Abstract
Purpose of Review
There has been an increased prevalence of allergy. Due to this relatively rapid rise, changes in environmental exposures are likely the main contributor. In this review, we highlight literature from the last 3 years pertaining to the role of air pollution, greenness, and the rural/farm lifestyle and their association with the development of allergic sensitization, atopic dermatitis, food allergy, and allergic rhinitis in infancy and childhood. Because asthma has a more complex pathophysiology, it was excluded from this review.
Recent Findings
Recent studies support a role for air pollution, greenness, and rural/farming lifestyle influencing atopic outcomes that continue to be defined. While many studies have examined singular environmental exposures, the interconnectedness of these exposures and others points to a need for future work to consider an individual’s whole exposure.
Summary
Environmental exposures’ influence on atopic disease development remains an ongoing and important area of study.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(Suppl 1):8–16.
Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet (London, England). 2006;368(9537):733–43.
Loh W, Tang MLK. The epidemiology of food allergy in the global context. Int J Environ Res Public Health. 2018;15(9).
Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J Allergy Clin Immunol. 2011;127(3):668-76.e1-2.
Aït-Khaled N, Pearce N, Anderson HR, Ellwood P, Montefort S, Shah J. Global map of the prevalence of symptoms of rhinoconjunctivitis in children: The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three. Allergy. 2009;64(1):123–48.
Hill DA, Spergel JM. The atopic march: critical evidence and clinical relevance. Ann Allergy Asthma Immunol. 2018;120(2):131–7.
Papapostolou N, Xepapadaki P, Gregoriou S, Makris M. Atopic dermatitis and food allergy: a complex interplay what we know and what we would like to learn. J Clin Med. 2022;11(14).
Eigenmann PA, Calza AM. Diagnosis of IgE-mediated food allergy among Swiss children with atopic dermatitis. Pediatr Allergy Immunol. 2000;11(2):95–100.
Hill DA, Grundmeier RW, Ram G, Spergel JM. The epidemiologic characteristics of healthcare provider-diagnosed eczema, asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 2016;16:133.
Gustafsson D, Sjöberg O, Foucard T. Development of allergies and asthma in infants and young children with atopic dermatitis–a prospective follow-up to 7 years of age. Allergy. 2000;55(3):240–5.
Brough HA, Nadeau KC, Sindher SB, Alkotob SS, Chan S, Bahnson HT, et al. Epicutaneous sensitization in the development of food allergy: what is the evidence and how can this be prevented? Allergy. 2020;75(9):2185–205.
Martin PE, Eckert JK, Koplin JJ, Lowe AJ, Gurrin LC, Dharmage SC, et al. Which infants with eczema are at risk of food allergy? Results from a population-based cohort. Clin Exp Allergy. 2015;45(1):255–64.
Gray CL, Levin ME, du Toit G. Egg sensitization, allergy and component patterns in African children with atopic dermatitis. Pediatr Allergy Immunol. 2016;27(7):709–15.
Palmer DJ, Metcalfe J, Makrides M, Gold MS, Quinn P, West CE, et al. Early regular egg exposure in infants with eczema: a randomized controlled trial. J Allergy Clin Immunol. 2013;132(2):387-92.e1.
Brough HA, Liu AH, Sicherer S, Makinson K, Douiri A, Brown SJ, et al. Atopic dermatitis increases the effect of exposure to peanut antigen in dust on peanut sensitization and likely peanut allergy. J Allergy Clin Immunol. 2015;135(1):164–70.
Sweeney A, Sampath V, Nadeau KC. Early intervention of atopic dermatitis as a preventive strategy for progression of food allergy. Allergy Asthma Clin Immunol. 2021;17(1):30.
Kader HA, Azeem M, Jwayed SA, Al-Shehhi A, Tabassum A, Ayoub MA, et al. Current insights into immunology and novel therapeutics of atopic dermatitis. Cells. 2021;10(6).
Hon KLE, Chan VPY, Leung AKC. Experimental drugs with the potential to treat atopic eczema. J Exp Pharmacol. 2021;13:487–98.
Dantzer JA, Wood RA. Next-generation approaches for the treatment of food allergy. Curr Allergy Asthma Rep. 2019;19(1):5.
Apfelbacher CJ, Diepgen TL, Schmitt J. Determinants of eczema: population-based cross-sectional study in Germany. Allergy. 2011;66(2):206–13.
