. L., Ramakrishna, S., & Huang, Z. M. (2005). Recent development of polymer nanofibers for biomedical and biotechnological applications. Journal of Materials Science: Materials in Medicine,16, 933–946.
Mitra, S., Mateti, T., Ramakrishna, S., & Laha, A. (2022). A review on curcumin-loaded electrospun nanofibers and their application in modern medicine. JOM Journal of the Minerals Metals and Materials Society (1989), 74, 3392–3407.
Teodoro, K. B. R., Alvarenga, A. D., Rocha Oliveira, L. F., Marques Chagas, P. A., Lopes, R. G., da Silveira Andre, R., et al. (2023). Fast Fabrication of multifunctional PCL/curcumin nanofibrous membranes for wound dressings. ACS Applied Bio Materials,6(6), 2325–2337.
Van An, N., Hoang, L. H., Le, H. H. L., Thai Son, N., Hong, L. T., Viet, T. T., et al. (2023). Distribution and antibiotic resistance characteristics of bacteria isolated from blood culture in a teaching hospital in Vietnam during 2014–2021. Infection and Drug Resistance,31(16), 1677–1692.
Belykh, E., Carotenuto, A., Kalinin, A. A., Akshulakov, S. K., Kerimbayev, T., Borisov, V. E., et al. (2019). Surgical protocol for infections, nonhealing wound prophylaxis, and analgesia: Development and implementation for posterior spinal fusions. World Neurosurgery,123, 390–401.
Ghobrial, G. M., Thakkar, V., Andrews, E., Lang, M., Chitale, A., Oppenlander, M. E., et al. (2014). Intraoperative vancomycin use in spinal surgery: Single institution experience and microbial trends. Spine (Phila Pa 1976),39(7), 550–555.
Liu, J. X., Bravo, D., Buza, J., Kirsch, T., Kennedy, O., Rokito, A., et al. (2018). Topical vancomycin and its effect on survival and migration of osteoblasts, fibroblasts, and myoblasts: An in vitro study. Journal of Orthopaedics,15(1), 53–58.
Herten, M., Idelevich, E. A., Sielker, S., Becker, K., Scherzinger, A. S., Osada, N., et al. (2017). Vascular graft impregnation with antibiotics: The influence of high concentrations of rifampin, vancomycin, daptomycin, and bacteriophage endolysin HY-133 on viability of vascular cells. Medical Science Monitor Basic Research,23, 250.
Ullah, A., Haider, M. K., Wang, F. F., Morita, S., Kharaghani, D., Ge, Y., et al. (2022). “Clay-corn-caprolactone” a novel bioactive clay polymer nanofibrous scaffold for bone tissue engineering. Applied Clay Science,220, 106455.
Teodoro, K. B. R., Alvarenga, A. D., Marques Chagas, P. A., Lopes, R. G., Alves, F., Stringasci, M. D., et al. (2024). Synergistic tetracycline–curcumin association in biocompatible PCL nanostructured wound dressings. ACS Applied Polymer Materials,6(9), 5089–5101.
Nandhini, P., Ramya, R. D., Murugan, M., & Rajan, M. (2023). Vancomycin and curcumin-loaded zinc oxide functionalized chitosan carrier for the treatment of multi-drug resistant bacterial infection. Journal of Materials Science,58(11), 4922–4936.
Heris, M. A., Jahandideh, A., Akbarzadeh, A., & Mortazavi, P. (2024). Dual-loaded poly (ε-caprolactone) nanofibers for wound healing applications: Co-delivery of clindamycin and propolis extract for synergistic therapeutic effects. Bionanoscience, 1–14. https://doi.org/10.1007/s12668-024-01337-9
Behere, I., & Ingavle, G. (2022). In vitro and in vivo advancement of multifunctional electrospun nanofiber scaffolds in wound healing applications: Innovative nanofiber designs, stem cell approaches, and future perspectives. Journal of Biomedical Materials Research, Part A,110(2), 443–461.
