Abstract
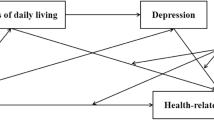
Residents’ quality of life (QOL) is an important indicator of their well-being, both physically and mentally, along with their social relations. Improving their QOL is an important developmental goal for governments around the world. This study aims to provide a new perspective on the relationship between leisure-time physical activity and residents’ QOL. It also seeks to provide theoretical references for improving residents’ QOL through two mediating variables, sleep quality and depressed mood, and the chain mediation model formed between them. This study conducted a questionnaire survey on 538 residents based on the Physical Activity Rating Scale, the Pittsburgh Sleep Quality Index, the Depression Self-Rating Scale, and the World Health Organization Quality of Survival Measurement Scale in Chinese, with the actual situation taken into account in the design of the questionnaire. AMOS software was employed to construct a chain mediation model between leisure-time physical activity and residents’ QOL, with Bootstrap** used to test the mediation effect. Leisure-time physical activity had a significant effect on residents’ QOL; both sleep quality and depression showed significant individual mediation effects, as well as chain mediation effects, between leisure-time physical activity and residents’ QOL. Depression and sleep quality play a significant role in better residents’ QOL of life through leisure-time physical activity. Increased individual knowledge of leisure-time physical activity and improved leisure-time physical activity behaviors can effectively alleviate depression, improve sleep quality, and thus promote overall QOL.


Similar content being viewed by others
Data availability
The dataset used and analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable
References
Abraham, R., Leonhardt, M., Lien, L., Hanssen, I., Hauff, E., & Thapa, S. B. (2022). The relationship between religiosity/spirituality and quality of life among female Eritrean refugees living in Norwegian asylum centres. International Journal of Social Psychiatry, 68(4), 881–890. https://doi.org/10.1177/00207640211010207
Al-Janabi, H., Wittenberg, E., Donaldson, C., & Brouwer, W. (2022). The relative value of carer and patient quality of life: A person trade-off (PTO) study. Social Science & Medicine, 292, Article 114556. https://doi.org/10.1016/j.socscimed.2021.114556
Amelia, V. L., Jen, H.-J., Lee, T.-Y., Chang, L.-F., & Chung, M.-H. (2022). Comparison of the Associations between Self-Reported Sleep Quality and Sleep Duration Concerning the Risk of Depression: A Nationwide Population-Based Study in Indonesia. International Journal of Environmental Research and Public Health, 19(21), Article 14273. https://doi.org/10.3390/ijerph192114273
An, Y., Yang, Y., Wang, A. P., Li, Y., Zhang, Q. G., Cheung, T., Ungvari, G. S., Qin, M. Z., An, F. R., & **ang, Y. T. (2020). Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. Journal of Affective Disorders, 276, 312–315. https://doi.org/10.1016/j.jad.2020.06.047
Aqeel, M., Rehna, T., Shuja, K. H., & Abbas, J. (2022). Comparison of students’ mental wellbeing, anxiety, depression, and quality of life during COVID-19’s full and partial (Smart) lockdowns: A follow-up study at a 5-month interval. Frontiers in Psychiatry, 13, Article 835585. https://doi.org/10.3389/fpsyt.2022.835585
Azharuddin, M., Kapur, P., & Sharma, M. (2021). Association between sleep quality and health-related quality of life in Indian Type 2 diabetes mellitus outpatients: Evidence from a cross-sectional study. Metabolism-Clinical and Experimental, 116, 44–44. https://doi.org/10.1016/j.metabol.2020.154575
