Abstract
Background
Intracranial hemorrhages is one of the major causes of mortality and morbidity worldwide, and there is still no effective biomarker to predict prognosis.
Aim
We aimed to determine the effectiveness of high sensitive troponin I (hs-cTn-I) levels to predict the prognosis of spontaneous intracerebral hemorrhage (sICH) by comparing Glasgow Coma Score (GCS) and hematoma volume with hs-cTn-I levels.
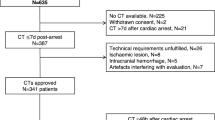
Methods
This study was planned as a retrospective observational study. Patients with available data, over 18 years old and sICH were included in the study. Cerebral computed tomography images were evaluated by a senior radiologist. Hematoma volume was calculated using the ABC/2 formula.
Results
The study comprised 206 individuals in total 78 (37.86%) women and 128 (62.13%) men. Forty-four (21.35%) of patients died. The sensitivity of GCS, hs-cTn-I, and hematoma volume values were 86.36%, 66.67%, and 59.46%, respectively, with corresponding specificities of 78.75%, 93.02%, and 87.58%. Patients with hs-cTn-I values over 26, GCS values of ≤ 9, and hematoma volume values above 44.16 were found to have higher risk of mortality (p = 0.011; p < 0.001; p < 0.001, respectively). The mortality rates were found to be increased 2.586 (IQR: 1.224–5.463) times in patients with hs-cTn-I values above 26, 0.045 times (IQR: 0.018–0.115) in patients with GCS values ≤ 9, and 7.526 times (IQR: 3.518–16.100) in patients with hematoma volume values above 44.16.
Conclusions
Our findings suggest that hs-cTn-I values exceeding 26 units may serve as effective biochemical markers for predicting the prognosis of patients with sICH.
Similar content being viewed by others
Data availability
Data and materials are reachable from hospital automation information systems.
References
WHO The top 10 causes of death. 9 December 2020. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Van Asch CJ, Luitse MJ, Rinkel GJ et al (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 9:167–176. https://doi.org/10.1016/S1474-4422(09)70340-0
Tsao CW, Aday AW, Almarzooq ZI and others (2022) Heart disease and stroke statistics–2022 update: a report From the American Heart Association. Circulation 145:e153–e639. https://doi.org/10.1161/CIR.0000000000001052
Garg P, Morris P, Fazlanie AL and others (2017) Cardiac biomarkers of acute coronary syndrome: from history to high-sensitivity cardiac troponin. Intern Emerg Med 12(2):147–155. https://doi.org/10.1007/s11739-017-1612-1
Latini R, Masson S, Anand IS and others (2007) Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 116(11):1242–1249. https://doi.org/10.1161/CIRCULATIONAHA.106.655076
Rosjo H, Varpula M, Hagve TA and others (2011) Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive Care Med 37(1):77–85. https://doi.org/10.1007/s00134-010-2051-x
Aksu A, Avci A, Yolcu S and others (2023) The relationship between infarct volume and high sensitivity troponin I level in patients diagnosed with ischemic stroke. Ir J Med Sci 192(2):901–906. https://doi.org/10.1007/s11845-022-03048-0
Palma JA, Benarroch EE (2014) Neural control of the heart: recent concepts and clinical correlations. Neurology 83:261–271. https://doi.org/10.1212/WNL.0000000000000605
Beissner F, Meissner K, Bar KJ, Napadow V (2013) The autonomic brain: an activation likelihood estimation meta-analysis for central processing of autonomic function. J Neurosci 33:10503–10511. https://doi.org/10.1523/JNEUROSCI.1103-13.2013
Pinho J, Costa AS, Araujo JM et al (2019) Intracerebral hemorrhage outcome: A comprehensive update. J Neurol Sci 398:54–66. https://doi.org/10.1016/j.jns.2019.01.013
Trifan G, Testai FD (2020) Systemic Immune-Inflammation (SII) index predicts poor outcome after spontaneous supratentorial intracerebral hemorrhage. J Stroke Cerebrovasc Dis 29(9):105057. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105057
Greenberg SM, Ziai WC, Cordonnier C and others (2022) Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke 53:00–00. https://doi.org/10.1161/STR.0000000000000407
Ariesen MJ, Claus SP, Rinkel GJE, Algra A (2003) Risk factors for intracerebral hemorrhage in the general population: A systematic review. Stroke 34(8):2060–2065. https://doi.org/10.1161/01.STR.0000080678.09344.8D
Celikbilek A, Goksel BK, Zararsiz G, Benli S (2013) Spontaneous intra-cerebral hemorrhage: A retrospective study of risk factors and outcome in a Turkish population. J Neurosci Rural Pract 40(03):271–277. https://doi.org/10.4103/0976-3147.118770
Bernardo F, Rebordao L, Machado S et al (2019) In-hospital and long-term prognosis after spontaneous intracerebral hemorrhage among young adults aged 18–65 years. J Stroke Cerebrovasc Dis: Off J Nat Stroke Assoc 28(11):104350. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104350
Aydın IE, Yıldırım Ç, Savrun ST et al (2021) The Effect of Hemorrhage Volume on Mortality in Spontaneous Intracerebral Hemorrhages. Van Tıp Derg 28(3):389–392. https://doi.org/10.5505/vtd.2021.81084
Biffi A, Battey TW, Ayres AM and others (2011) Warfarin-related intraventricular hemorrhage: imaging and outcome. Neurology 77:1840–1846. https://doi.org/10.1212/WNL.0b013e3182377e12