Han, C., Cai, N., Chan, V., Liu, M., Feng, X., & Yu, F. (2018). Enhanced drug delivery, mechanical properties and antimicrobial activities in poly(lactic acid) nanofiber with mesoporous Fe3O4-COOH nanoparticles. Colloids and Surfaces A: Physicochemical and Engineering Aspects,559, 104–114.
Motasadizadeh, H., Azizi, S., Shaabani, A., Sarvestani, M. G., Sedghi, R., & Dinarvand, R. (2022). Development of PVA/chitosan-g-poly (N-vinyl imidazole)/TiO2/curcumin nanofibers as high-performance wound dressing. Carbohydrate Polymers,296, 119956.
Pham, Q. P., Sharma, U., & Mikos, A. G. (2006). Electrospun poly (ε-caprolactone) microfiber and multilayer nanofiber/microfiber scaffolds: Characterization of scaffolds and measurement of cellular infiltration. Biomacromolecules,7(10), 2796–2805.
Malik, R., Garg, T., Goyal, A. K., & Rath, G. (2015). Polymeric nanofibers: Targeted gastro-retentive drug delivery systems. Journal of Drug Targeting,23(2), 109–124.
Shi, S., Wu, H., Zhi, C., Yang, J., Si, Y., Ming, Y., et al. (2023). A skin-like nanostructured membrane for advanced wound dressing. Composites Part B: Engineering,250, 110438.
Ramakrishna, S., Fujihara, K., Teo, W. E., Lim, T. C., & Ma, Z. (2005). An Introduction to Electrospinning and Nanofibers, pp. 1–382. https://doi.org/10.1142/9789812567611_0003
Fahimirad, S., Abtahi, H., Satei, P., Ghaznavi-Rad, E., Moslehi, M., & Ganji, A. (2021). Wound healing performance of PCL/chitosan based electrospun nanofiber electrosprayed with curcumin loaded chitosan nanoparticles. Carbohydrate Polymers,259, 117640.
Figueira, D. R., Miguel, S. P., de Sá, K. D., & Correia, I. J. (2016). Production and characterization of polycaprolactone- hyaluronic acid/chitosan- zein electrospun bilayer nanofibrous membrane for tissue regeneration. International Journal of Biological Macromolecules,93, 1100–1110.
Davoudi, Z., Akbarzadeh, A., Rahmatiyamchi, M., Movassaghpour, A. A., Alipour, M., Nejati-Koshki, K., Sadeghi, Z., Dariushnejad, H., & Zarghami, N. (2014). Molecular target therapy of AKT and NF-kB signaling pathways and multidrug resistance by specific cell penetrating inhibitor peptides in HL-60 cells. Asian Pacific Journal of Cancer Prevention,15(10), 4353–4358.
Badrzadeh, F., Akbarzadeh, A., Zarghami, N., Yamchi, M. R., Zeighamian, V., Tabatabae, F. S., Taheri, M., & Kafil, H. S. (2014). Comparison between effects of free curcumin and curcumin loaded NIPAAm-MAA nanoparticles on telomerase and PinX1 gene expression in lung cancer cells. International Asian Pacific Journal of Cancer Prevention,15(20), 8931–8936.
Xue, J., Wu, T., Dai, Y., & **a, Y. (2019). Electrospinning and electrospun nanofibers: Methods, materials, and applications. Chemical Reviews,119(8), 5298–5415.
Augustine, R., Rehman, S. R. U., Ahmed, R., Zahid, A. A., Sharifi, M., Falahati, M., et al. (2020). Electrospun chitosan membranes containing bioactive and therapeutic agents for enhanced wound healing. International Journal of Biological Macromolecules,156, 153–170.