Wadonda-Kabondo N, Sterne JA, Golding J, Kennedy CT, Archer CB, Dunnill MG. Association of parental eczema, hayfever, and asthma with atopic dermatitis in infancy: birth cohort study. Arch Dis Child. 2004;89(10):917–21.
Tsai HJ, Kumar R, Pongracic J, Liu X, Story R, Yu Y, et al. Familial aggregation of food allergy and sensitization to food allergens: a family-based study. Clin Exp Allergy. 2009;39(1):101–9.
Hatzler L, Panetta V, Illi S, Hofmaier S, Rohrbach A, Hakimeh D, et al. Parental hay fever reinforces IgE to pollen as pre-clinical biomarker of hay fever in childhood. Pediatr Allergy Immunol. 2014;25(4):366–73.
Schultz LF. Atopic dermatitis: a genetic-epidemiologic study in a population-based twin sample. J Am Acad Dermatol. 1993;28(5 Pt 1):719–23.
Liu X, Zhang S, Tsai HJ, Hong X, Wang B, Fang Y, et al. Genetic and environmental contributions to allergen sensitization in a Chinese twin study. Clin Exp Allergy. 2009;39(7):991–8.
Sicherer SH, Furlong TJ, Maes HH, Desnick RJ, Sampson HA, Gelb BD. Genetics of peanut allergy: a twin study. J Allergy Clin Immunol. 2000;106(1 Pt 1):53–6.
van Beijsterveldt CE, Boomsma DI. Genetics of parentally reported asthma, eczema and rhinitis in 5-yr-old twins. Eur Respir J. 2007;29(3):516–21.
Kanchan K, Clay S, Irizar H, Bunyavanich S, Mathias RA. Current insights into the genetics of food allergy. J Allergy Clin Immunol. 2021;147(1):15–28.
Johansson E, Mersha TB. Genetics of food allergy. Immunol Allergy Clin North Am. 2021;41(2):301–19.
Al-Shobaili HA, Ahmed AA, Alnomair N, Alobead ZA, Rasheed Z. Molecular genetic of atopic dermatitis: an update. Int J Health Sci. 2016;10(1):96–120.
Gupta J, Johansson E, Bernstein JA, Chakraborty R, Khurana Hershey GK, Rothenberg ME, et al. Resolving the etiology of atopic disorders by using genetic analysis of racial ancestry. J Allergy Clin Immunol. 2016;138(3):676–99.
Choi BY, Han M, Kwak JW, Kim TH. Genetics and epigenetics in allergic rhinitis. Genes. 2021;12(12).
Moore M, Gould P, Keary BS. Global urbanization and impact on health. Int J Hyg Environ Health. 2003;206(4–5):269–78.
Alkotob SS, Cannedy C, Harter K, Movassagh H, Paudel B, Prunicki M, et al. Advances and novel developments in environmental influences on the development of atopic diseases. Allergy. 2020;75(12):3077–86.
Cecchi L, D’Amato G, Annesi-Maesano I. External exposome and allergic respiratory and skin diseases. J Allergy Clin Immunol. 2018;141(3):846–57.
Gallant MJ, Ellis AK. Prenatal and early-life exposure to indoor air-polluting factors and allergic sensitization at 2 years of age. Ann Allergy Asthma Immunol. 2020;124(3):283–7.
Wang C, Wei CC, Wan L, Lin CL, Tsai JD. Association of exposure to hydrocarbon air pollution with the incidence of atopic dermatitis in children. Ital J Pediatr. 2021;47(1):202.
Salvi S. Health effects of ambient air pollution in children. Paediatr Respir Rev. 2007;8(4):275–80.
Park TH, Park S, Cho MK, Kim S. Associations of particulate matter with atopic dermatitis and chronic inflammatory skin diseases in South Korea. Clin Exp Dermatol. 2022;47(2):325–34.
Hendricks AJ, Eichenfield LF, Shi VY. The impact of airborne pollution on atopic dermatitis: a literature review. Br J Dermatol. 2020;183(1):16–23.
Rushton L. Health impact of environmental tobacco smoke in the horne. Rev Environ Health. 2021;19(3–4):291–310.
Peters RL, Mavoa S, Koplin JJ. An overview of environmental risk factors for food allergy. Int J Environ Res Public Health. 2022;19(2).