Lee SH, Ryu WS, Roh JK (2009) Cerebral microbleeds are a risk factor for warfarin-related intracerebral hemorrhage. Neurology 72:171–176. https://doi.org/10.1212/01.wnl.0000339060.11702.dd
Lovelock CE, Cordonnier C, Naka H and others (2010) Edinburgh Stroke Study Group. Antithrombotic drug use, cerebral microbleeds, and intracerebral hemorrhage: a systematic review of published and unpublished studies. Stroke 41:1222–1228. https://doi.org/10.1161/STROKEAHA.109.572594
Zubkov AY, Mandrekar JN, Claassen DO et al (2008) Predictors of outcome in warfarin-related intracerebral hemorrhage. Arch Neurol 65:1320–1325. https://doi.org/10.1001/archneur.65.10.1320
Delcourt C, Sato S, Zhang S and others (2017) Intracerebral hemorrhage location and outcome among INTERACT2 participants. Neurology 88(15):1408–1414. https://doi.org/10.1212/WNL.0000000000003771
Takeuchi S, Wada K, Nagatani K et al (2013) Decompressive hemicraniectomy for spontaneous intracerebral hemorrhage. Neurosurg Focus 34(5):E5. https://doi.org/10.3171/2013.2.FOCUS12424
Al-Khaled M, Awwad S, Bruning T (2020) Nontraumatic spontaneous intracerebral hemorrhage: Baseline characteristics and early outcomes. Brain Behav 10(1):e01512. https://doi.org/10.1002/brb3.1512
Muresan EM, Golea A, Vesa SC et al (2022) Admission emergency department point-of-care biomarkers for prediction of early mortality in spontaneous ıntracerebral hemorrhage. In Vivo 36:1534–1543. https://doi.org/10.21873/invivo.12864
Hegde A, Menon G (2018) Modifying the intracerebral hemorrhage score to suit the needs of the develo** world. Ann Indian Acad Neurol 21(4):270–274. https://doi.org/10.4103/aian.AIAN_419_17
Dolgun H, Hanalioglu S, Gurses L et al (2020) Surgical treatment of spontaneous ıntracerebral hematomas. ACU Sağlık Bil Derg 11(3):439–446. https://doi.org/10.31067/0.2020.293
Ironside N, Chen CJ, Dreyer V et al (2020) Location-specific differences in hematoma volume predict outcomes in patients with spontaneous intracerebral hemorrhage. Int J Stroke 15(1):90–102. https://doi.org/10.1177/1747493019830589
Bhatia R, Singh H, Singh S and others (2013) A prospective study of in-hospital mortality and discharge outcome in spontaneous intracerebral hemorrhage. Neurol India 61(3):244–248. https://doi.org/10.4103/0028-3886.115062
Qin G, Dai C, Feng S, Wu G (2022) Changes of electrocardiogram and myocardial enzymes in patients with ıntracerebral hemorrhage. Hindawi Dis Markers 9309444. https://doi.org/10.1155/2022/9309444
Cheung RTF, Zou LY (2003) Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke 34(7):1717–1722. https://doi.org/10.1161/01.STR.0000078657.22835.B9
Hemphill JC 3rd, Bonovich DC, Besmertis L et al (2001) The ICH score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke 32:891–897. https://doi.org/10.1161/01.str.32.4.891
Broderick JP, Brott TG, Duldner JE et al (1993) Volume of intracerebral hemorrhage: A powerful and easy-to-use predictor of 30-day mortality. Stroke 24(7):987–993. https://doi.org/10.1161/01.str.24.7.987
Garrett MC, Komotar RJ, Starke RM et al (2010) Elevated troponin levels are predictive of mortality in surgical intracerebral hemorrhage patients. Neurocrit Care 12:199–203. https://doi.org/10.1007/s12028-009-9245-5
He Y, Liu Q, Wang J et al (2020) Prognostic value of elevated cardiac troponin I in patients with intracerebral hemorrhage. Clin Cardiol 43:338–345. https://doi.org/10.1002/clc.23320
Alkhachroum AM, Miller B, Chami T et al (2019) A troponin study on patients with ischemic stroke, intracerebral hemorrhage and subarachnoid hemorrhage: Type II myocardial infarction is significantly associated with stroke severity, discharge disposition and mortality. J Clin Neurosci 64:83–88. https://doi.org/10.1016/j.jocn.2019.04.005
Acknowledgements
There is no person, instution or company to acknowledgement.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Dr. Ulger Huseyin, Dr. Icme Ferhat, Dr. Avci Akkan, Dr. Avci Begum Seyda and Dr Parlatan Cenk: conceptualization, methodology, investigation, and writing – original draft. Dr. Icme Ferhat, Dr. Avci Akkan and Dr. Aksay Erdem: resources, formal analysis, and writing – review and editing. Dr. Icme Ferhat, Dr. Ulger Huseyin: conceptualization, methodology, and writing – review and editing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The ethics committee of the Adana City Training and Research Hospital approved the study.
The study was performed according to the recommendations set by the The Declaration of Helsinki on Medical Research involving Human Subjects.
Informed consent
Written informed consent was not necessary because no patient data has been included in the manuscript.
Conflict of interest
The authors have no conflicts of interests to declare.
Human rights
This manuscript was carried out in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Any part of this paper is not under consideration for publishing or published in anywhere else.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ulger, H., Icme, F., Parlatan, C. et al. Prognostic relationship between high sensitivity troponin I level, hematoma volume and glasgow coma score in patients diagnosed with spontaneous intracerebral hemorrhage. Ir J Med Sci (2024). https://doi.org/10.1007/s11845-024-03737-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11845-024-03737-y