Bai, W., Zhao, Y. J., Cai, H., Sha, S., Zhang, Q. E., Lei, S. M.,... **ang, Y. T. (2022). Network analysis of depression, anxiety, insomnia and quality of life among Macau residents during the COVID-19 pandemic. Journal of Affective Disorders, 311, 181–188. https://doi.org/10.1016/j.jad.2022.05.061
Bai, Y.-L., Chang, Y.-Y., Chiou, C.-P., & Lee, B.-O. (2019). Mediating effects of fatigue on the relationships among sociodemographic characteristics, depression, and quality of life in patients receiving hemodialysis [Article]. Nursing & Health Sciences, 21(2), 231–238. https://doi.org/10.1111/nhs.12587
Bindewald, J., Oeken, J., Wollbrueck, D., Wulke, C., Dietz, A., Herrmann, E., Schwarz, R., & Singer, S. (2007). Quality of life correlates after surgery for laryngeal carcinoma. Laryngoscope, 117(10), 1770–1776. https://doi.org/10.1097/MLG.0b013e3180caa18c
Blafoss, R., Sundstrup, E., Jakobsen, M.D., Bay, H., Garde, A.H., & Andersen, L.L. (2019). Are insomnia type sleep problems associated with a less physically active lifestyle? A cross-sectional study among 7,700 adults from the general working population. Frontiers in Public Health, 7, Article 117. https://doi.org/10.3389/fpubh.2019.00117
Brailovskaia, J., & Margraf, J. (2020). Relationship between depression symptoms, physical activity, and addictive social media use. Cyberpsychology Behavior and Social Networking, 23(12), 818–822. https://doi.org/10.1089/cyber.2020.0255
Buysse, D. J., Reynolds, C. F., 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Celik, N., Ceylan, B., Unsal, A., & Cagan, O. (2019). Depression in health college students: relationship factors and sleep quality [Article]. Psychology Health & Medicine, 24(5), 625–630. https://doi.org/10.1080/13548506.2018.1546881
Chae, S.-M., Kang, H.S., & Ra, J.S. (2017). Body esteem is a mediator of the association between physical activity and depression in Korean adolescents. Applied Nursing Research, 33, 42–48. https://doi.org/10.1016/j.apnr.2016.10.001
Chen, J., Chen, X., Mao, R., Fu, Y., Chen, Q., Zhang, C., & Zheng, K. (2023). Hypertension, sleep quality, depression, and cognitive function in elderly: A cross-sectional study. Frontiers in Aging Neuroscience, 15, Article 1051298. https://doi.org/10.3389/fnagi.2023.1051298
Cheng, M., Lei, X., Zhu, C., Hou, Y., Lu, M., Wang, X., & Wu, Q. (2022). The association between poor sleep quality and anxiety and depression symptoms in Chinese patients with coronary heart disease [Article]. Psychology Health & Medicine, 27(6), 1347–1356. https://doi.org/10.1080/13548506.2021.1874440
Ciomperlik, H., Dhanani, N. H., Cassata, N., Mohr, C., Bernardi, K., Holihan, J. L., Lyons, N., Olavarria, O., Ko, T. C., & Liang, M. K. (2021). Patient quality of life before and after ventral hernia repair. Surgery, 169(5), 1158–1163. https://doi.org/10.1016/j.surg.2020.11.003
Craike, M., Bourke, M., Hilland, T. A., Wiesner, G., Pascoe, M. C., Bengoechea, E. G., & Parker, A. G. (2019). Correlates of physical activity among disadvantaged groups: A systematic review. American Journal of Preventive Medicine, 57(5), 700–715. https://doi.org/10.1016/j.amepre.2019.06.021
Dodge, T., Vaylay, S., & Kracke-Bock, J. (2022). Subjective vitality: a benefit of self-directed, leisure time physical activity. Journal of Happiness Studies, 23(6), 2903–2922. https://doi.org/10.1007/s10902-022-00528-z
Eder, A. B. (2023). A perceptual control theory of emotional action [Article]. Cognition & Emotion, 37(7), 1167–1184. https://doi.org/10.1080/02699931.2023.2265234
Fekedulegn, D., Innes, K., Andrew, M.E., Tinney-Zara, C., Charles, L.E., Allison, P., Violanti, J. M., & Knox, S. S. (2018). Sleep quality and the cortisol awakening response (CAR) among law enforcement officers: The moderating role of leisure time physical activity. Psychoneuroendocrinology, 95, 158–169. https://doi.org/10.1016/j.psyneuen.2018.05.034