•• Yao TC, Huang HY, Pan WC, Wu CY, Tsai SY, Hung CY, et al. Association of prenatal exposure to fine particulate matter pollution with childhood eczema. Allergy. 2021;76(7):2241–5. COMMENT: Identified a sensitive prenatal window for exposure to PM and found a lower threshold for the negative effects of PM2.5.
Sbihi H, Boutin RC, Cutler C, Suen M, Finlay BB, Turvey SE. Thinking bigger: how early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease. Allergy. 2019;74(11):2103–15.
Dijkhoff IM, Drasler B, Karakocak BB, Petri-Fink A, Valacchi G, Eeman M, et al. Impact of airborne particulate matter on skin: a systematic review from epidemiology to in vitro studies. Part Fibre Toxicol. 2020;17(1):35.
**an M, Ma S, Wang K, Lou H, Wang Y, Zhang L, et al. Particulate matter 2.5 causes deficiency in barrier integrity in human nasal epithelial cells. Allergy Asthma Immunol Res. 2020;12(1):56–71.
Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Krämer U, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008;177(12):1331–7.
Kantor R, Kim A, Thyssen JP, Silverberg JI. Association of atopic dermatitis with smoking: a systematic review and meta-analysis. J Am Acad Dermatol. 2016;75(6):1119-25.e1.
Thacher JD, Gruzieva O, Pershagen G, Neuman Å, Wickman M, Kull I, et al. Pre- and postnatal exposure to parental smoking and allergic disease through adolescence. Pediatrics. 2014;134(3):428–34.
Thacher JD, Gruzieva O, Pershagen G, Neuman Å, van Hage M, Wickman M, et al. Parental smoking and development of allergic sensitization from birth to adolescence. Allergy. 2016;71(2):239–48.
Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007;29(5):879–88.
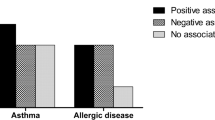
Gruzieva O, Gehring U, Aalberse R, Agius R, Beelen R, Behrendt H, et al. Meta-analysis of air pollution exposure association with allergic sensitization in European birth cohorts. J Allergy Clin Immunol. 2014;133(3):767-76.e7.
Melén E, Standl M, Gehring U, Altug H, Antó JM, Berdel D, et al. Air pollution and IgE sensitization in 4 European birth cohorts-the MeDALL project. J Allergy Clin Immunol. 2021;147(2):713–22.
Saulyte J, Regueira C, Montes-Martínez A, Khudyakov P, Takkouche B. Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: a systematic review and meta-analysis. PLoS Med. 2014;11(3):e1001611.
•• Kim YM, Kim J, Ha SC, Ahn K. Effects of exposure to indoor fine particulate matter on atopic dermatitis in children. Int J Environ Res Public Health. 2021;18(21). COMMENT: Examined the effect of indoor concentration of PM, which is not as commonly studied as outdoor PM.
Granum B, Oftedal B, Agier L, Siroux V, Bird P, Casas M, et al. Multiple environmental exposures in early-life and allergy-related outcomes in childhood. Environ Int. 2020;144:106038.
To T, Zhu J, Stieb D, Gray N, Fong I, Pinault L, et al. Early life exposure to air pollution and incidence of childhood asthma, allergic rhinitis and eczema. Eur Respir J. 2020;55(2).
Wang H, Li XB, Chu XJ, Cao NW, Wu H, Huang RG, et al. Ambient air pollutants increase the risk of immunoglobulin E-mediated allergic diseases: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2022:1–19.
Min KD, Yi SJ, Kim HC, Leem JH, Kwon HJ, Hong S, et al. Association between exposure to traffic-related air pollution and pediatric allergic diseases based on modeled air pollution concentrations and traffic measures in Seoul, Korea: a comparative analysis. Environ Health. 2020;19(1):6.
Silverberg JI, Hanifin J, Simpson EL. Climatic factors are associated with childhood eczema prevalence in the United States. J Invest Dermatol. 2013;133(7):1752–9.
Noh SR, Kim JS, Kim EH, Jeon BH, Kim JH, Kim YM, et al. Spectrum of susceptibility to air quality and weather in individual children with atopic dermatitis. Pediatr Allergy Immunol. 2019;30(2):179–87.
Ye C, Gu H, Li M, Chen R, **ao X, Zou Y. Air pollution and weather conditions are associated with daily outpatient visits of atopic dermatitis in Shanghai, China. Dermatology (Basel, Switzerland). 2022:1–11.
