Abstract
Purpose
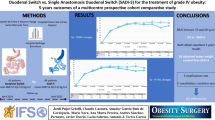
The literature on long-term outcomes of duodenal switch (DS) compared to single anastomosis duodenal switch (SADI-S) procedures is lacking. We evaluated the long-term outcomes of SADI-S compared to those after the classic DS procedure.
Methods
This is a follow-up report from a single-institution prospective cohort study comparing long-term outcomes of SADI-S versus DS both as one- and two-stage procedures (ClinicalTrials.gov: NCT02792166). Data is depicted as count (percentage) or median (interquartile range).
Results
Forty-two patients underwent SADI-S, of whom 11 had it as a second-stage procedure (26%). Of 20 patients who underwent DS, twelve had it as a second-stage procedure (60%). Both groups were similar at baseline. Median follow-up times for one-stage SADI-S and DS were 57 (24) and 57 (9) months, respectively (p = 0.93). Similar BMI reductions were observed after one-stage SADI-S (16.5 kg/m2 [8.5]) and DS (18.9 kg/m2 [7.2]; p = 0.42). At median follow-up of 51 (21) and 60 (15) months after second-stage SADI-S and DS, respectively (p = 0.60), surgical procedures yielded reductions in BMI of 20.5 kg/m2 (14.0) and 24.0 kg/m2 (13.9), respectively (p = 0.52). Follow-up rates were similar for one-stage (≥ 88%; p = 0.29) and second-stage procedures (≥ 83%; p = 0.16). Similar diabetes and hypertension remissions were found (p = 0.77; P = 0.54, respectively). Despite fat-soluble vitamin deficiencies at baseline, after supplementation, they were either eliminated or less prevalent long-term after SADI-S. Daily bowel movements were also less frequent.
Conclusions
Long-term weight and comorbidity outcomes after SADI-S are similar to those of DS both as one- and two-stage surgeries. SADI-S procedure may allow for similar beneficial outcomes with less burden from gastrointestinal symptoms and fat-soluble vitamin deficiencies.
Graphical Abstract



Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Hedberg J, Sundstrom J, Sundbom M. Duodenal switch versus Roux-en-Y gastric bypass for morbid obesity: systematic review and meta-analysis of weight results, diabetes resolution and early complications in single-centre comparisons. Obes Rev. 2014;15:555–63.
Strain GW, Torghabeh MH, Gagner M, Ebel F, Dakin GF, Abelson JS, et al. The Impact of Biliopancreatic Diversion with Duodenal Switch (BPD/DS) Over 9 Years. Obes Surg. 2017;27:787–94.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641.
Marceau P, Biron S, Marceau S, Hould FS, Lebel S, Lescelleur O, et al. Long-Term Metabolic Outcomes 5 to 20 Years After Biliopancreatic Diversion. Obes Surg. 2015;25:1584–93.
Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;15:408–16.
Marceau P, Biron S, Hould FS, Lebel S, Marceau S, Lescelleur O, et al. Duodenal switch: long-term results. Obes Surg. 2007;17:1421–30.
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25:1822–32.
Newbury L, Dolan K, Hatzifotis M, Low N, Fielding G. Calcium and vitamin D depletion and elevated parathyroid hormone following biliopancreatic diversion. Obes Surg. 2003;13:893–5.
Aasheim ET, Bjorkman S, Sovik TT, Engstrom M, Hanvold SE, Mala T, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90:15–22.
Clapp B, Badaoui JN, Gamez JA, Vivar A, Ghanem OM. Reluctance in duodenal switch adoption: an international survey among bariatric surgeons. Surg Obes Relat Dis. 2021;17:1760–5.
Sanchez-Pernaute A, Rubio Herrera MA, Perez-Aguirre E, Garcia Perez JC, Cabrerizo L, Diez Valladares L, et al. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17:1614–8.
Regan JP, Inabnet WB, Gagner M, Pomp A. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003;13:861–4.
Sanchez-Pernaute A, Rubio MA, Conde M, Arrue E, Perez-Aguirre E, Torres A. Single-anastomosis duodenoileal bypass as a second step after sleeve gastrectomy. Surg Obes Relat Dis. 2015;11:351–5.
Sanchez-Pernaute A, Rubio MA, Cabrerizo L, Ramos-Levi A, Perez-Aguirre E, Torres A. Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) for obese diabetic patients. Surg Obes Relat Dis. 2015.
Surve A, Zaveri H, Cottam D, Belnap L, Cottam A, Cottam S. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13:415–22.
Finno P, Osorio J, Garcia-Ruiz-de-Gordejuela A, Casajoana A, Sorribas M, Admella V, et al. Single Versus Double-Anastomosis Duodenal Switch: Single-Site Comparative Cohort Study in 440 Consecutive Patients. Obes Surg. 2020;30:3309–16.
Yashkov Y, Bordan N, Torres A, Malykhina A, Bekuzarov D. SADI-S 250 vs Roux-en-Y Duodenal Switch (RY-DS): Results of 5-Year Observational Study. Obes Surg. 2021;31:570–9.
Pereira AM, Guimaraes M, Pereira SS, Ferreira de Almeida R, Monteiro MP, Nora M. Single and dual anastomosis duodenal switch for obesity treatment: a single-center experience. Surg Obes Relat Dis. 2021;17:12–9.