Forte, P., & Monteiro, A.M. (2022). The physical activity and exercise as key role topic in sports medicine for old people quality of life [Editorial Material]. Medicina-Lithuania, 58(6), Article 797. https://doi.org/10.3390/medicina58060797
Fukushima, T., Nakano, J., Hashizume, K., Ueno, K., Matsuura, E., Ikio, Y., Ishii, S., Morishita, S., Tanaka, K., & Kusuba, Y. (2021). Effects of aerobic, resistance, and mixed exercises on quality of life in patients with cancer: A systematic review and meta-analysis. Complementary Therapies in Clinical Practice, 42, Article 101290. https://doi.org/10.1016/j.ctcp.2020.101290
Gao, T., **ang, Y.-T., Zhang, H., Zhang, Z., & Mei, S. (2017). Neuroticism and quality of life: Multiple mediating effects of smartphone addiction and depression. Psychiatry Research, 258, 457–461. https://doi.org/10.1016/j.psychres.2017.08.074
Gujral, S., Aizenstein, H., Reynolds, C.F., III, Butters, M.A., & Erickson, K.I. (2017). Exercise effects on depression: Possible neural mechanisms. General Hospital Psychiatry, 49, 2–10. https://doi.org/10.1016/j.genhosppsych.2017.04.012
He, H.M., Mo, Q.Q., Bai, X.Y., Chen, X. G., Jia, C.X., Zhou, L., & Ma, Z. Y. (2021). Studying suicide using proxy-based data: reliability and validity of a short version scale for measuring quality of life in rural China. Peerj, 9, Article e12396. https://doi.org/10.7717/peerj.12396
Huber, F. A., Toledo, T. A., Newsom, G., & Rhudy, J.L. (2022). The relationship between sleep quality and emotional modulation of spinal, supraspinal, and perceptual measures of pain. Biological Psychology, 171, Article 108352. https://doi.org/10.1016/j.biopsycho.2022.108352
Irwin, P., Taylor, D., & Keefe, J. M. (2023). Provincial policies affecting resident quality of life in Canadian residential long-term care. Bmc Geriatrics, 23(1), Article 362. https://doi.org/10.1186/s12877-023-04074-y
Izdonaite-Medziuniene, I., & Preiksaitiene, L. (2024). Disposition of improving quality of life in older adults: the case of Lithuania. Aging Clinical and Experimental Research, 36(1), Article 26. https://doi.org/10.1007/s40520-023-02687-2
Jackson, D. L. (2003). Revisiting sample size and number of parameter estimates: Some support for the N:Q hypothesis. Structural Equation Modeling-a Multidisciplinary Journal, 10(1), 128–141. https://doi.org/10.1207/s15328007sem1001_6
Jansson, T. (2023). Permanent residence permits and demands for integration: A genealogical analysis of Swedish immigration policy. Journal of Ethnic and Migration Studies. https://doi.org/10.1080/1369183x.2023.2290451
Ji, C., Yang, J., Lin, L., & Chen, S. (2022). Anxiety and sleep quality amelioration in college students: A comparative study between team sports and individual sports. Behavioral Sciences, 12(5), Article 149. https://doi.org/10.3390/bs12050149
Kim, H.-Y. (2013). Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restorative Dentistry & Endodontics, 38(1), 52–54. https://doi.org/10.5395/rde.2013.38.1.52
Kim, J., Chun, S., Heo, J., Lee, S., & Han, A. (2016). Contribution of leisure-time physical activity on psychological benefits among elderly immigrants. Applied Research in Quality of Life, 11(2), 461–470. https://doi.org/10.1007/s11482-014-9374-7
Kudrnacova, M., & Kudrnac, A. (2023). Better sleep, better life? testing the role of sleep on quality of life. Plos One, 18(3), Article e0282085. https://doi.org/10.1371/journal.pone.0282085
Kuhlthau, K. A., McDonnell, E., Coury, D. L., Payakachat, N., & Macklin, E. (2018). Associations of quality of life with health-related characteristics among children with autism. Autism, 22(7), 804–813. https://doi.org/10.1177/1362361317704420