Hu Y, Jiang F, Tan J, Liu S, Li S, Wu M, et al. Environmental exposure and childhood atopic dermatitis in Shanghai: a season-stratified time-series analysis. Dermatology (Basel, Switzerland). 2022;238(1):101–8.
Kuiper IN, Markevych I, Accordini S, Bertelsen RJ, Bråbäck L, Christensen JH, et al. Associations of preconception exposure to air pollution and greenness with offspring asthma and hay fever. Int J Environ Res Public Health. 2020;17(16).
Wang J, Lu M, An Z, Jiang J, Li J, Wang Y, et al. Associations between air pollution and outpatient visits for allergic rhinitis in **nxiang, China. Environ Sci Pollut Res Int. 2020;27(19):23565–74.
Hao S, Yuan F, Pang P, Yang B, Jiang X, Yan A. Early childhood traffic-related air pollution and risk of allergic rhinitis at 2–4 years of age modification by family stress and male gender: a case-control study in Shenyang, China. Environ Health Prev Med. 2021;26(1):48.
Guo M, Wei L, Yan H, Duan Z, Niu Z, **ao C. Exposure to ambient air pollution during trimesters of pregnancy and childhood allergic diseases in Wuhan, China. Int J Environ Health Res. 2021:1–11.
Liu Y, Lu C, Li Y, Norbäck D, Deng Q. Outdoor air pollution and indoor window condensation associated with childhood symptoms of allergic rhinitis to pollen. Int J Environ Res Public Health. 2022;19(13).
Wu R, Guo Q, Fan J, Guo C, Wang G, Wu W, et al. Association between air pollution and outpatient visits for allergic rhinitis: effect modification by ambient temperature and relative humidity. Sci Total Environ. 2022;821:152960.
Hartig T, Mitchell R, de Vries S, Frumkin H. Nature and health. Annu Rev Public Health. 2014;35:207–28.
Li L, Hart JE, Coull BA, Cao SJ, Spengler JD, Adamkiewicz G. Effect of residential greenness and nearby parks on respiratory and allergic diseases among middle school adolescents in a Chinese city. Int J Environ Res Public Health. 2019;16(6).
Gernes R, Brokamp C, Rice GE, Wright JM, Kondo MC, Michael YL, et al. Using high-resolution residential greenspace measures in an urban environment to assess risks of allergy outcomes in children. Sci Total Environ. 2019;668:760–7.
Lambert KA, Katelaris C, Burton P, Cowie C, Lodge C, Garden FL, et al. Tree pollen exposure is associated with reduced lung function in children. Clin Exp Allergy. 2020;50(10):1176–83.
•• Peters RL, Sutherland D, Dharmage SC, Lowe AJ, Perrett KP, Tang MLK, et al. The association between environmental greenness and the risk of food allergy: a population-based study in Melbourne, Australia. Pediatr Allergy Immun. 2022;33(2):e13749. COMMENT: First study to look at the association between greenness and FA.
Haahtela T. A biodiversity hypothesis. Allergy. 2019;74(8):1445–56.
Caynes RJC, Mitchell MGE, Wu DS, Johansen K, Rhodes JR. Using high-resolution LiDAR data to quantify the three-dimensional structure of vegetation in urban green space. Urban Ecosyst. 2016;19(4):1749–65.
Song J-H, Han S-H, Yu K, Kim Y-I. Assessing the possibility of land-cover classification using lidar intensity data. Int Arch Photogramm Remote Sens Spat Inf Sci. 2012;34.
Kwak DA, Lee WK, Kafatos M, Son Y, Cho HK, Lee SH. Estimation of effective plant area index for South Korean forests using LiDAR system. Sci China Life Sci. 2010;53(7):898–908.
Parmes E, Pesce G, Sabel CE, Baldacci S, Bono R, Brescianini S, et al. Influence of residential land cover on childhood allergic and respiratory symptoms and diseases: evidence from 9 European cohorts. Environ Res. 2020;183:108953.
Lambert KA, Bowatte G, Tham R, Lodge CJ, Prendergast LA, Heinrich J, et al. Greenspace and atopic sensitization in children and adolescents-a systematic review. Int J Environ Res Public Health. 2018;15(11).
Markevych I, Ludwig R, Baumbach C, Standl M, Heinrich J, Herberth G, et al. Residing near allergenic trees can increase risk of allergies later in life: LISA Leipzig study. Environ Res. 2020;191:110132.
