Abstract
Purpose of Review
Preclinical evidence indicates progesterone and estrogen influence drug-taking behaviors, including nicotine/tobacco. However, clinical research on this relationship is less clear. This lack of clarity may be due to measuring naturally occurring endogenous hormones to examine this relationship, which introduces substantial error. Therefore, the goal of this review is to examine the link between the delivery of exogenous hormones and cigarette smoking-related behavior.
Recent Findings
Exogenous progesterone may have favorable effects on cognition, symptomatology, consumption, and smoking cessation. Hormonal replacement therapy does not have a clear relationship with smoking-related behaviors. Oral contraceptive use may have adverse effects on stress response, nicotine metabolism, and symptomatology.
Summary
Additional research is needed to explore how the administration of exogenous hormones may (a) strengthen research methodology on this topic, (b) enhance our understanding of the role of progesterone/estrogen on smoking-related behaviors, and (c) improve smoking cessation outcomes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
United States Department of Health and Human Services. (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. A Rep Surg Gen. 1081.
WHO | WHO report on the global tobacco epidemic 2017. WHO [Internet]. 2019 [cited 2020 Jul 28]; Available from: http://www.who.int/tobacco/global_report/2017/en/
Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med [Internet]. 2013 Jan 24 [cited 2020 Jul 28];368(4):341–50. Available from: http://www.nejm.org/doi/10.1056/NEJMsa1211128
Lynch WJ, Sofuoglu M. Role of progesterone in nicotine addiction: evidence from initiation to relapse. Exp Clin Psychopharmacol. 2010 Dec;18(6):451–61.
Anker JJ, Carroll ME. The role of progestins in the behavioral effects of cocaine and other drugs of abuse: human and animal research. Neurosci Biobehav Rev. 2010 Nov;35(2):315–33.
Carroll ME, Lynch WJ, Roth ME, Morgan AD, Cosgrove KP. (2004) Sex and estrogen influence drug abuse. Trends Pharmacol Sci [Internet]. 1 [cited 2018 Nov 26];25(5):273–9. Available from: https://www.sciencedirect.com/science/article/pii/S0165614704000914
Carroll ME, Anker JJ. Sex differences and ovarian hormones in animal models of drug dependence. Horm Behav. 2010 Jun;58(1):44–56.
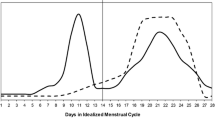
Weinberger AH, Smith PH, Allen SS, Cosgrove KP, Saladin ME, Gray KM, et al. Systematic and meta-analytic review of research examining the impact of menstrual cycle phase and ovarian hormones on smoking and cessation. Nicotine Tob Res. 2015 Apr;17(4):407–21.
Wetherill RR, Franklin TR, Allen SS. Ovarian hormones, menstrual cycle phase, and smoking: a review with recommendations for future studies. Curr Addict Reports [Internet]. 2016;3(1):1–8. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medp&AN=27134810https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:27134810&id=doi:10.1007%2Fs40429-016-0093-z&issn=2196-2952&isbn=&volume=3&issu.
Allen AM, McRae-Clark AL, Carlson S, Saladin ME, Gray KM, Wetherington CL, et al. Determining menstrual phase in human biobehavioral research: a review with recommendations. Exp Clin Psychopharmacol 2015 Nov
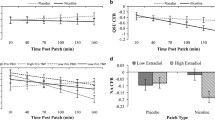
Allen S, Petersen A, Harrison K, Tosun N, Cameron J. Response to nicotine following overnight smoking abstinence during short-term progesterone treatment in women. Exp Clin Psychopharmacol [Internet]. 2019;29:29. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medp&AN=31464476https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:31464476&id=doi:10.1037%2Fpha0000312&issn=1064-1297&isbn=&volume=&issue=&spage.
• Harrison K, Petersen A, Tosun N, Crist K, Allen AM, Allene S. Effect of exogenous progesterone administration on cigarette smoking-related symptomology in oral contraceptive users who smoke. Addict Behav. 2020 1;102. This article uses a randomized double-blind cross-over tiral to examine the effect of exogenous progesterone treatment on smoking-related symptomatology during acute abstinence.
Sofuoglu M, Babb DA, Hatsukami DK. (2018 ) Progesterone treatment during the early follicular phase of the menstrual cycle: effects on smoking behavior in women. Pharmacol Biochem Behav [Internet]. [cited 5];69(1–2):299–304. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11420098.
Sofuoglu M, Mitchell E, Mooney M. Progesterone effects on subjective and physiological responses to intravenous nicotine in male and female smokers. Hum Psychopharmacol. 2009;24(7):559–64.
