Abstract
Objectives
To develop and validate the 4-year risk of type 2 diabetes mellitus among adults with metabolic syndrome.
Design
Retrospective cohort study of a large multicenter cohort with broad validation.
Settings
The derivation cohort was from 32 sites in China and the geographic validation cohort was from Henan population-based cohort study.
Results
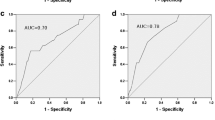
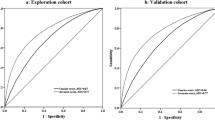
568 (17.63) and 53 (18.67%) participants diagnosed diabetes during 4-year follow-up in the develo** and validation cohort, separately. Age, gender, body mass index, diastolic blood pressure, fasting plasma glucose and alanine aminotransferase were included in the final model. The area under curve for the training and external validation cohort was 0.824 (95% CI, 0.759–0.889) and 0.732 (95% CI, 0.594–0.871), respectively. Both the internal and external validation have good calibration plot. A nomogram was constructed to predict the probability of diabetes during 4-year follow-up, and on online calculator is also available for a more convenient usage (https://lucky0708.shinyapps.io/dynnomapp/).
Conclusion
We developed a simple diagnostic model to predict 4-year risk of type 2 diabetes mellitus among adults with metabolic syndrome, which is also available as web-based tools (https://lucky0708.shinyapps.io/dynnomapp/).





Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available in the DRYAD database repository, for the derivation cohort can be downloaded from https://doi.org/10.5061/dryad.ft8750v, and for the validation part can be downloaded from https://datadryad.org/stash/share/HNXtM6qk-4uSRGSP90XkBKzIi818a4R40i5EWblEog0.
References
Mortality, G.B.D. and C. Causes of Death, Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385(9963), 117–171 (2015)
Y. Zheng, S.H. Ley, F.B. Hu, Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14(2), 88–98 (2018)
American Diabetes Association, 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43(Suppl 1), S14–S31 (2020)
L. Wang et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317(24), 2515–2523 (2017)
S.H. Yang, K.F. Dou, W.J. Song, Prevalence of diabetes among men and women in China. N. Engl. J. Med. 362(25), 2425–2426 (2010).
Diabetes Prevention Program Research Group, Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 3(11), 866–875 (2015)
J. Lindstrom et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 368(9548), 1673–1679 (2006)
Q. Gong et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol. 7(6), 452–461 (2019)
W.H. Herman et al. Impact of lifestyle and metformin interventions on the risk of progression to diabetes and regression to normal glucose regulation in overweight or obese people with impaired glucose regulation. Diabetes Care 40(12), 1668–1677 (2017)
M.G. Saklayen, The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 20(2), 12 (2018)
P. Ranasinghe et al. Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: a systematic review. BMC Public Health 17(1), 101 (2017)
Z. Gu et al. Obesity and lipid-related parameters for predicting metabolic syndrome in Chinese elderly population. Lipids Health Dis. 17(1), 289 (2018)
E. Muzurovic, D.P. Mikhailidis, C. Mantzoros, Non-alcoholic fatty liver disease, insulin resistance, metabolic syndrome and their association with vascular risk. Metabolism 119, 154770 (2021)
N.C. do Vale Moreira et al. Prevalence of Metabolic Syndrome by different definitions, and its association with type 2 diabetes, pre-diabetes, and cardiovascular disease risk in Brazil. Diabetes Metab. Syndr. 14(5), 1217–1224 (2020)
Y. Chen et al. Association of body mass index and age with incident diabetes in Chinese adults: a population-based cohort study. BMJ Open 8(9), e021768 (2018)
J. Lu et al. Predictive value of fasting glucose, postload glucose, and hemoglobin A1c on risk of diabetes and complications in Chinese adults. Diabetes Care 42(8), 1539–1548 (2019)
T. Wang et al. Ideal cardiovascular health metrics and major cardiovascular events in patients with prediabetes and diabetes. JAMA Cardiol. 4(9), 874–883 (2019)
C. Chen, F.C. Lu; P.R.C. Department of Disease Control Ministry of Health, The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. 17(Suppl), 1–36 (2004)
Chinese Preventive Medicine, Association et al., [Chinese guideline on healthy lifestyle to prevent cardiometabolic diseases]. Zhonghua Yu Fang Yi Xue Za Zhi 54(3), 256–277 (2020)
American Diabetes, A., Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1), S62–9 (2010)
G.S. Collins et al. Transparent reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): the TRIPOD Statement. Br. J. Surg. 102(3), 148–158 (2015)
P. Lunde et al. The effectiveness of smartphone apps for lifestyle improvement in noncommunicable diseases: systematic review and meta-analyses. J. Med. Internet Res. 20(5), e162 (2018)
S. Chatterjee, K. Khunti, M.J. Davies, Type 2 diabetes. Lancet 389(10085), 2239–2251 (2017)
R.A. DeFronzo et al. Type 2 diabetes mellitus. Nat. Rev. Dis. Prim. 1, 15019 (2015)
U. Galicia-Garcia et al. Pathophysiology of type 2 diabetes mellitus. Int J. Mol. Sci. 21, 17 (2020)
Z.T. Bloomgarden, Dyslipidemia and the metabolic syndrome. Diabetes Care 27(12), 3009–3016 (2004)