Bublin M, Breiteneder H. Cross-reactivity of peanut allergens. Curr Allergy Asthma Rep. 2014;14(4):426.
Seo SC, Park SJ, Park CW, Yoon WS, Choung JT, Yoo Y. Clinical and immunological effects of a forest trip in children with asthma and atopic dermatitis. Iran J Allergy Asthma Immunol. 2015;14(1):28–36.
Lee JY, Lamichhane DK, Lee M, Ye S, Kwon JH, Park MS, et al. Preventive effect of residential green space on infantile atopic dermatitis associated with prenatal air pollution exposure. Int J Environ Res Public Health. 2018;15(1).
Dzhambov AM, Lercher P, Rüdisser J, Browning M, Markevych I. Allergic symptoms in association with naturalness, greenness, and greyness: a cross-sectional study in schoolchildren in the Alps. Environ Res. 2021;198:110456.
Riedler J, Braun-Fahrländer C, Eder W, Schreuer M, Waser M, Maisch S, et al. Exposure to farming in early life and development of asthma and allergy: a cross-sectional survey. Lancet (London, England). 2001;358(9288):1129–33.
Alfvén T, Braun-Fahrländer C, Brunekreef B, von Mutius E, Riedler J, Scheynius A, et al. Allergic diseases and atopic sensitization in children related to farming and anthroposophic lifestyle–the PARSIFAL study. Allergy. 2006;61(4):414–21.
Illi S, Depner M, Genuneit J, Horak E, Loss G, Strunz-Lehner C, et al. Protection from childhood asthma and allergy in Alpine farm environments-the GABRIEL advanced studies. J Allergy Clin Immunol. 2012;129(6):1470-7.e6.
Holbreich M, Genuneit J, Weber J, Braun-Fahrländer C, Waser M, von Mutius E. Amish children living in northern Indiana have a very low prevalence of allergic sensitization. J Allergy Clin Immunol. 2012;129(6):1671–3.
Stein MM, Hrusch CL, Gozdz J, Igartua C, Pivniouk V, Murray SE, et al. Innate immunity and asthma risk in Amish and Hutterite farm children. N Engl J Med. 2016;375(5):411–21.
Botha M, Basera W, Facey-Thomas HE, Gaunt B, Gray CL, Ramjith J, et al. Rural and urban food allergy prevalence from the South African Food Allergy (SAFFA) study. J Allergy Clin Immunol. 2019;143(2):662-8.e2.
Botha M, Basera W, Facey-Thomas HE, Gaunt B, Genuneit J, Gray CL, et al. Nutrition and allergic diseases in urban and rural communities from the South African Food Allergy cohort. Pediatr Allergy Immunol. 2019;30(5):511–21.
Levin ME, Botha M, Basera W, Facey-Thomas HE, Gaunt B, Gray CL, et al. Environmental factors associated with allergy in urban and rural children from the South African Food Allergy (SAFFA) cohort. J Allergy Clin Immunol. 2020;145(1):415–26.
•• Lehtimäki J, Thorsen J, Rasmussen MA, Hjelmsø M, Shah S, Mortensen MS, et al. Urbanized microbiota in infants, immune constitution, and later risk of atopic diseases. J Allergy Clin Immunol. 2021;148(1):234–43. COMMENT: A study of early life rural exposure on infant microbiome and childhood atopic outcomes.
Martina C, Looney RJ, Marcus C, Allen M, Stahlhut R. Prevalence of allergic disease in Old Order Mennonites in New York. Ann Allergy Asthma Immunology. 2016;117(5):562-3.e1.
Phillips JT, Stahlhut RW, Looney RJ, Järvinen KM. Food allergy, breastfeeding, and introduction of complementary foods in the New York Old Order Mennonite Community. Ann Allergy Asthma Immunol. 2020;124(3):292-4.e2.
Järvinen KM, Davis EC, Bevec E, Jackson CM, Pizzarello C, Catlin E, et al. Biomarkers of development of immunity and allergic diseases in farming and non-farming lifestyle infants: design, methods and 1 year outcomes in the “Zooming in to Old Order Mennonites” birth cohort study. Front Pediatr. 2022;10.