Sofuoglu M, Mouratidis M, Mooney M. Progesterone improves cognitive performance and attenuates smoking urges in abstinent smokers. Psychoneuroendocrinology [Internet]. 2011 Jan [cited 2018 Mar 5];36(1):123–32. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0306453010001733
Allen A, Petersen A, Harrison K, Nair U, Allen S. Effect of exogenous progesterone administration on smoking topography. Addict Behav [Internet]. 2020 Jul 22 [cited 2020 Jul 28];106570. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0306460320307000
• Allen SS, Allen AM, Lunos S, Tosun N (2016) Progesterone and postpartum smoking relapse: a pilot double-blind placebo-controlled randomized trial. Nicotine Tob Res. Aug;18: 2145–2153. This article uses a randomized double-blind control trial to examine the effect of exogenous progesterone treatment on postpartum smoking relapse.
Allen A, Tosun N, Carlson S, Allen S (2018) Postpartum changes in mood and smoking-related symptomatology: an ecological momentary assessment investigation. Nicotine Tob Res. 20(6).
• Forray A, Gilstad-Hayden K, Suppies C, Bogen D, Sofuoglu M, Yonkers KA (2019) Progesterone for smoking relapse prevention following delivery: a pilot, randomized, double-blind study. Psychoneuroendocrinology [Internet]. 2017 Dec [cited 2019 May 6];86:96–103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28926762This article uses a randomized double-blind control trial to examine the effect of exogenous progesterone treatment on postpartum smoking relapse.
• Tosun NL, Fieberg AM, Eberly LE, Harrison KA, Tipp AR, Allen AM, et al. (2019) Exogenous progesterone for smoking cessation in men and women: a pilot double-blind, placebo-controlled randomized clinical trial. Addiction [Internet]. 2019 May 6 [cited 2019 May 29];add.14645. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31059177This article uses a randomized double-blind control trial to examine the effect of exogenous progesterone treatment on smoking cessation in men and women.
Allen AM, Friedrichsen SC, Petersen N, Allen SS (2019) Subjective response to intranasal nicotine administration in oral contraceptive users and naturally-cycling women. Addict Behav [Internet]. 98:106043. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=prem&AN=31310925https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:31310925&id=doi:10.1016%2Fj.addbeh.2019.106043&issn=0306-4603&isbn=&volume=98&.
Allen SS, Brintnell DM, Hatsukami D, Reich B. Energy intake and physical activity during short-term smoking cessation in postmenopausal women. Addict Behav [Internet]. 2004;29(5):947–51. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L38822951. https://doi.org/10.1016/j.addbeh.2004.02.041.
Allen SS, Hatsukami D, Brintnell DM, Bade T. Effect of nicotine replacement therapy on post-cessation weight gain and nutrient intake: a randomized controlled trial of postmenopausal female smokers. Addict Behav [Internet]. 2005;30(7):1273–80. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L40967016. https://doi.org/10.1016/j.addbeh.2005.01.003.
Allen SS, Hatsukami DK, Christianson D (2003) Nicotine withdrawal and depressive symptomatology during short-term smoking abstinence: a comparison of postmenopausal women using and not using hormone replacement therapy. Nicotine Tob Res [Internet]. 5(1):49–59. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med5&AN=12745506https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:12745506&id=doi:10.1080%2F14622200307264&issn=1462-2203&isbn=&volume=5&issue=1.
Allen SS, Hatsukami DK, Bade T, Center B (2004) Transdermal nicotine use in postmenopausal women: does the treatment efficacy differ in women using and not using hormone replacement therapy? Nicotine Tob Res [Internet]. 6(5):777–88. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med5&AN=15700913https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:15700913&id=doi:10.1080%2F1462220042000274239&issn=1462-2203&isbn=&volume=6&is.
• Chenoweth MJ, Novalen M, Hawk LW, Schnoll RA, George TP, Cinciripini PM, et al. (2014) Known and novel sources of variability in the nicotine metabolite ratio in a large sample of treatment-seeking smokers. Cancer Epidemiol Prev Biomarkers. This article identifies both HRT and OC as modifiers of nioctine metabolism ratio.
Hall KS, Trussell J. Types of combined oral contraceptives used by US women. Contraception. 2012 Dec;86(6):659–65.
Montoya ER, Bos PA (2017) How oral contraceptives impact social-emotional behavior and brain function. Trends Cogn Sci [Internet]. [cited 2019 Mar 26];21(2):125–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28089524.
Allen AM, Weinberger AH, Wetherill RR, Howe CL, McKee SA (2019) Oral contraceptives and cigarette smoking: a review of the literature and future directions. Nicotine Tob Res [Internet]. 21(5):592–601. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=29165663https://arizona-primo.hosted.exlibrisgroup.com/openurl/01UA/01UA? sid=OVID:medline&id=pmid:29165663&id=doi:10.1093%2Fntr%2Fntx258&issn=1462-2203&isbn=&volume=21&issue=5&.
• Allen AM, Carlson S, Eberly LE, Hatsukami D, Piper ME (2018) Use of hormonal contraceptives and smoking cessation: a preliminary report. Addict Behav [Internet]. [cited 2017 Sep 5];76:236–42. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0306460317302927This article is the first to examine smoking cessation rates by use of oral contraceptives.
