Abstract
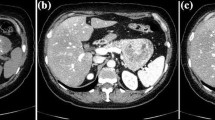
A 52-year-old man was transported via an ambulance because of syncope and the passage of tarry stools, which had been noted the previous day. He was diagnosed with upper gastrointestinal bleeding from a gastric ulcer and underwent endoscopic hemostasis. Prior to endoscopy, abdominal computerized tomography performed for gastrointestinal bleeding revealed pancreatic duct dilation. After discharge, abdominal imaging revealed a strongly enhancing tumor (5 mm) with caudal pancreatic duct dilation. Endoscopic retrograde pancreatography revealed that the main pancreatic duct was interrupted at the body. Pancreatic juice cytology was class III, and additional immunostaining were positive for chromogranin A, synaptophysin, and serotonin, suggesting a pancreatic neuroendocrine neoplasm (NEN). Distal pancreatectomy was performed and a yellowish-white solid lesion was found in the pancreatic duct. Pathological examination revealed narrowing of the pancreatic duct, extensive stromal fibrosis, and proliferation of tumor cells with small round nuclei and eosinophilic vesicles. Furthermore, the immunostaining findings of the resected specimen corresponded with those of the cytology. A diagnosis of NEN G1 (WHO classification) with Ki-67 index < 1% was made. Imaging of the pancreatic duct tend to be normal or show no involvement of the duct in pancreatic neuroendocrine neoplasms; however, there have been a few reports of stenosis due to fibrosis around the pancreatic duct. Serotonin positivity was previously documented to be significantly higher in patients with fibrosis. In lesions with pancreatic ductal stenosis, the addition of immunostaining to pancreatic juice cytology was thought to be useful in differentiating pancreatic cancer from pNEN.



Similar content being viewed by others
References
Verbeke CS. Endocrine tumours of the pancreas. Histopathology. 2010;56:669–82.
Obara T, Shudo R, Fujii T, et al. Pancreatic duct obstruction caused by malignant islet cell tumors of the pancreas. Gastrointest Endosc. 2000;51:604–7.
Klimstra DSKG, La Rosa S. Classification of neuroendocrine neoplasms of the digestive system, vol. 1. Lyon: World Health Organization; 2019.
Seki M, Ninomiya E, Ohta T, et al. Pancreatic endocrine tumor: pancreatographic features. J Jpn Panc Soc. 2001;16:438–47.
Sasano H, Tanaka M, et al. Epidemiological study of gastroenteropancreatic neuroendocrine tumors in Japan. J Gastroenterol. 2010;45:234–43.
Lee SL, Wang WW, Lanzillo JJ, et al. Serotonin produces both hyperplasia and hypertrophy of bovine pulmonary artery smooth muscle cells in culture. Am J Physiol. 1994;266:L46-52.
Bettini R, Partelli S, Boninsegna L, et al. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery. 2011;150:75–82.
Svejda B, Kidd M, Giovinazzo F, et al. The 5-HT(2B) receptor plays a key regulatory role in both neuroendocrine tumor cell proliferation and the modulation of the fibroblast component of the neoplastic microenvironment. Cancer. 2010;116:2902–12.
Shi C, Siegelman SS, Kawamoto S, et al. Pancreatic duct stenosis secondary to small endocrine neoplasms: a manifestation of serotonin production? Radiology. 2010;257:107–14.
Nishihara K, Matsunaga H, Tanabe R, et al. Endocrine tumor of the pancreas: impact of the endoscopic retrograde pancreatography findings. J Japan Pancreas Soc. 2008;23:671–5.
Nanno Y, Matsumoto I, Zen Y, et al. Pancreatic duct involvement in well-differentiated neuroendocrine tumors is an independent poor prognostic factor. Ann Surg Oncol. 2017;24:1127–33.
Takikawa T, Kikuta K, Hamada S, et al. A new preoperative scoring system for predicting aggressiveness of non-functioning pancreatic neuroendocrine neoplasms. Diagnostics (Basel). 2022;12:397.
Acknowledgements
We would like to thank pathologist Dr. Norio Takayashiki and pathology technicians Naoki Uchiyama and Junichi Hakamaduka for their help in diagnosing the disease. The authors thank the anonymous reviewers for their comments on an earlier version of this paper.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest directly relevant to the content of this article.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ariga, H., Kashimura, J., Horigome, Y. et al. Serotonin-positive neuroendocrine neoplasm with pancreatic ductal dilation in which cytological immunostaining contributed to the diagnosis. Clin J Gastroenterol 15, 822–825 (2022). https://doi.org/10.1007/s12328-022-01632-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-022-01632-6