Ege MJ, Bieli C, Frei R, van Strien RT, Riedler J, Ublagger E, et al. Prenatal farm exposure is related to the expression of receptors of the innate immunity and to atopic sensitization in school-age children. J Allergy Clin Immunol. 2006;117(4):817–23.
Pfefferle PI, Büchele G, Blümer N, Roponen M, Ege MJ, Krauss-Etschmann S, et al. Cord blood cytokines are modulated by maternal farming activities and consumption of farm dairy products during pregnancy: the PASTURE Study. J Allergy Clin Immunol. 2010;125(1):108-15.e1-3.
Douwes J, Cheng S, Travier N, Cohet C, Niesink A, McKenzie J, et al. Farm exposure in utero may protect against asthma, hay fever and eczema. Eur Respir J. 2008;32(3):603–11.
Horak E, Morass B, Ulmer H, Genuneit J, Braun-Fahrländer C, von Mutius E. Prevalence of wheezing and atopic diseases in Austrian schoolchildren in conjunction with urban, rural or farm residence. Wien Klin Wochenschr. 2014;126(17–18):532–6.
Braun-Fahrländer C, Gassner M, Grize L, Neu U, Sennhauser FH, Varonier HS, et al. Prevalence of hay fever and allergic sensitization in farmer’s children and their peers living in the same rural community. SCARPOL team. Swiss Study on Childhood Allergy and Respiratory Symptoms with Respect to Air Pollution. Clin Exp Allergy. 1999;29(1):28–34.
•• Steiman CA, Evans MD, Lee KE, Lasarev MR, Gangnon RE, Olson BF, et al. Patterns of farm exposure are associated with reduced incidence of atopic dermatitis in early life. J Allergy Clin Immunol. 2020;146(6):1379–86.e6. COMMENT: First study demostrating farm-life protection against AD in America.
Tong H, Gao L, Deng Y, Kong Y, **ang R, Tan L, et al. Prevalence of allergic rhinitis and associated risk factors in 6 to 12 years schoolchildren from Wuhan in central China: a cross-sectional study. Am J Rhinol Allergy. 2020;34(5):632–41.
Tong X, Tong H, Gao L, Deng Y, **ang R, Cen R, et al. A multicenter study of prevalence and risk factors for allergic rhinitis in primary school children in 5 cities of Hubei Province, China. Int Arch Allergy Immunol. 2022;183(1):34–44.
• Strieker S, Weinmann T, Gerlich J, von Mutius E, Nowak D, Radon K, et al. Farm living and allergic rhinitis from childhood to young adulthood - prospective results of the GABRIEL study. J Allergy Clin Immunol. 2022. COMMENT: Demostrated a role for farm exposure in childhood is protective against childhood and young adult AR.
Loss G, Apprich S, Waser M, Kneifel W, Genuneit J, Büchele G, et al. The protective effect of farm milk consumption on childhood asthma and atopy: the GABRIELA study. J Allergy Clin Immunol. 2011;128(4):766-73.e4.
von Mutius E, Vercelli D. Farm living: effects on childhood asthma and allergy. Nat Rev Immunol. 2010;10(12):861–8.
Broussard JL, Devkota S. The changing microbial landscape of Western society: Diet, dwellings and discordance. Mol Metab. 2016;5(9):737–42.
Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364(8):701–9.
Trikamjee T, Basera W, Botha M, Facey-Thomas HE, Gaunt B, Genuneit J, et al. Associations between environmental dust composition and atopic dermatitis in urban and rural settings. Pediatr Allergy Immunol. 2021;32(5):1013–21.
Mahdavinia M, Greenfield LR, Moore D, Botha M, Engen P, Gray C, et al. House dust microbiota and atopic dermatitis; effect of urbanization. Pediatr Allergy Immunol. 2021;32(5):1006–12.
Chen CC, Chen KJ, Kong MS, Chang HJ, Huang JL. Alterations in the gut microbiotas of children with food sensitization in early life. Pediatr Allergy Immunol. 2016;27(3):254–62.
Penders J, Thijs C, van den Brandt PA, Kummeling I, Snijders B, Stelma F, et al. Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut. 2007;56(5):661–7.
Bisgaard H, Li N, Bonnelykke K, Chawes BL, Skov T, Paludan-Müller G, et al. Reduced diversity of the intestinal microbiota during infancy is associated with increased risk of allergic disease at school age. J Allergy Clin Immunol. 2011;128(3):646-52.e1-5.