Lee, D. H., Rezende, L. F. M., Joh, H. K., Keum, N., Ferrari, G., Rey-Lopez, J. P., Rimm, E. B., Tabung, F. K., & Giovannucci, E. L. (2022a). Long-term leisure-time physical activity intensity and all-cause and cause-specific mortality: A prospective cohort of US adults. Circulation, 146(7), 523–534. https://doi.org/10.1161/circulationaha.121.058162
Lee, M.C., Chen, Y.Y., Tai, C. Y., & Wu, S.F.V. (2022b). The mediating effect of self-efficacy in the relationship between mental health and quality of life in patients with hypertensive nephrology. Journal of Advanced Nursing, 78(9), 2827–2836. https://doi.org/10.1111/jan.15199
Li, Y., & Guo, K. (2023). Research on the relationship between physical activity, sleep quality, psychological resilience, and social adaptation among Chinese college students: A cross-sectional study. Frontiers in Psychology, 14, Article 1104897. https://doi.org/10.3389/fpsyg.2023.1104897
Lin, C.-H., Hsu, Y.-J., Hsu, P.-H., Lee, Y.-L., Lin, C.-H., Lee, M.-S., & Chiang, S.-L. (2021). Effects of intradialytic exercise on dialytic parameters, health-related quality of life, and depression status in hemodialysis patients: A randomized controlled trial. International Journal of Environmental Research and Public Health, 18(17), Article 9205. https://doi.org/10.3390/ijerph18179205
Lin, M.-C., Livneh, H., Lu, M.-C., Chang, C.-H., Chen, M.-L., & Tsai, T.-Y. (2023). Effects of a walking exercise programme on disease activity, sleep quality, and quality of life in systemic lupus erythematosus patients. International Journal of Nursing Practice. https://doi.org/10.1111/ijn.13174
Liu, Y., Feng, Q., & Guo, K. (2023). Physical activity and depression of Chinese college students: chain mediating role of rumination and anxiety [Article]. Frontiers in Psychology, 14, Article 1190836. https://doi.org/10.3389/fpsyg.2023.1190836
Lochbaum, M., Stoner, E., Hefner, T., Cooper, S., Lane, A. M., & Terry, P. C. (2022). Sport psychology and performance meta-analyses: A systematic review of the literature. Plos One, 17(2), Article e0263408. https://doi.org/10.1371/journal.pone.0263408
Martin-Parent, M. A., & Dewart, G. (2023). Promoting resident autonomy to maintain quality of life. Journal of the American Medical Directors Association, 24(9), 1266–1270. https://doi.org/10.1016/j.jamda.2023.06.021
Mazaheri, M., Gharraee, B., Shabani, A., & Lotfi, M. (2019). Studying the predictive factors of suicide attempts in patients with type 1 bipolar disorder. Psychiatry Research, 275, 373–378. https://doi.org/10.1016/j.psychres.2019.04.012
Miller, K. E., & Woodward, S. H. (2020). Wakemeter relies on changing perception thresholds across sleep stages. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 16(5), 825–825. https://doi.org/10.5664/jcsm.8418
Nang, E. E. K., Khoo, E. Y. H., Salim, A., Tai, E. S., Lee, J., & Van Dam, R. M. (2010). Patterns of physical activity in different domains and implications for intervention in a multi-ethnic Asian population: a cross-sectional study. Bmc Public Health, 10, Article 644. https://doi.org/10.1186/1471-2458-10-644
Nuzzo, J. L. (2023). Narrative review of sex differences in muscle strength, endurance, activation, size, fiber type, and strength training participation rates, preferences, motivations, injuries, and neuromuscular adaptations. Journal of Strength and Conditioning Research, 37(2), 494–536. https://doi.org/10.1519/jsc.0000000000004329
Ouyang, Z. G., Liu, F. Y., Zhai, G., & Bilan, S. (2020). Assessment of resident happiness under uncertainty of economic policies: Empirical evidences from China. Sustainability, 12(18), Article 7296. https://doi.org/10.3390/su12187296