Gebelli JP, Lazzara C, de Gordejuela AGR, Nora M, Pereira AM, Sanchez-Pernaute A, et al. Duodenal Switch vs. Single-Anastomosis Duodenal Switch (SADI-S) for the Treatment of Grade IV Obesity: 5-Year Outcomes of a Multicenter Prospective Cohort Comparative Study. Obes Surg. 2022;32:3839–46.
Andalib A, Bouchard P, Alamri H, Bougie A, Demyttenaere S, Court O. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S): short-term outcomes from a prospective cohort study. Surg Obes Relat Dis. 2021;17:414–24.
Verhoeff K, Mocanu V, Zalasky A, Dang J, Kung JY, Switzer NJ, et al. Evaluation of Metabolic Outcomes Following SADI-S: a Systematic Review and Meta-analysis. Obes Surg. 2022;32:1049–63.
Sanchez-Pernaute A, Rubio MA, Perez Aguirre E, Barabash A, Cabrerizo L, Torres A. Single-anastomosis duodenoileal bypass with sleeve gastrectomy: metabolic improvement and weight loss in first 100 patients. Surg Obes Relat Dis. 2013;9:731–5.
Sanchez-Pernaute A, Herrera MA, Perez-Aguirre ME, Talavera P, Cabrerizo L, Matia P, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up Obes Surg. 2010;20:1720–6.
Clapp B, Wynn M, Martyn C, Foster C, O’Dell M, Tyroch A. Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis. 2018;14:741–7.
Muller TD, Bluher M, Tschop MH, DiMarchi RD. Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov. 2022;21:201–23.
Zorrilla-Nunez LF, Campbell A, Giambartolomei G, Lo Menzo E, Szomstein S, Rosenthal RJ. The importance of the biliopancreatic limb length in gastric bypass: A systematic review. Surg Obes Relat Dis. 2019;15:43–9.
Alsop BR, Sharma P. Esophageal Cancer. Gastroenterol Clin North Am. 2016;45:399–412.
Andalib A, Bouchard P, Demyttenaere S, Ferri LE, Court O. Esophageal cancer after sleeve gastrectomy: a population-based comparative cohort study. Surg Obes Relat Dis. 2021;17:879–87.
Bennett S, Gostimir M, Shorr R, Mallick R, Mamazza J, Neville A. The role of routine preoperative upper endoscopy in bariatric surgery: a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12:1116–25.
Bevilacqua LA, Obeid NR, Yang J, Zhu C, Altieri MS, Spaniolas K, et al. Incidence of GERD, esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma after bariatric surgery. Surg Obes Relat Dis. 2020;16:1828–36.
Brown WA, Johari Halim Shah Y, Balalis G, Bashir A, Ramos A, Kow L, et al. IFSO Position Statement on the Role of Esophago-Gastro-Duodenal Endoscopy Prior to and after Bariatric and Metabolic Surgery Procedures. Obes Surg. 2020;30:3135–53.
Campos GM, Mazzini GS, Altieri MS, Docimo S Jr, DeMaria EJ, Rogers AM, et al. ASMBS position statement on the rationale for performance of upper gastrointestinal endoscopy before and after metabolic and bariatric surgery. Surg Obes Relat Dis. 2021;17:837–47.
Surve A, Cottam D, Medlin W, Richards C, Belnap L, Horsley B, et al. Long-term outcomes of primary single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Surg Obes Relat Dis. 2020;16:1638–46.
Portela R, Marrerro K, Vahibe A, Galvani C, Billy H, Abu Dayyeh B, et al. Bile Reflux After Single Anastomosis Duodenal-Ileal Bypass with Sleeve (SADI-S): a Meta-analysis of 2,029 Patients. Obes Surg. 2022;32:1516–22.
Joret MO, Nanayakkara A, Kulasegaran S, Robertson J, Hammodat H. Duodenal Switch Combined with Systematic Post-operative Supplementation and Regular Patient Follow-up Results in Good Nutritional Outcomes. Obes Surg. 2022;32:1–11.
Rao R, Mehta M, Sheth DR, Hogan G. Four-Year Nutritional Outcomes in Single-Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy Patients: an Australian Experience. Obes Surg. 2023:1–11.
Funding
This work was supported by an unrestricted institutional award named Herbert S Lang Award in Oncology and Surgery provided to the corresponding author from the Research Institute of McGill University Health Center. The funding entity had no role in the design of the study, data collection, analysis, or interpretation of the results, writing of the manuscript or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In addition, the study was approved by the institutional Research Ethics Board.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points.
• At long-term follow-up, SADI-S (as either one- or two-stage procedure) is equally effective for weight loss as compared to classic DS.
• At long-term follow-up, SADI-S showed comparable resolution of weight-related comorbidities (especially for T2D) as compared to classic DS.
• SADI-S demonstrated fewer nutritional deficiencies (especially fat-soluble vitamins) and GI symptoms (daily bowel movements) as compared to classic DS.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andalib, A., Safar, A., Bouchard, P. et al. Single Anastomosis Duodenal Switch versus Classic Duodenal Switch: Long-term Outcomes from a Prospective Comparative Cohort Study. OBES SURG 33, 3951–3961 (2023). https://doi.org/10.1007/s11695-023-06900-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06900-z