Patra, J. K., Das, G., Fraceto, L. F., Campos, E. V. R., Rodriguez-Torres, M. D. P., Acosta-Torres, L. S., et al. (2018). Nano based drug delivery systems: Recent developments and future prospects. Journal of Nanobiotechnology,16, 1–33.
Samadishadlou, M., Farshbaf, M., Annabi, N., Kavetskyy, T., Khalilov, R., Saghfi, S., Akbarzadeh, A., & Mousavi, S. (2018). Magnetic carbon nanotubes: Preparation, physical properties, and applications in biomedicine. Artificial Cells, Nanomedicine, and Biotechnology,46(7), 1313–1330.
Fathi, H. A., Abdelkader, A., AbdelKarim, M. S., Abdelaziz, A. A., El-Mokhtar, M. A., Allam, A., et al. (2020). Electrospun vancomycin-loaded nanofibers for management of methicillin-resistant Staphylococcus aureus-induced skin infections. International Journal of Pharmaceutics,586, 119620.
Cui, W., Zhou, Y., & Chang, J. (2010). Electrospun nanofibrous materials for tissue engineering and drug delivery. Science and Technology of Advanced Materials,11(1), 014108.
Sundelacruz, S., & Kaplan, D. L (2009) Stem cell- and scaffold-based tissue engineering approaches to osteochondral regenerative medicine. In Seminars in cell & developmental biology (Vol. 20, No. 6, pp. 646–655). Academic Press.
Merrell, J. G., McLaughlin, S. W., Tie, L., Laurencin, C. T., Chen, A. F., & Nair, L. S. (2009). Curcumin-loaded poly(ε-caprolactone) nanofibres: Diabetic wound dressing with anti-oxidant and anti-inflammatory properties. Clinical and Experimental Pharmacology and Physiology,36(12), 1149–1156.
Hasan, R., Sumnu, G., Sahin, S., Oz, E., & Oz, F. (2023). The effects of citric acid crosslinking on fabrication and characterization of gelatin/curcumin-based electrospun antioxidant nanofibers. Antioxidants,12(7), 1387.
Lim, G. P., Chu, T., Yang, F., Beech, W., Frautschy, S. A., & Cole, G. M. (2001). The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. Journal of Neuroscience,21(21), 8370–8377.
Duvoix, A., Blasius, R., Delhalle, S., Schnekenburger, M., Morceau, F., Henry, E., et al. (2005). Chemopreventive and therapeutic effects of curcumin. Cancer Letters,223(2), 181–190.
Panchatcharam, M., Miriyala, S., Gayathri, V. S., & Suguna, L. (2006). Curcumin improves wound healing by modulating collagen and decreasing reactive oxygen species. Molecular and Cellular Biochemistry,290(1–2), 87–96.
Funding
The authors would like to thank the Department of Clinical Science, Science and Research Branch, Islamic Azad University, and the Department of Medical Nanotechnology, Faculty of Advanced Medical Sciences, Tabriz University of Medical Sciences for financially supporting this project (grant no: 62379).
Author information
Authors and Affiliations
Contributions
AHZ: conceptualization, methodology, investigation, formal analysis, and writing—review and editing. AA: writing—original draft and writing—review and editing. PM: methodology and investigation. AJ and AA: project administration, conceptualization, supervision, resources, and funding acquisition.
Corresponding author
Ethics declarations
Ethical Approval
The ethical approval for this paper was obtained from the research ethics committee of Tabriz University of Medical Sciences)IR.TBZMED.VCR.REC.1398.487(.
Research Involving Humans and Animals Statement
None.
Consent to Participate
None.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ziabari, A.H., Jahandideh, A., Akbarzadeh, A. et al. Poly(Ε-Caprolactone) (PCL) Nanofibers as a Potent Platform for Co-Delivery of Vancomycin and Curcumin: Drug Release Profiling and Biophysically In-Vitro Investigating. BioNanoSci. (2024). https://doi.org/10.1007/s12668-024-01488-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s12668-024-01488-9