Papadopoulou, S. K. K., Mantzorou, M., Voulgaridou, G., Pavlidou, E., Vadikolias, K., Antasouras, G., Vorvolakos, T., Psara, E., Vasios, G. K., Serdari, A., Poulios, E., & Giaginis, C. (2023). Nutritional status is associated with health-related quality of life, physical activity, and sleep quality: A cross-sectional study in an elderly Greek population. Nutrients, 15(2), Article 443. https://doi.org/10.3390/nu15020443
Pedras, S., Carvalho, R., & Graca Pereira, M. (2018). Predictors of quality of life in patients with diabetic foot ulcer: The role of anxiety, depression, and functionality. Journal of Health Psychology, 23(11), 1488–1498. https://doi.org/10.1177/1359105316656769
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903. https://doi.org/10.1037/0021-9010.88.5.879
Polat, H. T., & Serin, E. K. (2021). Self-esteem and sexual quality of life among obese women. Perspectives in Psychiatric Care, 57(3), 1083–1087. https://doi.org/10.1111/ppc.12660
Puciato, D., Rozpara, M., & Borysiuk, Z. (2018). Physical activity as a determinant of quality of life in working-age people in Wroclaw, Poland. International Journal of Environmental Research and Public Health, 15(4), Article 623. https://doi.org/10.3390/ijerph15040623
Qamar, Z., Alghamdi, A. M. S., Bin Haydarah, N. K., Balateef, A. A., Alamoudi, A. A., Abumismar, M. A., Shivakumar, S., Cicciù, M., & Minervini, G. (2023). Impact of temporomandibular disorders on oral health-related quality of life: A systematic review and meta-analysis. Journal of Oral Rehabilitation, 50(8), 706–714. https://doi.org/10.1111/joor.13472
Qiu, L., Gong, F., Wu, J., You, D., Zhao, Y., Xu, L., Cao, X., & Bao, F. (2022). Exercise interventions improved sleep quality through regulating intestinal microbiota composition. International Journal of Environmental Research and Public Health, 19(19), Article 12385. https://doi.org/10.3390/ijerph191912385
Rodrigues, F., Figueiredo, N., Jacinto, M., Monteiro, D., & Morouco, P. (2023). Social-cognitive theories to explain physical activity. Education Sciences, 13(2), Article 122. https://doi.org/10.3390/educsci13020122
Sanchez-Diaz, M., Rodriguez-Pozo, J. A., Latorre-Fuentes, J. M., Salazar-Nievas, M. C., Alejandro, M.-L., & Arias-Santiago, S. (2023). Sleep quality as a predictor of quality-of-life and emotional status impairment in patients with chronic spontaneous urticaria: A cross-sectional study. International Journal of Environmental Research and Public Health, 20(4). https://doi.org/10.3390/ijerph20043508
Sato, M., Jordan, J. S., & Funk, D. C. (2014). The role of physically active leisure for enhancing quality of life. Leisure Sciences, 36(3), 293–313. https://doi.org/10.1080/01490400.2014.886912
Schlenz, A. M., Thomas, S. J., Gloston, G., Lebensburger, J., Maxwell, S. L., & Kanter, J. (2022). Sleep quality and pain in adolescents and young adults with sickle cell disease. Journal of Clinical Sleep Medicine, 18(12), 2845–2853. https://doi.org/10.5664/jcsm.10240
Sejbuk, M., Mironczuk-Chodakowska, I., & Witkowska, A. M. (2022). Sleep quality: A narrative review on nutrition, stimulants, and physical activity as important factors. Nutrients, 14(9), Article 1912. https://doi.org/10.3390/nu14091912
Singh, B., Olds, T., Curtis, R., Dumuid, D., Virgara, R., Watson, A., Szeto, K., O'Connor, E., Ferguson, T., Eglitis, E., Miatke, A., Simpson, C. E., & Maher, C. (2023). Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. British Journal of Sports Medicine, 57(18). https://doi.org/10.1136/bjsports-2022-106195
Stafford, T. (2004). What good are positive emotions? Psychologist, 17(6), 331–331.
Su, W., & Xu, X. (2009). Reliability and Validity of a Computerized and Chinese Version of the International Physical Activity Questionnaire. [Icaie 2009: Proceedings of the 2009 international conference on artificial intelligence and education, vols 1 and 2]. International Conference on Artificial Intelligence and Education, Wuhan, PEOPLES R CHINA.