J. Beulens et al. Risk and management of pre-diabetes. Eur. J. Prev. Cardiol. 26(2_suppl), 47–54 (2019)
R. Williams et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin. Pract. 162, 108072 (2020)
T. Xu et al. A nomogram model for the risk prediction of type 2 diabetes in healthy eastern China residents: a 14-year retrospective cohort study from 15,166 participants. EPMA J. 13(3), 397–405 (2022)
K. Wang et al. Nomogram prediction for the 3-year risk of type 2 diabetes in healthy mainland China residents. EPMA J. 10(3), 227–237 (2019)
K. Liang et al. Nomogram predicting the risk of progression from prediabetes to diabetes after a 3-year follow-up in chinese adults. Diabetes Metab. Syndr. Obes. 14, 2641–2649 (2021)
Y. Han et al. Nomogram model and risk score to predict 5-year risk of progression from prediabetes to diabetes in Chinese adults: development and validation of a novel model. Diabetes Obes. Metab. 25(3), 675–687 (2023)
Q. Liu et al. Development and validation of a nomogram to predict type 2 diabetes mellitus in overweight and obese adults: a prospective cohort study from 82938 adults in China. Int J. Endocrinol. 2020, 8899556 (2020)
R.H. Eckel et al. The metabolic syndrome. Lancet 375(9710), 181–183 (2010)
B.M. Cheung et al. Development of diabetes in Chinese with the metabolic syndrome: a 6-year prospective study. Diabetes Care 30(6), 1430–1436 (2007)
C. Ding et al. The associations of metabolic syndrome with incident hypertension, type 2 diabetes mellitus and chronic kidney disease: a cohort study. Endocrine 60(2), 282–291 (2018)
C.M. Ferrara, A.P. Goldberg, Limited value of the homeostasis model assessment to predict insulin resistance in older men with impaired glucose tolerance. Diabetes Care 24(2), 245–249 (2001)
M. Ng et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945), 766–781 (2014)
M.L. Power, J. Schulkin, Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br. J. Nutr. 99(5), 931–940 (2008)
M.F. Yao et al. Gender differences in risks of coronary heart disease and stroke in patients with type 2 diabetes mellitus and their association with metabolic syndrome in China. Int J. Endocrinol. 2016, 8483405 (2016)
A. Vaiserman, O. Lushchak, Developmental origins of type 2 diabetes: focus on epigenetics. Ageing Res Rev. 55, 100957 (2019)
C. Aguayo-Mazzucato et al. Acceleration of beta cell aging determines diabetes and senolysis improves disease outcomes. Cell Metab. 30(1), 129–142.e4 (2019)
P. Muntner et al. Comparison of the Framingham Heart Study hypertension model with blood pressure alone in the prediction of risk of hypertension: the Multi-Ethnic Study of Atherosclerosis. Hypertension 55(6), 1339–1345 (2010)
S.S. Mahmood et al. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet 383(9921), 999–1008 (2014)
C.E. Ruhl, J.E. Everhart, Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology 124(1), 71–79 (2003)
R. Wejstal et al. Persistent alanine aminotransferase elevation in healthy Swedish blood donors–mainly caused by obesity. Vox Sang. 55(3), 152–156 (1988)
L.S. Friedman et al. Evaluation of blood donors with elevated serum alanine aminotransferase levels. Ann. Intern. Med. 107(2), 137–144 (1987)
R.K. Schindhelm et al. Alanine aminotransferase as a marker of non-alcoholic fatty liver disease in relation to type 2 diabetes mellitus and cardiovascular disease. Diabetes Metab. Res Rev. 22(6), 437–443 (2006)
J. Westerbacka et al. Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia 47(8), 1360–1369 (2004)
Acknowledgements
The authors would like to thank Dr. Jiayi Yi, National Clinical Research Center for Cardiovascular Diseases, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, National Center for Cardiovascular Diseases, Bei**g, China, and Dr. Zhongheng Zhang, Department of Emergency Medicine, Sir Run-Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou 310016, China, for their advice on the study design.
Author contributions
Design: T.Y.; J.W.; L.W.; Gu.Q.; Y.Z.; Data collection: T.Y.; N.J.; M.P.; Analysis: T.Y.; F.G.; F.H.; Y.Song; Y.Z.; Writing manuscript: T.Y.; Y.Z.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the National Natural Science Foundation of China (U2004116, 81800734), the National Key Research and Development Program of China (2017YFC1309800) and the Key Project of Medical Science and Technology of Henan Province (SB201901046).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
The Rich Healthcare Group Review Board examined and granted approval for the investigations using human subjects in the derivation cohort. In compliance with national law and institutional standards, written informed permission was not needed for participation in this study. Additionally, the Ethical Review Committee of Rui** Hospital reviewed and authorized the human participants in the broad validation cohort (RUIJIN-2011-14). To take part in this study, the patients/participants gave their written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, T., Wang, J., Wu, L. et al. Development and validation of a nomogram to estimate future risk of type 2 diabetes mellitus in adults with metabolic syndrome: prospective cohort study. Endocrine 80, 336–345 (2023). https://doi.org/10.1007/s12020-023-03329-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03329-3