Depner M, Taft DH, Kirjavainen PV, Kalanetra KM, Karvonen AM, Peschel S, et al. Maturation of the gut microbiome during the first year of life contributes to the protective farm effect on childhood asthma. Nat Med. 2020;26(11):1766–75.
Seppo AE, Bu K, Jumabaeva M, Thakar J, Choudhury RA, Yonemitsu C, et al. Infant gut microbiome is enriched with Bifidobacterium longum ssp. infantis in Old Order Mennonites with traditional farming lifestyle. Allergy. 2021;76(11):3489–503.
Henrick BM, Hutton AA, Palumbo MC, Casaburi G, Mitchell RD, Underwood MA, et al. Elevated Fecal pH Indicates a profound change in the breastfed infant gut microbiome due to reduction of bifidobacterium over the past century. mSphere. 2018;3(2).
Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, et al. Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Nat Med. 2016;22(10):1187–91.
Henrick BM, Rodriguez L, Lakshmikanth T, Pou C, Henckel E, Arzoomand A, et al. Bifidobacteria-mediated immune system imprinting early in life. Cell. 2021;184(15):3884-98.e11.
Schuijs MJ, Willart MA, Vergote K, Gras D, Deswarte K, Ege MJ, et al. Farm dust and endotoxin protect against allergy through A20 induction in lung epithelial cells. Science (New York, NY). 2015;349(6252):1106–10.
Lluis A, Depner M, Gaugler B, Saas P, Casaca VI, Raedler D, et al. Increased regulatory T-cell numbers are associated with farm milk exposure and lower atopic sensitization and asthma in childhood. J Allergy Clin Immunol. 2014;133(2):551–9.
Schaub B, Liu J, Höppler S, Schleich I, Huehn J, Olek S, et al. Maternal farm exposure modulates neonatal immune mechanisms through regulatory T cells. J Allergy Clin Immunol. 2009;123(4):774-82.e5.
Lundell AC, Hesselmar B, Nordström I, Adlerberth I, Wold AE, Rudin A. Higher B-cell activating factor levels at birth are positively associated with maternal dairy farm exposure and negatively related to allergy development. J Allergy Clin Immunol. 2015;136(4):1074-82.e3.
Strömbeck A, Nordström I, Andersson K, Andersson H, Johansen S, Maglio C, et al. Allergic disease in 8-year-old children is preceded by delayed B cell maturation. Clin Exp Allergy. 2017;47(7):918–28.
Abbring S, Hols G, Garssen J, van Esch B. Raw cow’s milk consumption and allergic diseases - the potential role of bioactive whey proteins. Eur J Pharmacol. 2019;843:55–65.
Abbring S, Ryan JT, Diks MAP, Hols G, Garssen J, van Esch B. Suppression of food allergic symptoms by raw cow's milk in mice is retained after skimming but abolished after heating the milk-a promising contribution of alkaline phosphatase. Nutrients. 2019;11(7).
Abbring S, Blokhuis BRJ, Miltenburg JL, Olmedo K, Garssen J, Redegeld FA, et al. Direct inhibition of the allergic effector response by raw cow's milk-an extensive in vitro assessment. Cells. 2020;9(5).
Abbring S, Kusche D, Roos TC, Diks MAP, Hols G, Garssen J, et al. Milk processing increases the allergenicity of cow’s milk-preclinical evidence supported by a human proof-of-concept provocation pilot. Clin Exp Allergy. 2019;49(7):1013–25.
Wild CP. The exposome: from concept to utility. Int J Epidemiol. 2012;41(1):24–32.
Moran TP. The external exposome and food allergy. Curr Allergy Asthma Rep. 2020;20(8):37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Courtney M. Jackson reports grants from NIH, outside the submitted work; Alexandra N. Kaplan no conflict of interest. Kirsi M. Jarvinen reports grants from NIH, grants from Janssen R&D, grants from Bill and Melinda Gates Foundation, personal fees from DBV, personal fees from Janssen R&D, grants from Aimmune, personal fees from Up-To-Date, personal fees from Jovie, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jackson, C.M., Kaplan, A.N. & Järvinen, K.M. Environmental Exposures may Hold the Key; Impact of Air Pollution, Greenness, and Rural/Farm Lifestyle on Allergic Outcomes. Curr Allergy Asthma Rep 23, 77–91 (2023). https://doi.org/10.1007/s11882-022-01061-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-022-01061-y