Tang, Y., Ma, Y., Zhang, J. in Wang, H. (2022). The relationship between negative life events and quality of life in adolescents: Mediated by resilience and social support [Article]. Frontiers in Public Health, 10, Article 980104. https://doi.org/10.3389/fpubh.2022.980104
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317–320. https://doi.org/10.1177/0020764020915212
Trihandini, I., Muhtar, M., Sakti, D. A. K., & Erlianti, C. P. (2023). The effect of long-haul COVID-19 toward domains of the health-related quality of life among recovered hospitalized patients. Frontiers in Public Health, 11, Article 1068127. https://doi.org/10.3389/fpubh.2023.1068127
Tseng, T.-H., Chen, H.-C., Wang, L.-Y., & Chien, M.-Y. (2020). Effects of exercise training on sleep quality and heart rate variability in middle-aged and older adults with poor sleep quality: a randomized controlled trial. Journal of Clinical Sleep Medicine, 16(9), 1483–1492. https://doi.org/10.5664/jcsm.8560
Wang, J., Wu, Y. L., Ning, F., Zhang, C. Y., & Zhang, D. F. (2017). The association between leisure-time physical activity and risk of undetected prediabetes. Journal of Diabetes Research, 2017, Article 4845108. https://doi.org/10.1155/2017/4845108
Werneck, A. O., Stubbs, B., Kandola, A., Oyeyemi, A. L., Schuch, F. B., Hamer, M., Vancampfort, D., & Silva, D. R. (2022). Prospective associations of leisure-time physical activity with psychological distress and well-being: A 12-year cohort study. Psychosomatic Medicine, 84(1), 116–122. https://doi.org/10.1097/psy.0000000000001023
White, R. L., Babic, M. J., Parker, P. D., Lubans, D. R., Astell-Burt, T., & Lonsdale, C. (2017). Domain-specific physical activity and mental health: A meta-analysis. American Journal of Preventive Medicine, 52(5), 653–666. https://doi.org/10.1016/j.amepre.2016.12.008
Wong, F. Y., Yang, L., Yuen, J. W. M., Chang, K. K. P., & Wong, F. K. Y. (2018). Assessing quality of life using WHOQOL-BREF: a cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. Bmc Public Health, 18, Article 1113. https://doi.org/10.1186/s12889-018-5942-3
Yayan, E. H., Zengin, M., Karabulut, Y. E., & Akinci, A. (2019). The relationship between the quality of life and depression levels of young people with type I diabetes. Perspectives in Psychiatric Care, 55(2), 291–299. https://doi.org/10.1111/ppc.12349
Yeom, J., & Yeom, I. (2023). Mediating effects of fatigue on the relationship between sleep quality and the quality of life of shift-working nurses. Chronobiology International, 40(4), 450–457. https://doi.org/10.1080/07420528.2023.2186130
Zambelli, Z., Halstead, E. J., Fidalgo, A. R., & Dimitriou, D. (2021). Good sleep quality improves the relationship between pain and depression among individuals with chronic pain. Frontiers in Psychology, 12, Article 668930. https://doi.org/10.3389/fpsyg.2021.668930
Zhang, J., Zheng, S., & Hu, Z. (2022a). The effect of physical exercise on depression in college students: The chain mediating role of self-concept and social support. Frontiers in Psychology, 13, Article 841160. https://doi.org/10.3389/fpsyg.2022.841160
Zhang, X., Gu, X., Zhang, T., & Keller, J. M. (2022b). The mediating roles of sleep quality and sedentary behavior between physical fitness and depression among female college freshmen. Journal of American College Health, 70(5), 1528–1535. https://doi.org/10.1080/07448481.2020.1809431
Zhang, Y., El Ghaziri, M., & De Castillero, E. R. (2023). Synergistic effect of self-efficacy and social support on regular participation in leisure-time physical activity among nursing staff. International Journal of Nursing Practice, 29(2), Article e13087. https://doi.org/10.1111/ijn.13087
Zhao, X. L., Lan, M. X., Li, H. X., & Yang, J. (2021). Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Medicine, 77, 339–345. https://doi.org/10.1016/j.sleep.2020.05.021
Zung, W. W. K. (1972). Depression status inventory - adjunct to self-rating depression scale. Journal of Clinical Psychology, 28(4), 539-&543. https://doi.org/10.1002/1097-4679(197210)28:4<539::Aid-jclp2270280427>3.0.Co;2-s
Funding
This study was conducted by the China Social Science Foundation Program (20BYT081) and Social Science Planning Research Project of Shandong Province (No. 22CTYJ09).
Author information
Authors and Affiliations
Contributions
Conceptualization: [Chengkai Feng, Zhenguo Shi]; Methodology: [Yuge Tian]; Formal analysis and investigation: [Chengkai Feng,Chao Ma]; Writing—original draft preparation: [Chengkai Feng]; Writing—review and editing: [Jianmin Liu].
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of Shandong University (2021-R-001). Participants were aware that they could withdraw at any time.
Consent to participate
The study was conducted in accordance with the Declaration of Helsinki and informed consent was obtained from all subjects and/or their legal guardians.
Consent for publication
Not applicable
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, C., Shi, Z., Tian, Y. et al. A study of the relationship between leisure-time physical activity and residents’ quality of life. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-05990-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s12144-024-05990-x