Allen SS, Allen AM, Pomerleau CS. Influence of phase-related variability in premenstrual symptomatology, mood, smoking withdrawal, and smoking behavior during ad libitum smoking, on smoking cessation outcome. Addict Behav. 2009 Jan;34(1):107–11.
Schiller CE, Saladin ME, Gray KM, Hartwell KJ, Carpenter MJ. Association between ovarian hormones and smoking behavior in women. Exp Clin Psychopharmacol. 2012 Aug;20(4):251–7.
Lynch WJ, Roth ME, Carroll ME. Biological basis of sex differences in drug abuse: preclinical and clinical studies. Psychopharmacology. 2002 Nov;164(2):121–37.
Weinberger AH, Smith PH, Allen SS, Cosgrove KP, Saladin ME, Gray KM, et al. Systematic and meta-analytic review of research examining the impact of menstrual cycle phase and ovarian hormones on smoking and cessation. Nicotine Tob Res. 2015 Apr;17(4):407–21.
Drug Result Page - MICROMEDEX [Internet]. [cited 2019 Oct 25]. Available from: https://www.micromedexsolutions.com/micromedex2/librarian/CS/1395A6/ND_PR/evidencexpert/ND_P/evidencexpert/DUPLICATIONSHIELDSYNC/19A6CC/ND_PG/evidencexpert/ND_B/evidencexpert/ND_AppProduct/evidencexpert/ND_T/evidencexpert/PFActionId/evidencexpert.GoToDashboard?docId=486020&contentSetId=100&title=Progesterone&servicesTitle=Progesterone&brandName=Prometrium#.
Hydroxyprogesterone caproate injection USP.
Krop J, Kramer WG (2017) Comparative bioavailability of hydroxyprogesterone caproate administered via intramuscular injection or subcutaneous autoinjector in healthy postmenopausal women: a randomized, parallel group, open-label study. Clin Ther [Internet]. Dec 1 [cited 2020 Jul 29];39(12):2345–54. Available from: https://doi.org/10.1016/j.clinthera.2017.10.020.
Mishell DR (1996) Pharmacokinetics of depot medroxyprogesterone acetate contraception. J Reprod Med [Internet]. [cited 2018 Dec 10];41(5 Suppl):381–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8725700.
Frederiksen MC. Depot medroxyprogesterone acetate contraception in women with medical problems. J Reprod Med [Internet]. 1996 May [cited 2019 Nov 11];41(5 Suppl):414–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8725704.
Halderman LD, Nelson AL. Impact of early postpartum administration of progestin-only hormonal contraceptives compared with nonhormonal contraceptives on short-term breast-feeding patterns. Am J Obstet Gynecol. 2002;186(6):1250–8.
Chaudhri R, Rizvi F, Afzal M (2009) Body weight and bleeding pattern changes in women using DMPA-SC. J Coll Physicians Surg Pak [Internet]. [cited 2019 Apr 5];19(10):618–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19811711.
Peltier MKR, Sofuoglu M (2018) Role of exogenous progesterone in the treatment of men and women with substance use disorders: a narrative review. Vol. 32, CNS Drugs. Springer International Publishing; p. 421–35.
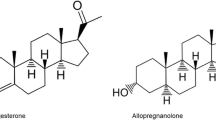
Allen AM, Al’Absi M, Lando H, Allen SS (2015) Allopregnanolone association with psychophysiological and cognitive functions during acute smoking abstinence in premenopausal women. Exp Clin Psychopharmacol. 23(1)
Allen AM, al’Absi M, Lando H, Hatsukami D, Allen SS (2013) Menstrual phase, depressive symptoms, and allopregnanolone during short-term smoking cessation. Exp Clin Psychopharmacol. 21(6).
Allen AM (2012) Allopregnanolone during short-term smoking abstinence: associations with depressive symptoms, smoking-related symptomatology and nicotine response
Meltzer-Brody S, Kanes SJ (2020) Allopregnanolone in postpartum depression: role in pathophysiology and treatment [Internet]. Vol. 12, Neurobiology of Stress. Elsevier Inc; [cited 2020 Jul 29]. Available from: https://pubmed.ncbi.nlm.nih.gov/32435663/
Tufano M, Pinna G (2020) Is there a future for PPARs in the treatment of neuropsychiatric disorders? [Internet]. Vol. 25, Molecules. MDPI AG; [cited 2020 Jul 29]. Available from: https://pubmed.ncbi.nlm.nih.gov/32120979/
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reproductive Psychiatry and Women’s Health
Rights and permissions
About this article
Cite this article
Allen, A., Mallahan, S., Ortega, A. et al. Administration of Exogenous Hormones and the Implications for Cigarette Smoking-Related Behaviors. Curr Psychiatry Rep 22, 70 (2020). https://doi.org/10.1007/s11920-020-01197-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11920-020-01197-6